Yonsei Med J.
2014 May;55(3):606-616. 10.3349/ymj.2014.55.3.606.
Efficacy of Combination Treatment with Intracoronary Abciximab and Aspiration Thrombectomy on Myocardial Perfusion in Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Coronary Stenting
- Affiliations
-
- 1Division of Cardiology, Yonsei University Wonju College of Medicine, Wonju, Korea. carshlee@yonsei.ac.kr
- 2Department of Cardiology, Ajou University Medical Center, Suwon, Korea. sjtahk@ajou.ac.kr
- KMID: 2068669
- DOI: http://doi.org/10.3349/ymj.2014.55.3.606
Abstract
- PURPOSE
We aimed to investigate whether combination therapy using intracoronary (IC) abciximab and aspiration thrombectomy (AT) enhances myocardial perfusion compared to each treatment alone in patients with ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (PCI).
MATERIALS AND METHODS
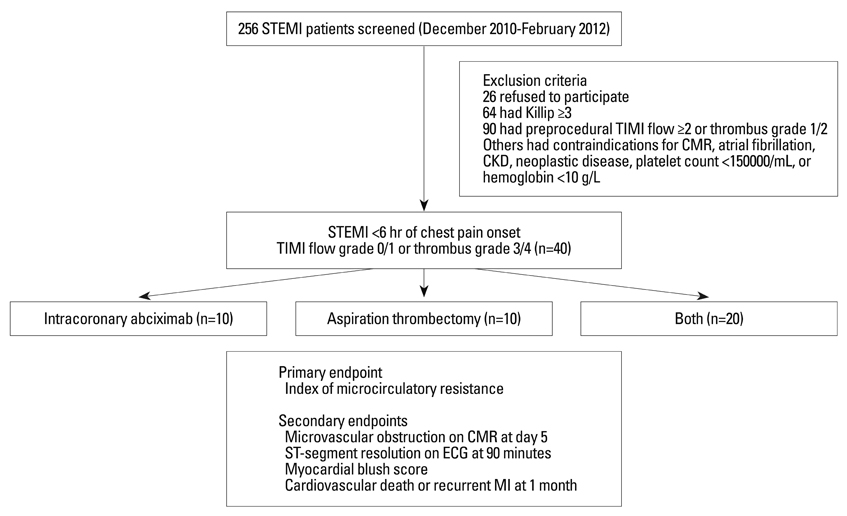
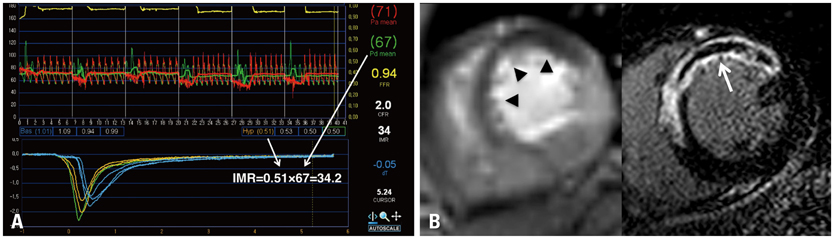
We enrolled 40 patients with STEMI, who presented within 6 h of symptom onset and had Thrombolysis in MI flow 0/1 or a large angiographic thrombus burden (grade 3/4). Patients were randomly divided into 3 groups: 10 patients who received a bolus of IC abciximab (0.25 mg/kg); 10 patients who received only AT; and 20 patients who received both treatments. The index of microcirculatory resistance (IMR) was measured with a pressure sensor/thermistor-tipped guidewire following successful PCI. Microvascular obstruction (MVO) was assessed using cardiac magnetic resonance imaging on day 5.
