Korean J Urol.
2014 Oct;55(10):670-676. 10.4111/kju.2014.55.10.670.
Role of Urinary Levels of Endothelin-1, Monocyte Chemotactic Peptide-1, and N-Acetyl Glucosaminidase in Predicting the Severity of Obstruction in Hydronephrotic Neonates
- Affiliations
-
- 1Antimicrobial Resistant Nosocomial Infection Research Center, Mazandaran University of Medical Sciences, Sari, Iran. hamidmjaafari@yahoo.com
- 2Molecular and Cell Biology Research Center, Hemoglubinopathy Institute, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
- 3Department of Radiology, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
- KMID: 2069791
- DOI: http://doi.org/10.4111/kju.2014.55.10.670
Abstract
- PURPOSE
Antenatal hydronephrosis (AH) is found in 0.5%-1% of neonates. The aim of the study was to assess the urinary concentrations of 3 biomarkers, endothelin-1 (ET-1), monocyte chemotactic peptide-1 (MCP-1), and N-acetyl-glucosaminidase (NAG) in severely hydronephrotic neonates.
MATERIALS AND METHODS
Neonates with a history of prenatal hydronephrosis were enrolled in the prospective study in 2 groups. Group 1 included neonates with severe forms of obstruction requiring surgical intervention and group 2 included neonates with milder forms of obstruction without any functional impairment. Fresh voided urinary levels of ET-1, MCP-1, and NAG were measured and their ratios to urinary Cr were calculated.
RESULTS
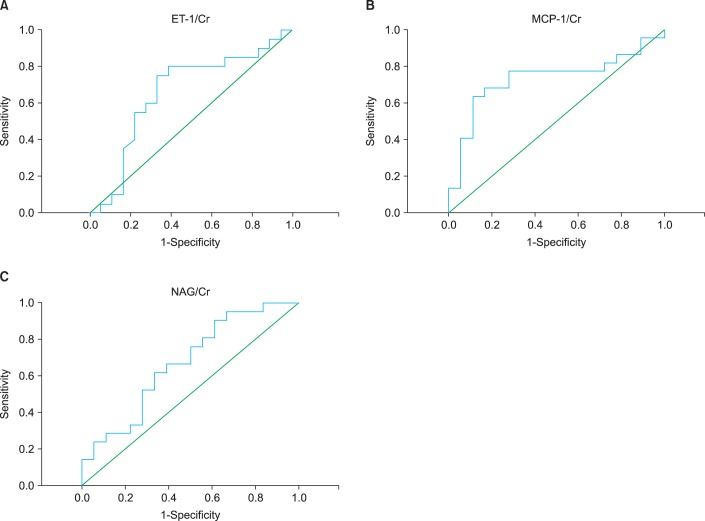
Fourty-two neonates were enrolled into the 2 groups: group 1, 24 patients (21 male, 3 female); group 2, 18 neonates (16 male, 2 female). There were no statistically significant differences between urinary ET-1, NAG, MCP-1 values, and ET-1/Cr and NAG/Cr ratios in groups 1 and 2. The urinary MCP-1/Cr ratio was significantly higher in group 1 than in group 2. For comparison of groups 1 and 2, the cut-off values were measured as 0.5709 ng/mg (sensitivity, 75%; specificity, 67%; positive predictive value [PPV], 71%; negative predictive value [NPV], 71%), 0.927 ng/mg (sensitivity, 77%; specificity, 72%; PPV, 77%; NPV, 72%), and 1.1913 IU/mg (sensitivity, 62%; specificity, 67%; PPV, 68%; NPV, 60%) for ET-1/Cr, MCP-1/Cr, and NAG/Cr ratios, respectively.
CONCLUSIONS
The urinary MCP-1/Cr ratio is significantly elevated in neonates with severe obstruction requiring surgical intervention. Based upon these results, urinary MCP-1/Cr may be useful in identification of severe obstructive hydronephrosis in neonates.
MeSH Terms
-
Acetylglucosaminidase/*urine
Biological Markers/urine
Chemokine CCL2/*urine
Endothelin-1/*urine
Female
Humans
Hydronephrosis/*congenital/etiology/surgery/ultrasonography
Infant, Newborn
Male
Predictive Value of Tests
Prospective Studies
Sensitivity and Specificity
Ureteral Obstruction/complications/*diagnosis/surgery
Acetylglucosaminidase
Biological Markers
Chemokine CCL2
Endothelin-1
Figure
Reference
-
1. Coplen DE. The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis: Nguyen HT, Herndon CDA, Cooper C, et al (Children's Hosp, Boston, MA; Children's Hosp of Alabama, Birmingham; Univ of Iowa Med Ctr, Iowa City; et al) J Pediatr Urol 6:212-231, 2010. Yearb Urol. 2010; 2010:209.2. Yamacake KG, Nguyen HT. Current management of antenatal hydronephrosis. Pediatr Nephrol. 2013; 28:237–243. PMID: 22836304.
Article3. Mohammadjafari H, Alam A, Kosarian M, Mousavi SA, Kosarian S. Vesicoureteral reflux in neonates with hydronephrosis; role of imaging tools. Iran J Pediatr. 2009; 19:347–353.4. Vazirian S, Mohammadjafari H, Mohammadjafari R. Postnatal management of prenatal hydronephrosis. J Clin Excell. 2013; 1:63–82.5. Ucero AC, Benito-Martin A, Izquierdo MC, Sanchez-Nino MD, Sanz AB, Ramos AM, et al. Unilateral ureteral obstruction: beyond obstruction. Int Urol Nephrol. 2014; 46:765–776. PMID: 24072452.
