Ann Surg Treat Res.
2023 Jun;104(6):303-312. 10.4174/astr.2023.104.6.303.
Long-term incidence of depression in rectal cancer patients with or without stoma: a population-based cohort study
- Affiliations
-
- 1Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- 2Institute for Evidence-based Medicine, Cochrane Collaboration, Seoul, Korea
- 3Division of Colon and Rectal Surgery, Department of Surgery, Korea University Ansan Hospital, Ansan, Korea
- KMID: 2542794
- DOI: http://doi.org/10.4174/astr.2023.104.6.303
Abstract
- Purpose
Significant improvements have been made in the surgical treatment of rectal cancer with a higher sphinctersaving rate without compromising oncologic results. There have been studies about the quality of life of rectal cancer patients after surgery. However, no study has reported the long-term annual incidence of depression after rectal cancer surgery according to stoma status. The objective of this study was to determine the annual incidence of depression after rectal cancer surgery and the factors affecting it, especially the prevalence of depression according to the presence or duration of a stoma.
Methods
Using the Korea National Health Insurance Service database, patients who underwent radical surgery for rectal cancer from 2002 to 2019 were searched. We analyzed the incidence and risk factors of depression in patients who underwent radical surgery for rectal cancer according to stoma status.
Results
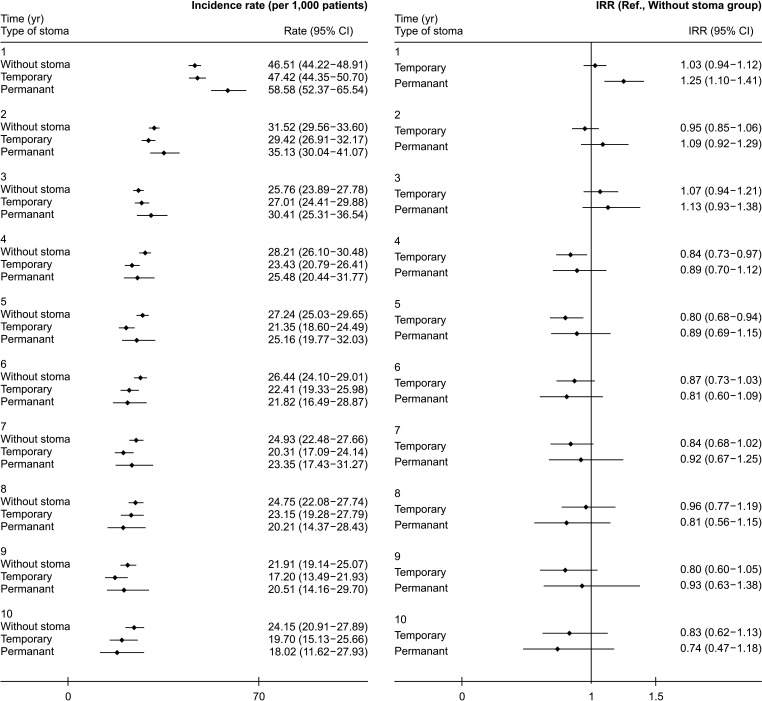
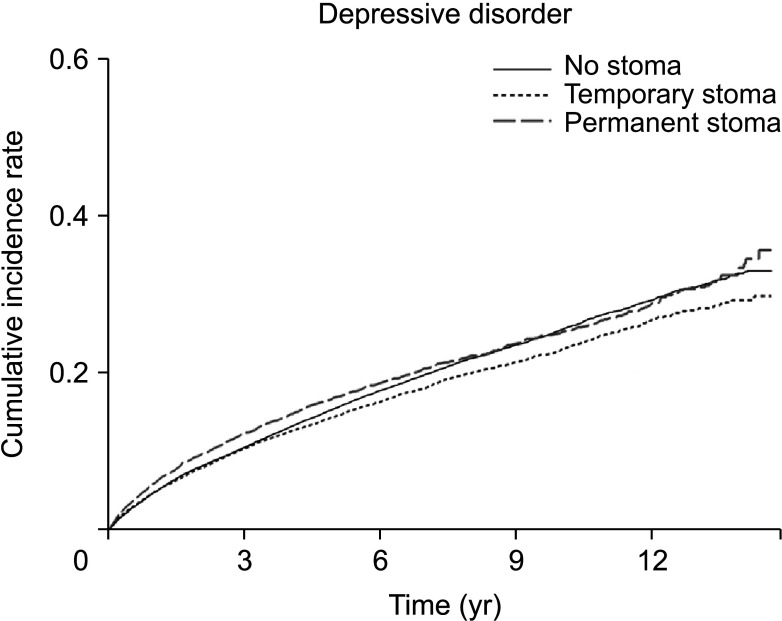
Annual incidence of depression in rectal cancer patients was decreasing annually for 15 years after surgery. There was no statistically significant difference in the incidence of depression according to the stoma status. However, the diagnosis of depression within 1 year after surgery was statistically significantly increased in the permanent stoma group.
