Korean J Radiol.
2015 Feb;16(1):160-168. 10.3348/kjr.2015.16.1.160.
MR Imaging Appearances of Soft Tissue Flaps Following Reconstructive Surgery of the Lower Extremity
- Affiliations
-
- 1Department of Radiology, Hospital Baden, Baden 5405, Switzerland. dr.o.magerkurth@gmail.com
- 2Department of Radiology, University of Michigan Hospitals, Ann Arbor, MI 48109, USA.
- KMID: 2069995
- DOI: http://doi.org/10.3348/kjr.2015.16.1.160
Abstract
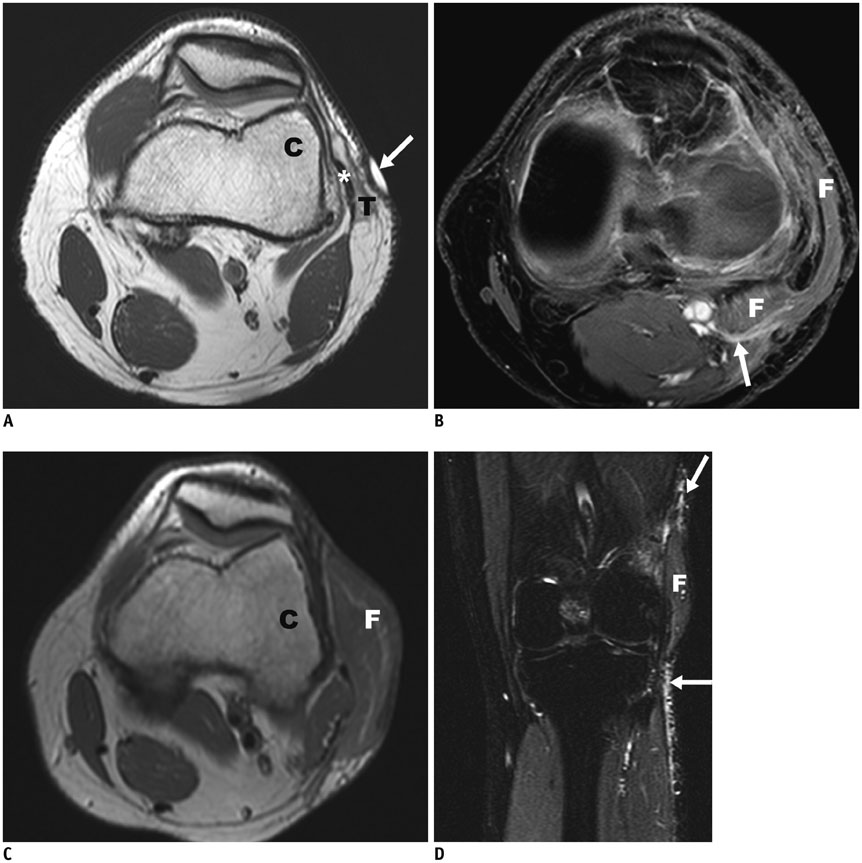
- MR imaging appearances of different types of reconstructive muscle flaps following reconstructive surgery of the lower extremity with associated post-surgical changes due to altered anatomy, radiation, and potential complications, can be challenging. A multidisciplinary therapeutic approach to tumors allows for limb salvage therapy in a majority of the patients. Decision-making for specific types of soft tissue reconstruction is based on the body region affected, as well as the size and complexity of the defect. Hematomas and infections are early complications that can jeopardize flap viability. The local recurrence of a tumor within six months after a complete resection with confirmed tumor-free margins and adjuvant radiation therapy is rare. Identification of a new lesion similar to the initial tumor favors a finding of tumor recurrence.
