Clin Orthop Surg.
2015 Mar;7(1):110-119. 10.4055/cios.2015.7.1.110.
Prognostic Factors of Septic Arthritis of Hip in Infants and Neonates: Minimum 5-Year Follow-up
- Affiliations
-
- 1Department of Orthopedic Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- 2Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jongsupshim@gmail.com
- KMID: 2069883
- DOI: http://doi.org/10.4055/cios.2015.7.1.110
Abstract
- BACKGROUND
The authors conducted the present study to identify clinical and radiological prognostic factors in infants and neonates with septic arthritis of the hip.
METHODS
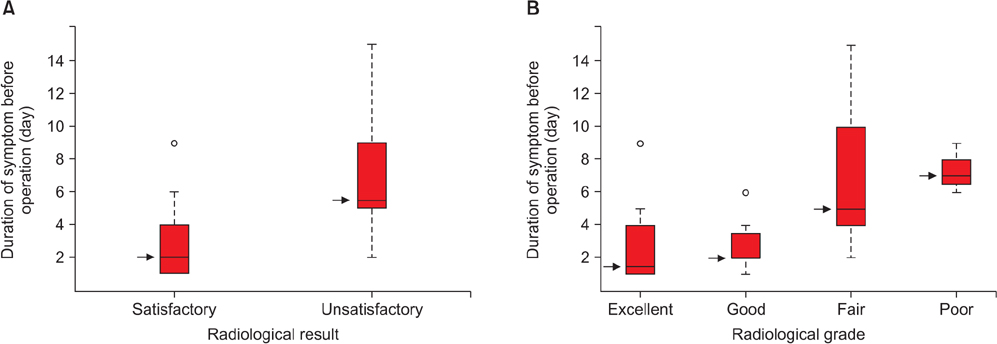
The authors retrospectively reviewed the records of 31 patients with septic arthritis of the hip. All of the patients were younger than 18 months old. Follow-up periods ranged from 5 to 17 years. The following potential variables for predicting the prognosis were included in the assessment: gender, age, underlying diseases, duration of symptoms, changes of hip joint in X-ray, concomitant osteomyelitis, elevation of erythrocyte sedimentation rate and C-reactive protein, sepsis, pus drainage, synovial fluid culture, and infecting organisms. Clinical and radiological prognoses were analyzed at the final follow-up.
RESULTS
Univariate analysis demonstrated that radiological prognoses were poorer in patients who had underlying diseases, a longer duration of symptoms, and pus drainage. However, on multivariate analysis, only the variable-duration of symptoms-was found to be statistically related with a poor radiological prognosis.
CONCLUSIONS
Although poor prognosis for patients with several underlying diseases and radiological changes has already been established, a favorable outcome might be expected with prompt surgical drainage and appropriate antibiotics.
Keyword
MeSH Terms
Figure
Reference
-
1. Belthur MV, Palazzi DL, Miller JA, Phillips WA, Weinberg J. A clinical analysis of shoulder and hip joint infections in children. J Pediatr Orthop. 2009; 29(7):828–833.2. Choi IH, Pizzutillo PD, Bowen JR, Dragann R, Malhis T. Sequelae and reconstruction after septic arthritis of the hip in infants. J Bone Joint Surg Am. 1990; 72(8):1150–1165.3. Kabak S, Halici M, Akcakus M, Cetin N, Narin N. Septic arthritis in patients followed-up in neonatal intensive care unit. Pediatr Int. 2002; 44(6):652–657.4. Kang SN, Sanghera T, Mangwani J, Paterson JM, Ramachandran M. The management of septic arthritis in children: systematic review of the English language literature. J Bone Joint Surg Br. 2009; 91(9):1127–1133.5. Chen CE, Ko JY, Li CC, Wang CJ. Acute septic arthritis of the hip in children. Arch Orthop Trauma Surg. 2001; 121(9):521–526.6. Nunn TR, Cheung WY, Rollinson PD. A prospective study of pyogenic sepsis of the hip in childhood. J Bone Joint Surg Br. 2007; 89(1):100–106.7. Shaw BA, Kasser JR. Acute septic arthritis in infancy and childhood. Clin Orthop Relat Res. 1990; (257):212–225.8. Klein DM, Barbera C, Gray ST, Spero CR, Perrier G, Teicher JL. Sensitivity of objective parameters in the diagnosis of pediatric septic hips. Clin Orthop Relat Res. 1997; (338):153–159.9. Bennett OM, Namnyak SS. Acute septic arthritis of the hip joint in infancy and childhood. Clin Orthop Relat Res. 1992; (281):123–132.10. Morrey BF, Bianco AJ Jr, Rhodes KH. Septic arthritis in children. Orthop Clin North Am. 1975; 6(4):923–934.11. Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005; 6(1):2–8.12. Merle D'Aubigne R. Numerical classificaion of the function of the hip: 1970. Rev Chir Orthop Reparatrice Appar Mot. 1990; (76):371–374.13. Caksen H, Ozturk MK, Uzum K, Yuksel S, Ustunbas HB, Per H. Septic arthritis in childhood. Pediatr Int. 2000; 42(5):534–540.14. Howard JB, Highgenboten CL, Nelson JD. Residual effects of septic arthritis in infancy and childhood. JAMA. 1976; 236(8):932–935.15. Morrey BF, Bianco AJ, Rhodes KH. Suppurative arthritis of the hip in children. J Bone Joint Surg Am. 1976; 58(3):388–392.16. Obletz BE. Acute suppurative arthritis of the hip in the neonatal period. J Bone Joint Surg Am. 1960; 42(1):23–30.17. Al Saadi MM, Al Zamil FA, Bokhary NA, Al Shamsan LA, Al Alola SA, Al Eissa YS. Acute septic arthritis in children. Pediatr Int. 2009; 51(3):377–380.18. Wang CL, Wang SM, Yang YJ, Tsai CH, Liu CC. Septic arthritis in children: relationship of causative pathogens, complications, and outcome. J Microbiol Immunol Infect. 2003; 36(1):41–46.19. Yamagishi Y, Togawa M, Shiomi M. Septic arthritis and acute hematogenous osteomyelitis in childhood at a tertiary hospital in Japan. Pediatr Int. 2009; 51(3):371–376.20. Young TP, Maas L, Thorp AW, Brown L. Etiology of septic arthritis in children: an update for the new millennium. Am J Emerg Med. 2011; 29(8):899–902.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features of Septic Arthritis in Neonates
- Arthroscopic Treatment of Septic Arthritis of the Hip in a Child: A Case Report
- Treatment of the Pyogenic Arthritis of Hip in Neonates and Infants
- Mycoplasma hominis Septic Arthritis of the Hip Developed in the Postpartum Period
- Hematogenous Septic Arthritis of the Hip in Extensive Burn