Lab Med Online.
2013 Jul;3(3):174-177. 10.3343/lmo.2013.3.3.174.
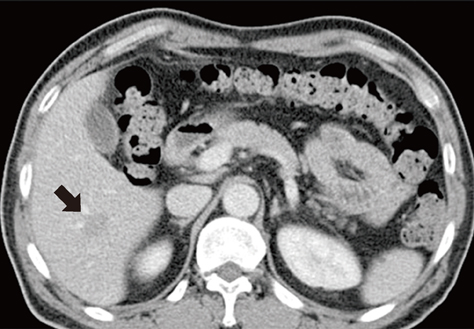
Liver Abscess Caused by Edwardsiella tarda: A Case Report
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yjpk@catholic.ac.kr
- 2Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2053553
- DOI: http://doi.org/10.3343/lmo.2013.3.3.174
Abstract
- Edwardsiella tarda is a member of the family Enterobacteriaceae, commonly found in tropical and subtropical aquatic environments. Most E. tarda infections are linked to exposure to water or animals that inhabit water. However, it is still an uncommon pathogen in humans and causes mainly watery diarrhea. We describe a case of liver abscess caused by E. tarda. A 60-yr-old Korean man, with underlying diabetes mellitus, had a 10-day stay in Egypt 15 days before presentation. Ultrasound-guided percutaneous transhepatic abscess aspiration was performed. Pus culture revealed E. tarda, which was susceptible to all the antibiotics commonly used against Gram-negative organisms. The patient was treated with cefobactam for 10 days and piperacillin/tazobactam for another 5 days combined with an additional abscess aspiration due to recurrent fever. This therapy led to clinical improvement. The possible source of infection in this case may have been the drinking water supplied during travel in Egypt, but we cannot completely rule out a domestic source, because a liver abscess caused by E. tarda has been reported in a Japanese patient without travel history. Considering the Korean custom of eating raw fish or shrimp, climate changes, and increasing international travel, infections due to E. tarda may increase in Korea. Clinical microbiologists should be aware of this potential pathogen, and prompt investigation of the infection source and site is needed.
Keyword
MeSH Terms
Figure
Reference
-
1. Ha J, Choi SP, Lee WH, Yoo SS, Kim HJ, Kim TH, et al. A clinical study on pyogenic liver abscesses: the changes in the clinical features during the recent 12 years. Korean J Med. 2008; 74:37–50.2. Choi HY, Cheon GJ, Kim YD, Han KH, Kim KS, Nah BK. Comparison of clinical characteristics between cryptogenic and biliary pyogenic liver abscess. Korean J Gastroenterol. 2007; 49:238–244.3. Park JH, Lee TH, Kim ST, Jung JH, Kim YS, Kim SM, et al. Clinical features of pyogenic liver abscess according to age group. Korean J Gastroenterol. 2010; 56:90–96.
Article4. Ewing WH, Mcwhorter AC, Escobar MR, Lubin AH. Edwardsiella, a new genus of Enterobacteriaceae based on a new species, E. tarda. Int Bull Bacteriol Nomencl Taxon. 1965; 15:33–38.
Article5. Koshi G, Lalitha MK. Edwardsiella tarda in a variety of human infections. Indian J Med Res. 1976; 64:1753–1759.6. Slaven EM, Lopez FA, Hart SM, Sanders CV. Myonecrosis caused by Edwardsiella tarda: a case report and case series of extraintestinal E. tarda infections. Clin Infect Dis. 2001; 32:1430–1433.
Article7. Janda JM, Abbott SL. Infections associated with the genus Edwardesiella: the role of Edwardsiella tarda in human disease. Clin Infect Dis. 1993; 17:742–748.8. Jordan GW, Hadley WK. Human infection with Edwardsiella tarda. Ann Intern Med. 1969; 70:283–288.9. Jaruratanasirikul S, Kalnauwakul S. Edwardsiella tarda: A causative agent in human infections. Southeast Asian J Trop Med Public Health. 1991; 22:30–34.10. Nelson JJ, Nelson CA, Carter JE. Extraintestinal manifestations of Edwardsiella tarda infection: a 10-year retrospective review. J La State Med Soc. 2009; 161:103–106.11. Wilson JP, Waterer RR, Wofford JD Jr, Chapman SW. Serious infections with Edwardsiella tarda. A case report and review of the literature. Arch Intern Med. 1989; 149:208–210.
Article12. Ota T, Nakano Y, Nishi M, Matsuno S, Kawashima H, Nakagawa T, et al. A case of liver abscess caused by Edwardsiella tarda. Intern Med. 2011; 50:1439–1442.13. Wang IK, Kuo HL, Chen YM, Lin CL, Chang HY, Chuang FR, et al. Extraintestinal manifestations of Edwardsiella tarda infection. Int J Clin Pract. 2005; 59:917–921.14. Thomsen RW, Jepsen P, Sørensen HT. Diabetes mellitus and pyogenic liver abscess: risk and prognosis. Clin Infect Dis. 2007; 44:1194–1201.
Article15. Mowbray EE, Buck G, Humbaugh KE, Marshall GS. Maternal colonization and neonatal sepsis caused by Edwardsiella tarda. Pediatrics. 2003; 111:296–298.16. Kourany M, Vasquez MA, Saenz R. Edwardsiellosis in man and animals in Panamá: clinical and epidemiological characteristics. Am J Trop Med Hyg. 1977; 26:1183–1190.
Article17. Stock I, Wiedemann B. Natural antibiotic susceptibilities of Edwardsiella tarda, E. ictaluri, and E. hoshinae. Antimicrob Agents Chemother. 2001; 45:2245–2255.
Article18. Yousuf RM, How SH, Amran M, Hla KT, Shah A, Francis A. Edwardsiella tarda septicemia with underlying multiple liver abscesses. Malays J Pathol. 2006; 28:49–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of a multiplex PCR assay to detect Edwardsiella tarda, Streptococcus parauberis, and Streptococcus iniae in olive flounder (Paralichthys olivaceus)
- Case Report of Treatment of IVlultiloculated Liver Abscess: Administration of Urokinase Through Drainage Catheter
- Antimicrobial property of lemongrass (Cymbopogon citratus) oil against pathogenic bacteria isolated from pet turtles
- Liver Cirrhosis Induced by Porphyria Cutanea Tarda: A Case Report and Review
- Multiple Liver Abscesses Associated with Ventriculoperitoneal Shunt Infection: Case Report and Review of the Literature