MeSH Terms
-
Adult
Female
Hematoma/etiology
Humans
Limb Salvage
Lower Extremity/anatomy & histology/radiography/*surgery
*Magnetic Resonance Imaging
Male
Middle Aged
Neoplasm Recurrence, Local
Reconstructive Surgical Procedures
Sarcoma/radiotherapy/*surgery
Soft Tissue Infections/radiography/*surgery
Soft Tissue Injuries/radiography/*surgery
Soft Tissue Neoplasms/radiotherapy/*surgery
Surgical Flaps/adverse effects
Figure
Reference
-
1. Bannasch H, Haivas I, Momeni A, Stark GB. Oncosurgical and reconstructive concepts in the treatment of soft tissue sarcomas: a retrospective analysis. Arch Orthop Trauma Surg. 2009; 129:43–49.2. Drake DB. Reconstruction for limb-sparing procedures in soft-tissue sarcomas of the extremities. Clin Plast Surg. 1995; 22:123–128.3. Heller L, Kronowitz SJ. Lower extremity reconstruction. J Surg Oncol. 2006; 94:479–489.4. Misra A, Mistry N, Grimer R, Peart F. The management of soft tissue sarcoma. J Plast Reconstr Aesthet Surg. 2009; 62:161–174.5. Morii T, Mochizuki K, Takushima A, Okazaki M, Satomi K. Soft tissue reconstruction using vascularized tissue transplantation following resection of musculoskeletal sarcoma: evaluation of oncologic and functional outcomes in 55 cases. Ann Plast Surg. 2009; 62:252–257.6. Serletti JM, Carras AJ, O'Keefe RJ, Rosier RN. Functional outcome after soft-tissue reconstruction for limb salvage after sarcoma surgery. Plast Reconstr Surg. 1998; 102:1576–1583. discussion 1584-1585.7. Karakousis CP, Proimakis C, Walsh DL. Primary soft tissue sarcoma of the extremities in adults. Br J Surg. 1995; 82:1208–1212.8. Popov P, Tukiainen E, Asko-Seljavaara S, Huuhtanen R, Virolainen M, Virkkunen P, et al. Soft-tissue sarcomas of the upper extremity: surgical treatment and outcome. Plast Reconstr Surg. 2004; 113:222–230. discussion 231-232.9. Zenn MR, Levin LS. Microvascular reconstruction of the lower extremity. Semin Surg Oncol. 2000; 19:272–281.10. Parrett BM, Talbot SG, Pribaz JJ, Lee BT. A review of local and regional flaps for distal leg reconstruction. J Reconstr Microsurg. 2009; 25:445–455.11. Heller L, Levin LS. Lower extremity microsurgical reconstruction. Plast Reconstr Surg. 2001; 108:1029–1041. quiz 1042.12. Moreira-Gonzalez A, Djohan R, Lohman R. Considerations surrounding reconstruction after resection of musculoskeletal sarcomas. Cleve Clin J Med. 2010; 77:Suppl 1. S18–S22.13. Achauer B, Eriksson E, Guyuron B, Coleman IJ, Russel R, Vander Kolk C. Plastic surgery: indications, operations, and outcomes. Saint-Louis: Mosby;2000. p. 475–496.14. Parrett BM, Pribaz JJ, Matros E, Przylecki W, Sampson CE, Orgill DP. Risk analysis for the reverse sural fasciocutaneous flap in distal leg reconstruction. Plast Reconstr Surg. 2009; 123:1499–1504.15. Peat BG, Bell RS, Davis A, O'Sullivan B, Mahoney J, Manktelow RT, et al. Wound-healing complications after soft-tissue sarcoma surgery. Plast Reconstr Surg. 1994; 93:980–987.16. Trecek J, Sundaram M. Radiologic case study. Extensive hematoma of the vastus intermedius showing components of subacute and chronic hemorrhage with associated myositis of the vastus intermedius and medialis. Orthopedics. 2007; 30:806880–881.17. Varma DG, Jackson EF, Pollock RE, Benjamin RS. Soft-tissue sarcoma of the extremities. MR appearance of post-treatment changes and local recurrences. Magn Reson Imaging Clin N Am. 1995; 3:695–712.18. Poon-Chue A, Menendez L, Gerstner MM, Colletti P, Terk M. MRI evaluation of post-operative seromas in extremity soft tissue sarcomas. Skeletal Radiol. 1999; 28:279–282.19. Ferguson PC. Surgical considerations for management of distal extremity soft tissue sarcomas. Curr Opin Oncol. 2005; 17:366–369.20. Vanel D, Lacombe MJ, Couanet D, Kalifa C, Spielmann M, Genin J. Musculoskeletal tumors: follow-up with MR imaging after treatment with surgery and radiation therapy. Radiology. 1987; 164:243–245.21. Costelloe CM, Kumar R, Yasko AW, Murphy WA Jr, Stafford RJ, Lewis VO, et al. Imaging characteristics of locally recurrent tumors of bone. AJR Am J Roentgenol. 2007; 188:855–863.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of soft tissue defect in the lower extremity with free flaps
- A Combined Scapular Flap and Latissimus Dorsi Flap
- Reconstruction of soft tissue injury of lower extremity with free flap transfer
- Reconstruction of lower extremity by fibular free flaps
- Reconstruction of Lower Extremities using Anterolateral thigh Perforator Free Flaps