Tuberc Respir Dis.
2007 Nov;63(5):423-429. 10.4046/trd.2007.63.5.423.
The Effect and Safety of Alveolar Recruitment Maneuver using Pressure-Controlled Ventilation in Acute Lung Injury and Acute Respiratory Distress Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. ysamkim@yuhs.ac
- 2Institute of Chest Disease, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea.
- KMID: 2050475
- DOI: http://doi.org/10.4046/trd.2007.63.5.423
Abstract
-
BACKGROUND: Alveolar recruitment (RM) is one of the primary goals of respiratory care for an acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). The purposes of alveolar recruitment are an improvement in pulmonary gas exchange and the protection of atelectrauma. This study examined the effect and safety of the alveolar RM using pressure control ventilation (PCV) in early ALI and ARDS patients.
METHODS
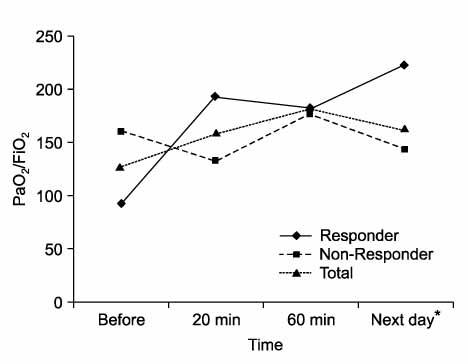
Sixteen patients with early ALI and ARDS who underwent alveolar RM using PCV were enrolled in this study. The patients' data were recorded at the baseline, and 20 minutes, and 60 minutes after alveolar RM, and on the next day after the maneuver. Alveolar RM was performed with an inspiratory pressure of 30 cmH2O and a PEEP of 20 cmH2O in a 2-minute PCV mode. The venous O2 saturation, central venous pressure, blood pressure, pulse rate, PaO2/FiO2 ratio, PEEP, and chest X-ray findings were obtained before and after alveolar RM.
RESULTS
Of the 16 patients, 3 had extra-pulmonary ALI/ARDS and the remaining 13 had pulmonary ALI/ARDS. The mean PEEP was 11.3 mmHg, and the mean PaO2/FiO2 ratio was 130.3 before RM. The PaO2/FiO2 ratio increased by 45% after alveolar RM. The PaO2/FiO2 ratio reached a peak 60 minutes after alveolar RM. The PaCO2 increased by 51.9 mmHg after alveolar RM. The mean blood pressure was not affected by alveolar RM. There were no complications due to pressure injuries such as a pneumothorax, pneumomediastinum, and subcutaneous emphysema.
CONCLUSION
In this study, alveolar RM using PCV improved the level of oxygenation in patients with an acute lung injury and acute respiratory distress syndrome. Moreover, there were no significant complications due to hemodynamic changes and pressure injuries. Therefore, alveolar RM using PCV can be applied easily and safely in clinical practice with lung protective strategy in early ALI and ARDS patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998. 388:347–354.2. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000. 342:1301–1308.3. Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with acute respiratory distress syndrome. N Engl J Med. 2004. 351:327–336.4. Girard TD, Bernard GR. Mechanical Ventilation in ARDS: a state-of-the-art review. Chest. 2007. 131:921–929.5. Lim SC, Adams AB, Simonson DA, Dries DJ, Broccard AF, Hotchkiss JR, et al. Intercomparison of recruitment maneuver efficacy in three models of acute lung injury. Crit Care Med. 2004. 32:2371–2377.6. Lim SC, Adams AB, Simonson DA, Dries DJ, Broccard AF, Hotchkiss JR, et al. Transient hemodynamic effects of recruitment maneuvers in three experimental models of acute lung injury. Crit Care Med. 2004. 32:2378–2384.7. Bellingan GJ. The pulmonary physician in critical care - 6: the pathogenesis of ALI/ARDS. Thorax. 2002. 57:540–546.8. Artigas A, Bernard GR, Carlet J, Dreyfuss D, Gattinoni L, Hudson L, et al. The American-European Consensus Conference on ARDS, part 2. Ventilatory, pharmacologic, supportive therapy, study design strategies and issues related to recovery and remodeling. Intensive Care Med. 1998. 24:378–398.9. Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventilatory strategies increases cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest. 1997. 99:944–952.10. Lim CM, Jung H, Koh Y, Lee JS, Shim TS, Lee SD, et al. Effect of alveolar recruitment maneuver in early acute respiratory distress syndrome according to anti-derecruitment strategy, etiological category of diffuse lung injury, and body position of the patient. Crit Care Med. 2003. 31:411–418.11. Kim HC, Cho DH, Kang GW, Park DJ, Lee JD, Hwang YS. Difference of short term survival in patients with ARDS according to responsiveness to alveolar recruitment. Tuberc Respir Dis. 2004. 56:280–288.12. Villagra A, Ochagavia A, Vatua S, Murias G, Del Mar, Lopez Aguilar J, et al. Recruitment maneuvers during lung protective ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2002. 165:165–170.13. Tugrul S, Cakar N, Akinci O, Ozcan PE, Disci R, Esen F, et al. Time required for equilibration of arterial oxygen pressure after setting optimal positive end-expiratory pressure in acute respiratory distress syndrome. Crit Care Med. 2005. 33:995–1000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Recruiting Maneuvers in a Patient with Acute Lung Injury after Femoral Nailing: A case report
- Ventilator-Induced Lung Injury
- The Effects of Repetitive Alveolar Recruitment on Oxygenation and Compliance in ARDS Patients
- Ventilator-Induced Lung Injury
- Difference of Short Term Survival in Patients with ARDS According to Responsiveness to Alveolar Recruitment