Conclusion
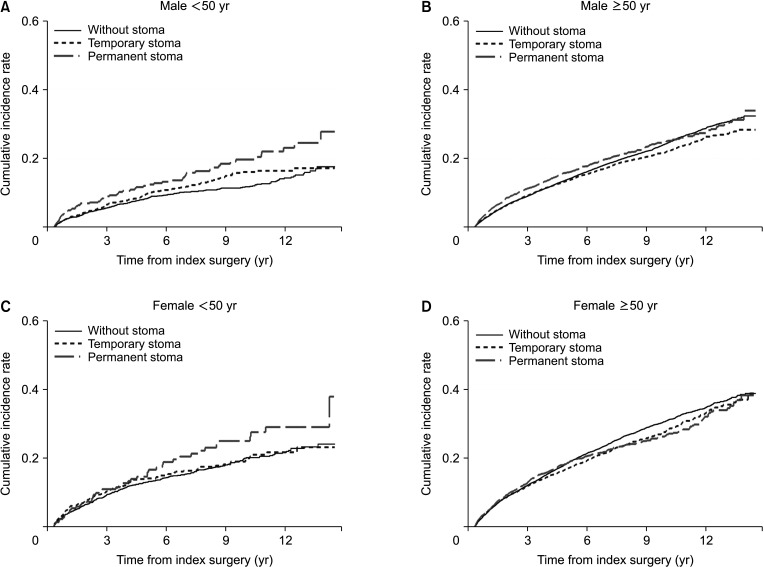
There was no difference in the overall incidence of depressive disorders among patients with rectal cancer based on their stoma status. However, a permanent stoma seems to increase the incidence in the first year after surgery. Education and intensive assessments of depressive disorders in patients with permanent stoma within 1 year after surgery are needed, particularly for female patients who are under 50 years old.
Keyword
Figure
Reference
-
1. Khil H, Kim SM, Hong S, Gil HM, Cheon E, Lee DH, et al. Time trends of colorectal cancer incidence and associated lifestyle factors in South Korea. Sci Rep. 2021; 11:2413. PMID: 33510236.2. Swedish Rectal Cancer Trial. Cedermark B, Dahlberg M, Glimelius B, Påhlman L, Rutqvist LE, et al. Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med. 1997; 336:980–987. PMID: 9091798.3. Weiser MR, Quah HM, Shia J, Guillem JG, Paty PB, Temple LK, et al. Sphincter preservation in low rectal cancer is facilitated by preoperative chemoradiation and intersphincteric dissection. Ann Surg. 2009; 249:236–242. PMID: 19212176.4. Chongpison Y, Hornbrook MC, Harris RB, Herrinton LJ, Gerald JK, Grant M, et al. Self-reported depression and perceived financial burden among long-term rectal cancer survivors. Psychooncology. 2016; 25:1350–1356. PMID: 26365584.5. Smith HR. Depression in cancer patients: pathogenesis, implications and treatment (Review). Oncol Lett. 2015; 9:1509–1514. PMID: 25788991.6. Follick MJ, Smith TW, Turk DC. Psychosocial adjustment following ostomy. Health Psychol. 1984; 3:505–517. PMID: 6536500.7. Clark M, Chur-Hansen A, Mikocka-Walus A. Systematic review with meta-analysis: current and emerging models of preoperative psychological preparation for individuals undergoing stoma surgery. J Psychosom Res. 2023; 168:111211. PMID: 36898315.8. Hong KS, Oh BY, Kim EJ, Chung SS, Kim KH, Lee RA. Psychological attitude to self-appraisal of stoma patients: prospective observation of stoma duration effect to self-appraisal. Ann Surg Treat Res. 2014; 86:152–160. PMID: 24761424.9. Emmertsen KJ, Laurberg S. Rectal Cancer Function Study Group. Impact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancer. Br J Surg. 2013; 100:1377–1387. PMID: 23939851.10. Kang SB, Cho JR, Jeong SY, Oh JH, Ahn S, Choi S, et al. Quality of life after sphincter preservation surgery or abdominoperineal resection for low rectal cancer (ASPIRE): a long-term prospective, multicentre, cohort study. Lancet Reg Health West Pac. 2020; 6:100087. PMID: 34327411.11. Pachler J, Wille-Jørgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev. 2012; 12:CD004323. PMID: 23235607.12. Näsvall P, Dahlstrand U, Löwenmark T, Rutegård J, Gunnarsson U, Strigård K. Quality of life in patients with a permanent stoma after rectal cancer surgery. Qual Life Res. 2017; 26:55–64. PMID: 27444778.13. Walming S, Asplund D, Bock D, Gonzalez E, Rosenberg J, Smedh K, et al. Quality of life in patients with resectable rectal cancer during the first 24 months following diagnosis. Colorectal Dis. 2020; 22:2028–2037. PMID: 32871612.14. Song L, Han X, Zhang J, Tang L. Body image mediates the effect of stoma status on psychological distress and quality of life in patients with colorectal cancer. Psychooncology. 