Article6. Cao YS, Yu DX, Cai Y, Chao M. Diagnosis and treatment of ureteropelvic junction obstruction in children. J Appl Clin Pediatr. 2007; 22:825.7. Klein J, Gonzalez J, Miravete M, Caubet C, Chaaya R, Decramer S, et al. Congenital ureteropelvic junction obstruction: human disease and animal models. Int J Exp Pathol. 2011; 92:168–192. PMID: 20681980.
Article8. Abedi SM, Mohammadjafari H, Hosseinimehr SJ, Mardanshahi A, Shahhosseini R. Imaging of renal cortex in nuclear medicine. J Clin Excell. 2014; 2:50–69.9. Mohammadjafari H, Rafiei A, Abedi M, Aalaee A, Mirabi AM, Abedi E. Urinary neutrophil-gelatinase associated lipocalin is a more prognostic biomarker to distinguish antenatal hydronephrosis in neonates. Res Mol Med. 2013; 1:10–16.
Article10. Trnka P, Hiatt MJ, Tarantal AF, Matsell DG. Congenital urinary tract obstruction: defining markers of developmental kidney injury. Pediatr Res. 2012; 72:446–454. PMID: 22902433.
Article11. Chevalier RL. Obstructive nephropathy: towards biomarker discovery and gene therapy. Nat Clin Pract Nephrol. 2006; 2:157–168. PMID: 16932414.
Article12. Mohammadjafari H, Rafiei A, Abedi M, Aalaee A, Abedi E. The role of urinary TIMP1 and MMP9 levels in predicting vesicoureteral reflux in neonates with antenatal hydronephrosis. Pediatr Nephrol. 2014; 29:871–878. PMID: 24389602.
Article13. Sharifian M, Ahmadi M, Karimi A, Zand RE, Moghadar R, Ahmadi R, et al. Urinary endothellin-1 level in children with pyelonephritis and hydronephrosis. Saudi J Kidney Dis Transpl. 2013; 24:731–736. PMID: 23816722.
Article14. Pollock D. Endothelin and the kidney. In : Battistini B, Warner TD, editors. Endothelin and its inhibitors. New York: Springer;2001. p. 477–501.15. Grandaliano G, Gesualdo L, Bartoli F, Ranieri E, Monno R, Leggio A, et al. MCP-1 and EGF renal expression and urine excretion in human congenital obstructive nephropathy. Kidney Int. 2000; 58:182–192. PMID: 10886563.
Article16. Stephan M, Conrad S, Eggert T, Heuer R, Fernandez S, Huland H. Urinary concentration and tissue messenger RNA expression of monocyte chemoattractant protein-1 as an indicator of the degree of hydronephrotic atrophy in partial ureteral obstruction. J Urol. 2002; 167:1497–1502. PMID: 11832777.
Article17. Skalova S, Rejtar P, Kutilek S. Increased urinary N-acetyl-beta-D-glucosaminidase activity in children with hydronephrosis. Int Braz J Urol. 2007; 33:80–83. PMID: 17335604.
Article18. Ma H, Fang Y, Tian WC, Qian K, Li J, Yang JJ, et al. Clinical value of renal dynamic imaging and urinary N-acetyl-β-D-glucosaminidase, apoptosis DNA fragment detection in evaluating damage degree of hydronephrotic kidneys in children with hydronephrosis. J Appl Clin Pediatr. 2009; 16:036.19. Csathy L, Pocsi I. Urinary N-acetyl-beta-D-glucosaminidase determination in newborns and children: methods and diagnostic applications. Eur J Clin Chem Clin Biochem. 1995; 33:575–587. PMID: 8611667.20. Chertin B, Pollack A, Koulikov D, Rabinowitz R, Hain D, Hadas-Halpren I, et al. Conservative treatment of ureteropelvic junction obstruction in children with antenatal diagnosis of hydronephrosis: lessons learned after 16 years of follow-up. Eur Urol. 2006; 49:734–738. PMID: 16504374.
Article21. Tombesi MM, Alconcher LF. Short-term outcome of mild isolated antenatal hydronephrosis conservatively managed. J Pediatr Urol. 2012; 8:129–133. PMID: 21798811.
Article22. Chevalier RL, Thornhill BA, Forbes MS, Kiley SC. Mechanisms of renal injury and progression of renal disease in congenital obstructive nephropathy. Pediatr Nephrol. 2010; 25:687–697. PMID: 19844747.
Article23. Bartoli F, Penza R, Aceto G, Niglio F, D'ddato O, Pastore V, et al. Urinary epidermal growth factor, monocyte chemotactic protein-1, and β2-microglobulin in children with ureteropelvic junction obstruction. J Pediatr Surg. 2011; 46:530–536. PMID: 21376205.
Article24. Taranta-Janusz K, Wasilewska A, Debek W, Waszkiewicz-Stojda M. Urinary cytokine profiles in unilateral congenital hydronephrosis. Pediatr Nephrol. 2012; 27:2107–2113. PMID: 22744767.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endothelin-1, Endothelin-2 and Endothelin-3 Induced Expression of Monocyte Chemoattractant Protein-1 in Rat Mesangial Cells
- Role of urinary N-acetyl-beta-D-glucosaminidase in predicting the prognosis of antenatal hydronephrosis
- Endothelin-1 In Patients With Lupus Nephritis
- Urinary N-Acetyl-beta-D-Glucosaminidase and beta 2-Microglobulin in Children with Various Renal Diseases
- Urinary N-acetyl-beta-D-glucosaminidase in rheumatoid arthritis