Infect Chemother.
2015 Jun;47(2):125-128. 10.3947/ic.2015.47.2.125.
Enterobacter cloacae Sacroiliitis with Acute Respiratory Distress Syndrome in an Adolescent
- Affiliations
-
- 1Department of Pediatrics and Adolescent, Hanyang University College of Medicine, Seoul, Korea. sungheeo@hanyang.ac.kr
- 2Department of Radiology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2068999
- DOI: http://doi.org/10.3947/ic.2015.47.2.125
Abstract
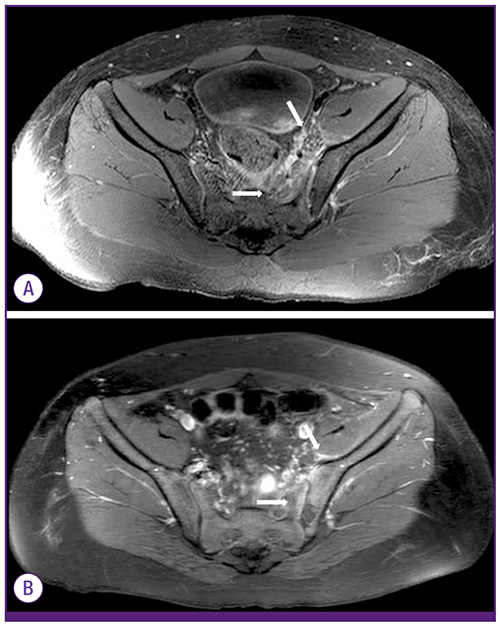
- Enterobacter cloacae has emerged as an important nosocomial pathogen, but is rarely a cause of sacroiliitis. Herein, we present the first reported case of Enterobacter cloacae sacroiliitis associated with sepsis and acute respiratory distress syndrome (ARDS). A previously healthy 14-year-old boy presented with low-grade fever and pain in the left side of the hip that was aggravated by walking. Pelvic computed tomography (CT) showed normal findings, and the patient received supportive care for transient synovitis with no antibiotics. However, there was no clinical improvement. On the third day of hospitalization, magnetic resonance imaging of the hip revealed findings compatible with sacroiliitis, for which vancomycin and ceftriaxone were administered. The patient suddenly developed high fever with dyspnea. Chest radiography and CT findings and a PaO2/FiO2 ratio <200 mmHg were suggestive of ARDS; the patient subsequently received ventilatory support and low-dose methylprednisolone infusions. Within one week, defervescence occurred, and the patient was able to breathe on his own. Following the timely recognition of, and therapeutic challenge to, ARDS, and after 6 weeks of parenteral antimicrobial therapy, the patient was discharged in good health with no complications.
MeSH Terms
-
Adolescent*
Anti-Bacterial Agents
Ceftriaxone
Dyspnea
Enterobacter cloacae*
Fever
Hip
Hospitalization
Humans
Magnetic Resonance Imaging
Male
Methylprednisolone
Radiography
Respiratory Distress Syndrome, Adult*
Sacroiliitis*
Sepsis
Synovitis
Thorax
Vancomycin
Walking
Anti-Bacterial Agents
Ceftriaxone
Methylprednisolone
Vancomycin
Figure
Reference
-
1. Schaad UB, McCracken GH Jr, Nelson JD. Pyogenic arthritis of the sacroiliac joint in pediatric patients. Pediatrics. 1980; 66:375–379.
Article2. Taylor ZW, Ryan DD, Ross LA. Increased incidence of sacroiliac joint infection at a children's hospital. J Pediatr Orthop. 2010; 30:893–898.
Article3. Molinos Quintana A, Morillo Gutiérrez B, Camacho Lovillo MS, Neth O, Obando Santaella I. Pyogenic sacroiliitis in children - a diagnostic challenge. Clin Rheumatol. 2011; 30:107–113.
Article4. Wu MS, Chang SS, Lee SH, Lee CC. Pyogenic sacroiliitis--a comparison between paediatric and adult patients. Rheumatology (Oxford). 2007; 46:1684–1687.
Article5. Asavamongkolkul A, Keerasuntonpong A, Kuagoolwongse C. Pyogenic sacroiliitis and adult respiratory distress syndrome: a case report. J Orthop Surg (Hong Kong). 2007; 15:226–229.
Article6. Konrad D, Zbinden R, Kuster H, Hunziker UA. Group G streptococcus sacroiliitis with sepsis in a 15-year-old adolescent. Scand J Infect Dis. 1999; 31:100–102.7. Wada A, Takamura K, Fujii T, Yanagida H, Surijamorn P. Septic sacroiliitis in children. J Pediatr Orthop. 2008; 28:488–492.
Article8. Ford LS, Ellis AM, Allen HW, Campbell DE. Osteomyelitis and pyogenic sacroiliitis: A difficult diagnosis. J Paediatr Child Health. 2004; 40:317–319.
Article9. Vyskocil JJ, Mcllroy MA, Brennan TA, Wilson FM. Pyogenic infection of the sacroiliac joint. Case reports and review of the literature. Medicine (Baltimore). 1991; 70:188–197.
Article10. Doita M, Yoshiya S, Nabeshima Y, Tanase Y, Nishida K, Miyamoto H, Watanabe Y, Kurosaka M. Acute pyogenic sacroiliitis without predisposing conditions. Spine (Phila Pa 1976). 2003; 28:E384–E389.
Article11. Hizel K, Guzel O, Dizbay M, Karakus R, Senol E, Arman D, Aktas F, Ulutan F. Age and duration of disease as factors affecting clinical findings and sacroiliitis in brucellosis. Infection. 2007; 35:434–437.
Article12. Harbarth S, Sudre P, Dharan S, Cadenas M, Pittet D. Outbreak of Enterobacter cloacae related to understaffing, overcrowding, and poor hygiene practices. Infect Control Hosp Epidemiol. 1999; 20:598–603.
Article13. ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–2533.14. Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998; 338:347–354.
Article15. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–1308.16. Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, Gibson M, Umberger R. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest. 2007; 131:954–963.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Activity of cefepime against enterobacter cloacae, serratin marcesc- ens, pseudomonas aeruginosa and other aerobic gram-negative bacilli
- Pneumatocele Caused by Enterobacter cloacae in the Preterm Neonates
- Treatment of Acute Respiratory Distress Syndrome
- Klebsiella pneumoniae and Enterobacter cloacae Induced Septic Arthritis in a Healthy Adolescent: A Rare Case Report
- Clinical Manifestations and Diagnosis of Acute Respiratory Distress Syndrome