RESULTS
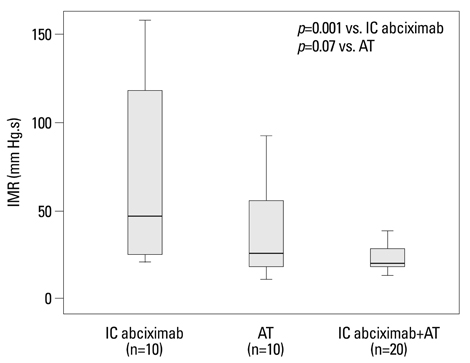
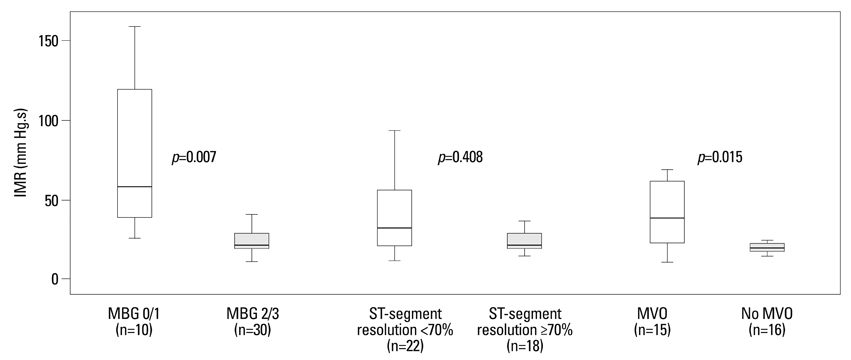
IMR was lower in the combination group than in the IC abciximab group (23.5+/-7.4 U vs. 66.9+/-48.7 U, p=0.001) and tended to be lower than in the AT group, with barely missed significance (23.5+/-7.4 U vs. 37.2+/-26.1 U, p=0.07). MVO was observed less frequently in the combination group than in the IC abciximab group (18.8% vs. 88.9%, p=0.002) and tended to occur less frequently than in the AT group (18.8% vs. 66.7%, p=0.054). No difference of IMR and MVO was found between the IC abciximab and the AT group (66.9+/-48.7 U vs. 37.2+/-26.1 U, p=0.451 for IMR; 88.9% vs. 66.7%, p=0.525 for MVO, respectively).
CONCLUSION
Combination treatment using IC abciximab and AT may synergistically improve myocardial perfusion in patients with STEMI undergoing primary PCI (Trial Registration: clinicaltrials. gov Identifier: NCT01404507).
MeSH Terms
Figure
Reference
-
1. Rezkalla SH, Kloner RA. No-reflow phenomenon. Circulation. 2002; 105:656–662.
Article2. Bekkers SC, Yazdani SK, Virmani R, Waltenberger J. Microvascular obstruction: underlying pathophysiology and clinical diagnosis. J Am Coll Cardiol. 2010; 55:1649–1660.3. Lerman A, Holmes DR, Herrmann J, Gersh BJ. Microcirculatory dysfunction in ST-elevation myocardial infarction: cause, consequence, or both? Eur Heart J. 2007; 28:788–797.
Article4. Jaffe R, Dick A, Strauss BH. Prevention and treatment of microvascular obstruction-related myocardial injury and coronary no-reflow following percutaneous coronary intervention: a systematic approach. JACC Cardiovasc Interv. 2010; 3:695–704.
Article5. Lee HY, Kim JH, Kim BO, Kang YJ, Ahn HS, Hwang MW, et al. Effect of Aspiration Thrombectomy on Microvascular Dysfunction in ST-Segment Elevation Myocardial Infarction With an Elevated Neutrophil Count. Korean Circ J. 2011; 41:68–75.
Article6. van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation. 1998; 97:2302–2306.7. Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000; 101:125–130.
Article8. Dibra A, Mehilli J, Dirschinger J, Pache J, Neverve J, Schwaiger M, et al. Thrombolysis in myocardial infarction myocardial perfusion grade in angiography correlates with myocardial salvage in patients with acute myocardial infarction treated with stenting or thrombolysis. J Am Coll Cardiol. 2003; 41:925–929.
Article9. Stone GW, Webb J, Cox DA, Brodie BR, Qureshi M, Kalynych A, et al. Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction: a randomized controlled trial. JAMA. 2005; 293:1063–1072.
