Korean J Urol.
2014 Sep;55(9):608-614. 10.4111/kju.2014.55.9.608.
Effect of Improvement in Lower Urinary Tract Symptoms on Sexual Function in Men: Tamsulosin Monotherapy vs. Combination Therapy of Tamsulosin and Solifenacin
- Affiliations
-
- 1Department of Urology, Hallym University College of Medicine, Chuncheon, Korea.
- 2Department of Urology, The Catholic University College of Medicine, Seoul, Korea.
- 3Department of Urology, Korea University College of Medicine, Seoul, Korea.
- 4Department of Urology, Yeungnam University College of Medicine, Daegu, Korea.
- 5Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 6Department of Urology, Chonbuk National University Medical School, Jeonju, Korea.
- 7Department of Urology, Seoul National University College of Medicine, Seoul, Korea.
- 8Department of Urology, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 9Department of Urology, Gyeongsang National University School of Medicine, Jinju, Korea.
- 10Department of Urology, Chonnam National University Medical School, Gwangju, Korea. kpark@chonnam.ac.kr
- KMID: 2069779
- DOI: http://doi.org/10.4111/kju.2014.55.9.608
Abstract
- PURPOSE
To evaluate how much the improvement of lower urinary tract symptoms (LUTS) affects sexual function and which storage symptoms or voiding symptoms have the greatest effect on sexual function.
MATERIALS AND METHODS
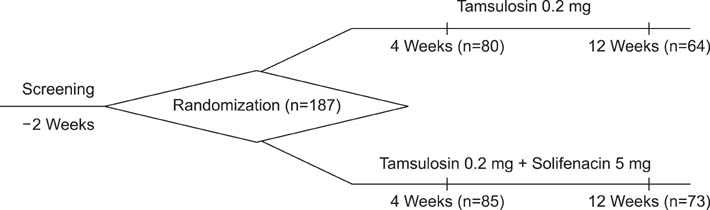
