Yonsei Med J.
2015 Mar;56(2):447-453. 10.3349/ymj.2015.56.2.447.
Risk Factors of Permanent Stomas in Patients with Rectal Cancer after Low Anterior Resection with Temporary Stomas
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jungwook.huh@gmail.com, seonghyeon.yun@samsung.com
- 2Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2070023
- DOI: http://doi.org/10.3349/ymj.2015.56.2.447
Abstract
- PURPOSE
The aim of this study was to identify risk factors influencing permanent stomas after low anterior resection with temporary stomas for rectal cancer.
MATERIALS AND METHODS
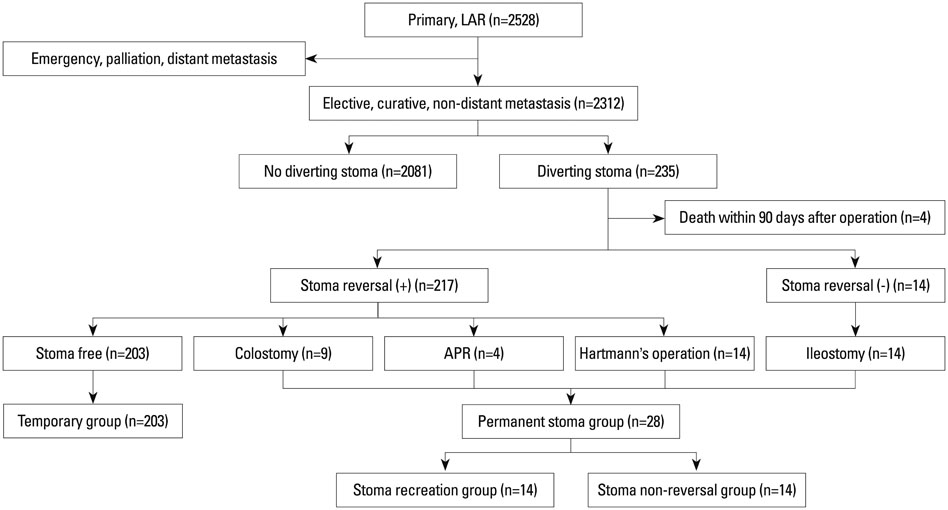
A total of 2528 consecutive rectal cancer patients who had undergone low anterior resection were retrospectively reviewed. Risk factors for permanent stomas were evaluated among these patients.
RESULTS
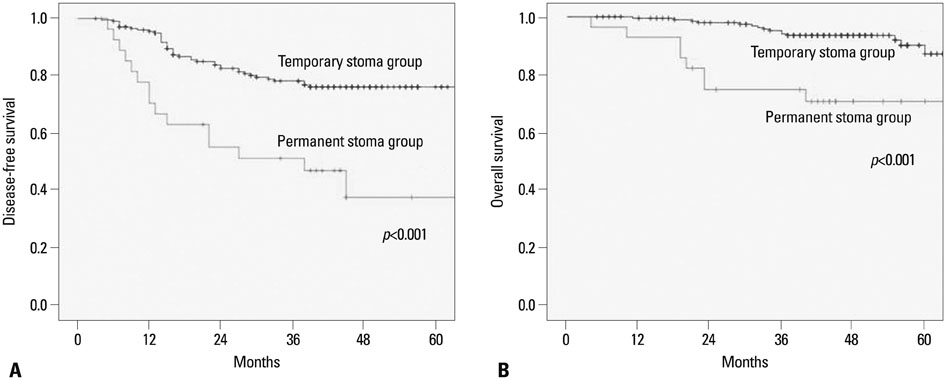
Among 2528 cases of rectal cancer, a total of 231 patients had a temporary diverting stoma. Among these cases, 217 (93.9%) received a stoma reversal. The median period between primary surgery and stoma reversal was 7.5 months. The temporary and permanent stoma groups consisted of 203 and 28 patients, respectively. Multivariate analysis showed that independent risk factors for permanent stomas were anastomotic-related complications (p=0.001) and local recurrence (p=0.001). The 5-year overall survival for the temporary and permanent stoma groups were 87.0% and 70.5%, respectively (p<0.001).
CONCLUSION
Rectal cancer patients who have temporary stomas after low anterior resection with local recurrence and anastomotic-related complications may be at increased risk for permanent stoma.
Keyword
MeSH Terms
-
Adenocarcinoma/pathology/*surgery
Adult
Aged
Aged, 80 and over
Female
Follow-Up Studies
Humans
Ileostomy/*statistics & numerical data
Incidence
Male
Middle Aged
Multivariate Analysis
Neoplasm Recurrence, Local
Postoperative Complications/epidemiology
Rectal Neoplasms/pathology/*surgery
Republic of Korea/epidemiology
Retrospective Studies
Risk Factors
Surgical Stomas/*statistics & numerical data
Treatment Outcome
Figure
Cited by 1 articles
-
Risk factors of stoma re-creation after closure of diverting ileostomy in patients with rectal cancer who underwent low anterior resection or intersphincteric resection with loop ileostomy
Ook Song, Kyung Hwan Kim, Soo Young Lee, Chang Hyun Kim, Young Jin Kim, Hyeong Rok Kim
Ann Surg Treat Res. 2018;94(4):203-208. doi: 10.4174/astr.2018.94.4.203.
