Clin Endosc.
2013 May;46(3):251-259. 10.5946/ce.2013.46.3.251.
Unusual Complications Related to Endoscopic Retrograde Cholangiopancreatography and Its Endoscopic Treatment
- Affiliations
-
- 1Digestive Disease Center, CHA Bundang Medical Center, CHA University, Seongnam, Korea. bluehipp@cha.ac.kr
- KMID: 2048930
- DOI: http://doi.org/10.5946/ce.2013.46.3.251
Abstract
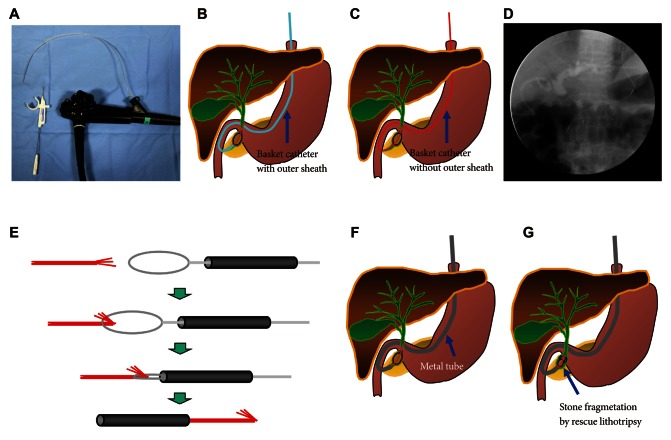
- Endoscopic retrograde cholangiopancreatography (ERCP)-induced complications, once occurred, can lead to significant morbidity. Commonly 5% to 10% of patients experience procedure related complications such as post-ERCP pancreatitis, biliary hemorrhage, and cholangitis, in descending order. However, complications such as perforation, pneumothorax, air embolism, splenic injury, and basket impaction are rare but are associated with high mortality if occurred. Such unexpected unusual complications might extend the length of hospitalization, require urgent surgical intervention, and put the patient in miserable condition leading to permanent disability or mortality. Although these ERCP-induced complications can be minimized by a skilled operator using advanced techniques and devices, the occurrence of unusual complications are hard to expect and induce very difficult management condition. In this review, we will focus on the uncommon complications related to ERCP. This review is also aimed at suggesting optimal endoscopic treatment strategies for several complications based on our institutional experiences.
MeSH Terms
Figure
Cited by 3 articles
-
Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
Jaihwan Kim
Clin Endosc. 2017;50(4):334-339. doi: 10.5946/ce.2017.068.Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
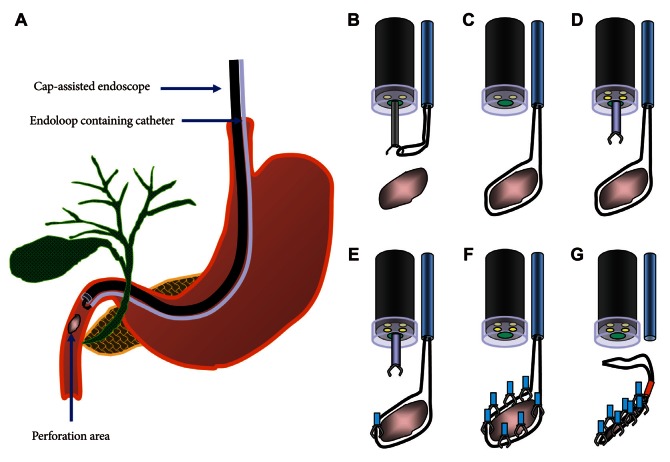
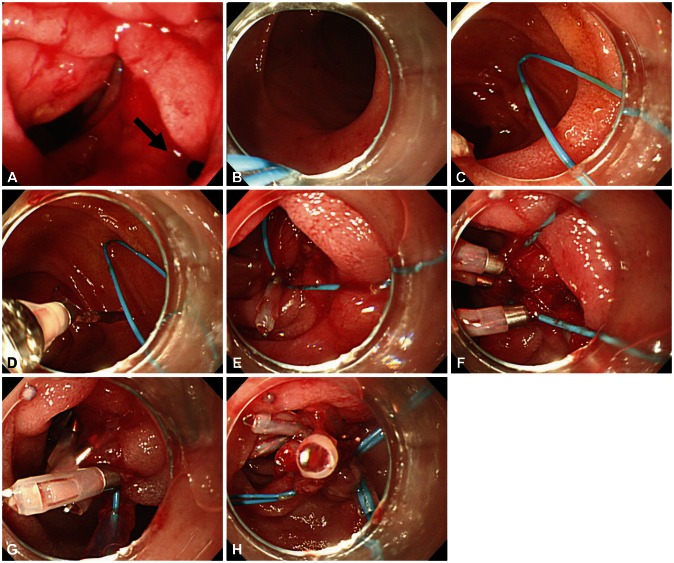
Seon Mee Park
Clin Endosc. 2016;49(4):376-382. doi: 10.5946/ce.2016.088.Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Tae Hoon Lee, Joung-Ho Han, Sang-Heum Park
Clin Endosc. 2013;46(5):522-528. doi: 10.5946/ce.2013.46.5.522.