A total of 187 patients were enrolled in this study. Patients were randomly assigned to receive either tamsulosin 0.2 mg (group A) or tamsulosin 0.2 mg and solifenacin 5 mg (group B). At 4 weeks and 12 weeks, the LUTS and sexual function of the patients were evaluated by use of the International Index of Erectile Function-5 (IIEF5), International Prostate Symptom Score (IPSS), Overactive Bladder Symptom Score (OABSS) questionnaire, uroflowmetry, and bladder scan.
RESULTS
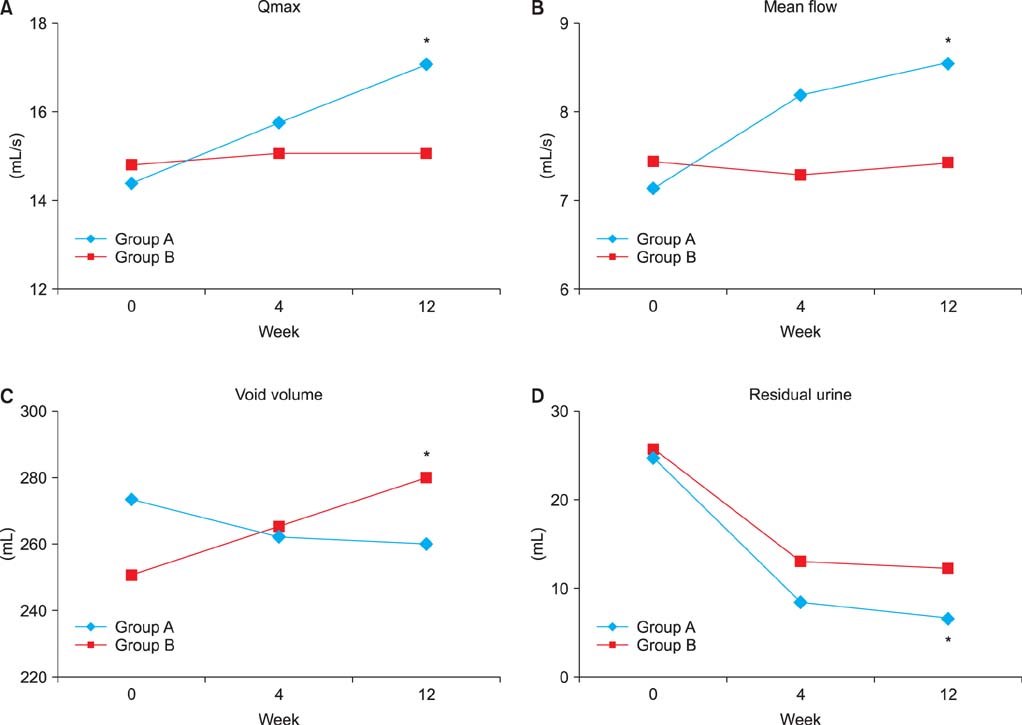
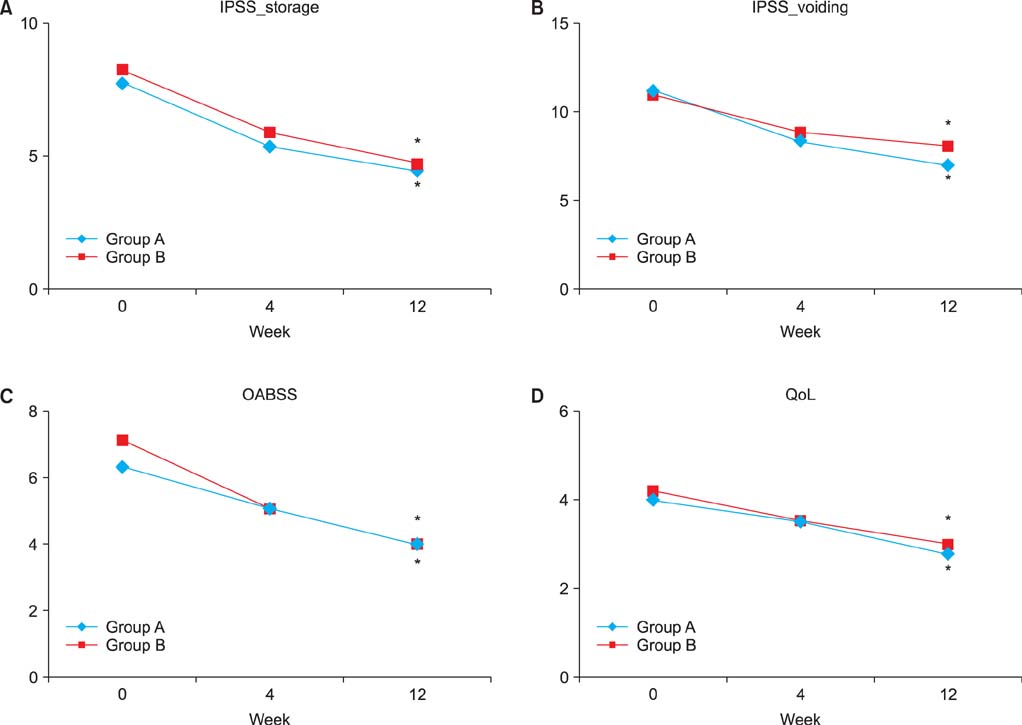
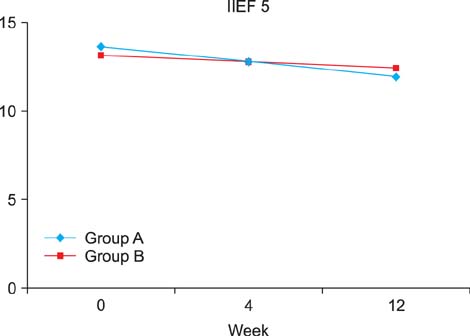
Both groups A and B showed statistically significant improvements in IPSS, OABSS, and quality of life (QoL). Group A showed improved maximum flow rate, mean flow rate, and residual urine volume by time. Group B did not show an improvement in flow rate or residual urine volume but total voiding volume increased with time. The IIEF5 score was not improved in either group. In group A, the IIEF5 score dropped from 13.66+/-4.97 to 11.93+/-6.14 after 12 weeks (p=0.072). Group B showed a decline in the IIEF5 score from 13.19+/-5.91 to 12.45+/-6.38 (p=0.299). Although group B showed a relatively smaller decrease in the IIEF5 score, the difference between the two groups was not significant (p=0.696).
CONCLUSIONS
Tamsulosin monotherapy and combination therapy with solifenacin did not improve erectile function despite improvements in voiding symptoms and QoL. The improvement in storage symptoms did not affect erectile function.