2020; 29:796–802. PMID: 32043668.15. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800. PMID: 27794523.16. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728. PMID: 28378543.17. Proudman D, Greenberg P, Nellesen D. The growing burden of major depressive disorders (MDD): implications for researchers and policy makers. Pharmacoeconomics. 2021; 39:619–625. PMID: 34013439.18. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011; 9:90. PMID: 21791035.19. Kim GE, Jo MW, Shin YW. Increased prevalence of depression in South Korea from 2002 to 2013. Sci Rep. 2020; 10:16979. PMID: 33046758.20. Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos T, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med. 2013; 43:471–481. PMID: 22831756.21. Thorpe G, Arthur A, McArthur M. Adjusting to bodily change following stoma formation: a phenomenological study. Disabil Rehabil. 2016; 38:1791–1802. PMID: 26930444.22. Bekkers MJ, van Knippenberg FC, van Dulmen AM, van den Borne HW, van Berge Henegouwen GP. Survival and psychosocial adjustment to stoma surgery and nonstoma bowel resection: a 4-year follow-up. J Psychosom Res. 1997; 42:235–244. PMID: 9130180.23. Jansen L, Koch L, Brenner H, Arndt V. Quality of life among long-term (≥5 years) colorectal cancer survivors: systematic review. Eur J Cancer. 2010; 46:2879–2888. PMID: 20605090.24. Sprangers MA, Taal BG, Aaronson NK, te Velde A. Quality of life in colorectal cancer. Stoma vs. nonstoma patients. Dis Colon Rectum. 1995; 38:361–369. PMID: 7720441.25. Sandberg S, Asplund D, Bisgaard T, Bock D, González E, Karlsson L, et al. Low anterior resection syndrome in a Scandinavian population of patients with rectal cancer: a longitudinal follow-up within the QoLiRECT study. Colorectal Dis. 2020; 22:1367–1378. PMID: 32346917.26. Russell MM, Ganz PA, Lopa S, Yothers G, Ko CY, Arora A, et al. Comparative effectiveness of sphincter-sparing surgery versus abdominoperineal resection in rectal cancer: patient-reported outcomes in National Surgical Adjuvant Breast and Bowel Project randomized trial R-04. Ann Surg. 2015; 261:144–148. PMID: 24670844.27. Fioravanti M, Di Cesare F, Ramelli L, La Torre F, Nicastro A, Messinetti S, et al. Pre-surgery information and psychological adjustment to enterostomy. Ital J Surg Sci. 1988; 18:55–61. PMID: 3372216.28. Bernhard J, Lowy A, Mathys N, Herrmann R, Hürny C. Health related quality of life: a changing construct? Qual Life Res. 2004; 13:1187–1197. PMID: 15473497.29. Bernhard J, Hürny C, Maibach R, Herrmann R, Laffer U. Swiss Group for Clinical Cancer Research (SAKK). Quality of life as subjective experience: reframing of perception in patients with colon cancer undergoing radical resection with or without adjuvant chemotherapy. Ann Oncol. 1999; 10:775–782. PMID: 10470423.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quality of Life After a Low Anterior Resection for Rectal Cancer in Elderly Patients
- Benefits and risks of diverting stoma creation during rectal cancer surgery
- Metachronous carcinoma at the colostomy site after abdominoperineal resection of rectal cancer: a case report
- Loop Colostomy with Not Everted Fashion for Rectal Cancer
- Short-term and Medium-term Outcomes of Low Midline and Low Transverse Incisions in Laparoscopic Rectal Cancer Surgery