Reference
-
1. Knight CD, Griffen FD. An improved technique for low anterior resection of the rectum using the EEA stapler. Surgery. 1980; 88:710–714.2. Heald RJ, Leicester RJ. The low stapled anastomosis. Br J Surg. 1981; 68:333–337.
Article3. Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986; 1:1479–1482.
Article4. Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–1740.
Article5. Matthiessen P, Hallböök O, Rutegård J, Sjödahl R. Population-based study of risk factors for postoperative death after anterior resection of the rectum. Br J Surg. 2006; 93:498–503.
Article6. Bokey EL, Chapuis PH, Hughes WJ, Koorey SG, Hinder JM, Edwards R. Morbidity, mortality and survival following resection for carcinoma of the rectum at Concord Hospital. Aust N Z J Surg. 1990; 60:253–259.
Article7. Tan WS, Tang CL, Shi L, Eu KW. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg. 2009; 96:462–472.
Article8. Pakkastie TE, Ovaska JT, Pekkala ES, Luukkonen PE, Järvinen HJ. A randomised study of colostomies in low colorectal anastomoses. Eur J Surg. 1997; 163:929–933.9. Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2007; 246:207–214.
Article10. Lindgren R, Hallböök O, Rutegård J, Sjödahl R, Matthiessen P. What is the risk for a permanent stoma after low anterior resection of the rectum for cancer? A six-year follow-up of a multicenter trial. Dis Colon Rectum. 2011; 54:41–47.
Article11. Nelson RS, Boland E, Ewing BM, Blatchford GJ, Ternent C, Shashidharan M, et al. Permanent diversion rates after neoadjuvant therapy and coloanal anastomosis for rectal cancer. Am J Surg. 2009; 198:765–770.
Article12. Hassan I, Larson DW, Wolff BG, Cima RR, Chua HK, Hahnloser D, et al. Impact of pelvic radiotherapy on morbidity and durability of sphincter preservation after coloanal anastomosis for rectal cancers. Dis Colon Rectum. 2008; 51:32–37.
Article13. Maggiori L, Bretagnol F, Lefèvre JH, Ferron M, Vicaut E, Panis Y. Conservative management is associated with a decreased risk of definitive stoma after anastomotic leakage complicating sphincter-saving resection for rectal cancer. Colorectal Dis. 2011; 13:632–637.
Article14. Mala T, Nesbakken A. Morbidity related to the use of a protective stoma in anterior resection for rectal cancer. Colorectal Dis. 2008; 10:785–788.
Article15. den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T, et al. A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol. 2007; 8:297–303.
Article16. Junginger T, Gönner U, Trinh TT, Lollert A, Oberholzer K, Berres M. Permanent stoma after low anterior resection for rectal cancer. Dis Colon Rectum. 2010; 53:1632–1639.
Article17. David GG, Slavin JP, Willmott S, Corless DJ, Khan AU, Selvasekar CR. Loop ileostomy following anterior resection: is it really temporary. Colorectal Dis. 2010; 12:428–432.18. Chun LJ, Haigh PI, Tam MS, Abbas MA. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. Dis Colon Rectum. 2012; 55:167–174.19. Seo SI, Yu CS, Kim GS, Lee JL, Yoon YS, Kim CW, et al. Characteristics and risk factors associated with permanent stomas after sphincter-saving resection for rectal cancer. World J Surg. 2013; 37:2490–2496.
Article20. Lim SW, Kim HJ, Kim CH, Huh JW, Kim YJ, Kim HR. Risk factors for permanent stoma after low anterior resection for rectal cancer. Langenbecks Arch Surg. 2013; 398:259–264.
Article21. Kairaluoma M, Rissanen H, Kultti V, Mecklin JP, Kellokumpu I. Outcome of temporary stomas. A prospective study of temporary intestinal stomas constructed between 1989 and 1996. Dig Surg. 2002; 19:45–51.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Psychological attitude to self-appraisal of stoma patients: prospective observation of stoma duration effect to self-appraisal
- The Relationship Between High-Output Stomas, Postoperative Ileus, and Readmission After Rectal Cancer Surgery With Diverting Ileostomy
- Long-term incidence of depression in rectal cancer patients with or without stoma: a population-based cohort study
- Comparative study between transanal tube and loop ileostomy in low anterior resection for mid rectal cancer: a retrospective single center trial
- Quality of Life After a Low Anterior Resection for Rectal Cancer in Elderly Patients