Article10. Kaltoft A, Bøttcher M, Nielsen SS, Hansen HH, Terkelsen C, Maeng M, et al. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment-elevation myocardial infarction: a randomized, controlled trial. Circulation. 2006; 114:40–47.
Article11. Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008; 358:557–567.
Article12. Sardella G, Mancone M, Bucciarelli-Ducci C, Agati L, Scardala R, Carbone I, et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol. 2009; 53:309–315.
Article13. Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008; 371:1915–1920.
Article14. Mehilli J, Kastrati A, Schulz S, Früngel S, Nekolla SG, Moshage W, et al. Abciximab in patients with acute ST-segment-elevation myocardial infarction undergoing primary percutaneous coronary intervention after clopidogrel loading: a randomized double-blind trial. Circulation. 2009; 119:1933–1940.
Article15. Kini AS, Chen VH, Krishnan P, Lee P, Kim MC, Mares A, et al. Bolus-only versus bolus + infusion of glycoprotein IIb/IIIa inhibitors during percutaneous coronary intervention. Am Heart J. 2008; 156:513–519.
Article16. Stone GW, Maehara A, Witzenbichler B, Godlewski J, Parise H, Dambrink JH, et al. Intracoronary abciximab and aspiration thrombectomy in patients with large anterior myocardial infarction: the INFUSE-AMI randomized trial. JAMA. 2012; 307:1817–1826.
Article17. Burzotta F, De Vita M, Gu YL, Isshiki T, Lefèvre T, Kaltoft A, et al. Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-data pooled analysis of 11 trials. Eur Heart J. 2009; 30:2193–2203.
Article18. Lockie T, Nagel E, Redwood S, Plein S. Use of cardiovascular magnetic resonance imaging in acute coronary syndromes. Circulation. 2009; 119:1671–1681.
Article19. Ørn S, Manhenke C, Greve OJ, Larsen AI, Bonarjee VV, Edvardsen T, et al. Microvascular obstruction is a major determinant of infarct healing and subsequent left ventricular remodelling following primary percutaneous coronary intervention. Eur Heart J. 2009; 30:1978–1985.
Article20. Fearon WF, Shah M, Ng M, Brinton T, Wilson A, Tremmel JA, et al. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008; 51:560–565.
Article21. Fearon WF, Low AF, Yong AS, McGeoch R, Berry C, Shah MG, et al. Prognostic value of the Index of Microcirculatory Resistance measured after primary percutaneous coronary intervention. Circulation. 2013; 127:2436–2441.
Article22. McGeoch R, Watkins S, Berry C, Steedman T, Davie A, Byrne J, et al. The index of microcirculatory resistance measured acutely predicts the extent and severity of myocardial infarction in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2010; 3:715–722.
Article23. Gibson CM, de Lemos JA, Murphy SA, Marble SJ, McCabe CH, Cannon CP, et al. Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation. 2001; 103:2550–2554.
Article24. Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987; 76:142–154.
Article25. Fearon WF, Balsam LB, Farouque HM, Caffarelli AD, Robbins RC, Fitzgerald PJ, et al. Novel index for invasively assessing the coronary microcirculation. Circulation. 2003; 107:3129–3132.
Article26. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging. 2002; 18:539–542.
Article27. Engblom H, Hedström E, Heiberg E, Wagner GS, Pahlm O, Arheden H. Size and transmural extent of first-time reperfused myocardial infarction assessed by cardiac magnetic resonance can be estimated by 12-lead electrocardiogram. Am Heart J. 2005; 150:920.
Article28. Mahrholdt H, Wagner A, Holly TA, Elliott MD, Bonow RO, Kim RJ, et al. Reproducibility of chronic infarct size measurement by contrast-enhanced magnetic resonance imaging. Circulation. 2002; 106:2322–2327.