MeSH Terms
-
Aged
Drug Therapy, Combination/methods
Erectile Dysfunction/*drug therapy/etiology
Humans
Lower Urinary Tract Symptoms/complications/*drug therapy
Male
Middle Aged
Quality of Life
Questionnaires
Quinuclidines/*administration & dosage
Rheology
Sulfonamides/*administration & dosage
Tetrahydroisoquinolines/*administration & dosage
Treatment Outcome
Urological Agents/*administration & dosage
Quinuclidines
Sulfonamides
Tetrahydroisoquinolines
Urological Agents
Figure
Reference
-
1. Rosen RC, Wei JT, Althof SE, Seftel AD, Miner M, Perelman MA, et al. Association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH Registry. Urology. 2009; 73:562–566.2. Jeh SU, Chung KH, Jung JH, Hyun JS. Improvement of lower urinary tract symptoms and sexual function after treatment with alpha-blocker. Korean J Urol. 2009; 50:369–374.3. Kumar R, Nehra A, Jacobson DJ, McGree ME, Gades NM, Lieber MM, et al. Alpha-blocker use is associated with decreased risk of sexual dysfunction. Urology. 2009; 74:82–87.4. Nordling J. Efficacy and safety of two doses (10 and 15 mg) of alfuzosin or tamsulosin (0.4 mg) once daily for treating symptomatic benign prostatic hyperplasia. BJU Int. 2005; 95:1006–1012.5. Kim SW, Lee WC, Kim MT, Ko K, Lee WK, Lee CH, et al. Effects of low-dose tamsulosin on sexual function in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Korean J Urol. 2013; 54:697–702.6. Roehrborn CG, Kaplan SA, Kraus SR, Wang JT, Bavendam T, Guan Z. Effects of serum PSA on efficacy of tolterodine extended release with or without tamsulosin in men with LUTS, including OAB. Urology. 2008; 72:1061–1067.7. Lee SH, Byun SS, Lee SJ, Kim KH, Lee JY. Effects of initial combined tamsulosin and solifenacin therapy for overactive bladder and bladder outlet obstruction secondary to benign prostatic hyperplasia: a prospective, randomized, multicenter study. Int Urol Nephrol. 2014; 46:523–529.8. Kaplan SA, Roehrborn CG, Chancellor M, Carlsson M, Bavendam T, Guan Z. Extended-release tolterodine with or without tamsulosin in men with lower urinary tract symptoms and overactive bladder: effects on urinary symptoms assessed by the International Prostate Symptom Score. BJU Int. 2008; 102:1133–1139.9. Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol. 2003; 44:637–649.10. Haillot O, Fraga A, Maciukiewicz P, Pushkar D, Tammela T, Hofner K, et al. The effects of combination therapy with dutasteride plus tamsulosin on clinical outcomes in men with symptomatic BPH: 4-year post hoc analysis of European men in the CombAT study. Prostate Cancer Prostatic Dis. 2011; 14:302–306.11. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003; 349:2387–2398.12. Lemack GE. Defining the role of overactive bladder treatments in men with lower urinary tract symptoms. Nat Clin Pract Urol. 2007; 4:174–175.13. Leliefeld HH, Stoevelaar HJ, McDonnell J. Sexual function before and after various treatments for symptomatic benign prostatic hyperplasia. BJU Int. 2002; 89:208–213.14. Aslan G, Cavus E, Karas H, Oner O, Duran F, Esen A. Association between lower urinary tract symptoms and erectile dysfunction. Arch Androl. 2006; 52:155–162.15. Irwin DE, Milsom I, Reilly K, Hunskaar S, Kopp Z, Herschorn S, et al. Overactive bladder is associated with erectile dysfunction and reduced sexual quality of life in men. J Sex Med. 2008; 5:2904–2910.16. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314.17. Glasser DB, Carson C 3rd, Kang JH, Laumann EO. Prevalence of storage and voiding symptoms among men aged 40 years and older in a US population-based study: results from the Male Attitudes Regarding Sexual Health study. Int J Clin Pract. 2007; 61:1294–1300.18. Kaplan SA, He W, Koltun WD, Cummings J, Schneider T, Fakhoury A. Solifenacin plus tamsulosin combination treatment in men with lower urinary tract symptoms and bladder outlet obstruction: a randomized controlled trial. Eur Urol. 2013; 63:158–165.19. Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome--overactive bladder symptom score. Urology. 2006; 68:318–323.20. Barry MJ. Evaluation of symptoms and quality of life in men with benign prostatic hyperplasia. Urology. 2001; 58:6 Suppl 1. 25–32.21. Kim YH, Seo JT, Yoon H. The effect of overactive bladder syndrome on the sexual quality of life in Korean young and middle aged women. Int J Impot Res. 2005; 17:158–163.22. Rogers R, Bachmann G, Jumadilova Z, Sun F, Morrow JD, Guan Z, et al. Efficacy of tolterodine on overactive bladder symptoms and sexual and emotional quality of life in sexually active women. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:1551–1557.23. Hajebrahimi S, Azaripour A, Sadeghi-Bazargani H. Tolterodine immediate release improves sexual function in women with overactive bladder. J Sex Med. 2008; 5:2880–2885.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia Treatment with Tamsulosin and Solifenacin Combination Therapy on Erectile Function
- Effects of Tamsulosin, Solifenacin, and Combination Therapy for the Treatment of Ureteral Stent Related Discomforts
- Detrusor Overactivity May Be a Prognostic Factor for Better Response to Combination Therapy Over Monotherapy in Male Patients With Benign Prostatic Enlargement and Storage Lower Urinary Tract Symptoms
- The Effect of Finasteride, Tamsulosin and Doxazosin Therapy on Sexual Function in Patients with Benign Prostatic Hyperplasia
- The Experience with Combination of Finasteride and Tamsulosin on Benign Prostatic Hyperplasia