Article29. Lim HS, Yoon MH, Tahk SJ, Yang HM, Choi BJ, Choi SY, et al. Usefulness of the index of microcirculatory resistance for invasively assessing myocardial viability immediately after primary angioplasty for anterior myocardial infarction. Eur Heart J. 2009; 30:2854–2860.
Article30. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.
Article31. American College of Emergency Physicians. Society for Cardiovascular Angiography and Interventions. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 61:485–510.32. Taniyama Y, Ito H, Iwakura K, Masuyama T, Hori M, Takiuchi S, et al. Beneficial effect of intracoronary verapamil on microvascular and myocardial salvage in patients with acute myocardial infarction. J Am Coll Cardiol. 1997; 30:1193–1199.
Article33. Micari A, Belcik TA, Balcells EA, Powers E, Wei K, Kaul S, et al. Improvement in microvascular reflow and reduction of infarct size with adenosine in patients undergoing primary coronary stenting. Am J Cardiol. 2005; 96:1410–1415.
Article34. Amit G, Cafri C, Yaroslavtsev S, Fuchs S, Paltiel O, Abu-Ful A, et al. Intracoronary nitroprusside for the prevention of the no-reflow phenomenon after primary percutaneous coronary intervention in acute myocardial infarction. A randomized, double-blind, placebo-controlled clinical trial. Am Heart J. 2006; 152:887.
Article35. Ito N, Nanto S, Doi Y, Sawano H, Masuda D, Yamashita S, et al. High index of microcirculatory resistance level after successful primary percutaneous coronary intervention can be improved by intracoronary administration of nicorandil. Circ J. 2010; 74:909–915.
Article36. Kubica A, Kozinski M, Navarese EP, Grzesk G, Goch A, Kubica J. Intracoronary versus intravenous abciximab administration in STEMI patients: overview of current status and open questions. Curr Med Res Opin. 2011; 27:2133–2144.
Article37. Romagnoli E, Burzotta F, Trani C, Biondi-Zoccai GG, Giannico F, Crea F. Rationale for intracoronary administration of abciximab. J Thromb Thrombolysis. 2007; 23:57–63.
Article38. Navarese EP, Kozinski M, Obonska K, Margheri M, Gurbel PA, Kubica J, et al. Clinical efficacy and safety of intracoronary vs. intravenous abciximab administration in STEMI patients undergoing primary percutaneous coronary intervention: a meta-analysis of randomized trials. Platelets. 2012; 23:274–281.
Article39. Shimada YJ, Nakra NC, Fox JT, Kanei Y. Meta-analysis of prospective randomized controlled trials comparing intracoronary versus intravenous abciximab in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2012; 109:624–628.40. Thiele H, Wöhrle J, Hambrecht R, Rittger H, Birkemeyer R, Lauer B, et al. Intracoronary versus intravenous bolus abciximab during primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction: a randomised trial. Lancet. 2012; 379:923–931.41. De Luca G, Verdoia M, Suryapranata H. Benefits from intracoronary as compared to intravenous abciximab administration for STEMI patients undergoing primary angioplasty: a meta-analysis of 8 randomized trials. Atherosclerosis. 2012; 222:426–433.
Article42. Poli A, Fetiveau R, Vandoni P, del Rosso G, D'Urbano M, Seveso G, et al. Integrated analysis of myocardial blush and ST-segment elevation recovery after successful primary angioplasty: real-time grading of microvascular reperfusion and prediction of early and late recovery of left ventricular function. Circulation. 2002; 106:313–318.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracoronary Catheter Aspiration Can Be an Adequate Option in Patients with Acute Myocardial Infarction Caused by Left Atrial Myxoma
- A Case of Acute Myocardial Infarction Associated with Myocardial Bridge Treated by Primary Coronary Stenting
- Intracoronary Thrombolysis and Delayed Percutaneous Coronary Intervention for the Treatment of Large Coronary Thrombi in a Patient with Polycythemia Vera
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography
- Phantom Ischemia Mimicking ST Segment Elevation Myocardial Infarction in Fulminant Myocarditis