Reference
-
1. Aliperti G. Complications related to diagnostic and therapeutic endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 1996; 6:379–407. PMID: 8673333.
Article2. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.
Article3. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID: 8782497.
Article4. Kahaleh M, Freeman M. Prevention and management of post-endoscopic retrograde cholangiopancreatography complications. Clin Endosc. 2012; 45:305–312. PMID: 22977824.
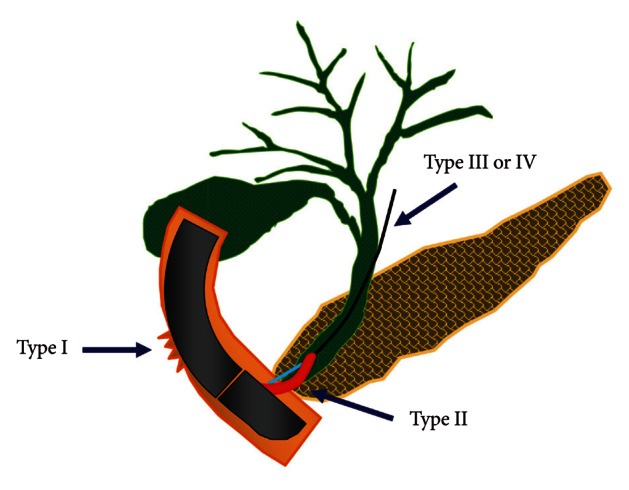
Article5. Machado NO. Management of duodenal perforation post-endoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article. JOP. 2012; 13:18–25. PMID: 22233942.6. Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000; 232:191–198. PMID: 10903596.
Article7. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298. PMID: 11932784.
Article8. Howard TJ, Tan T, Lehman GA, et al. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999; 126:658–663. PMID: 10520912.
Article9. Baron TH, Gostout CJ, Herman L. Hemoclip repair of a sphincterotomy-induced duodenal perforation. Gastrointest Endosc. 2000; 52:566–568. PMID: 11023583.
Article10. Genzlinger JL, McPhee MS, Fisher JK, Jacob KM, Helzberg JH. Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am J Gastroenterol. 1999; 94:1267–1270. PMID: 10235205.
Article11. Katsinelos P, Paroutoglou G, Papaziogas B, Beltsis A, Dimiropoulos S, Atmatzidis K. Treatment of a duodenal perforation secondary to an endoscopic sphincterotomy with clips. World J Gastroenterol. 2005; 11:6232–6234. PMID: 16273659.
Article12. Vezakis A, Fragulidis G, Nastos C, Yiallourou A, Polydorou A, Voros D. Closure of a persistent sphincterotomy-related duodenal perforation by placement of a covered self-expandable metallic biliary stent. World J Gastroenterol. 2011; 17:4539–4541. PMID: 22110286.
Article13. Park WY, Cho KB, Kim ES, Park KS. A case of ampullary perforation treated with a temporally covered metal stent. Clin Endosc. 2012; 45:177–180. PMID: 22866262.
Article14. Nam HS, Kim GH, Kim DU, et al. A case of duodenal perforation caused by biliary plastic stent treated with approximation using endoclip and detachable snare. Korean J Gastroenterol. 2011; 57:129–133. PMID: 21350325.
Article15. Seibert DG. Use of an endoscopic clipping device to repair a duodenal perforation. Endoscopy. 2003; 35:189. PMID: 12561015.
Article16. Sebastian S, Byrne AT, Torreggiani WC, Buckley M. Endoscopic closure of iatrogenic duodenal perforation during endoscopic ultrasound. Endoscopy. 2004; 36:245. PMID: 14986227.
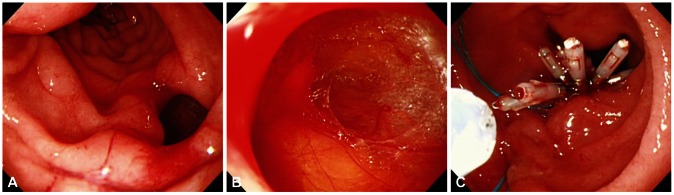
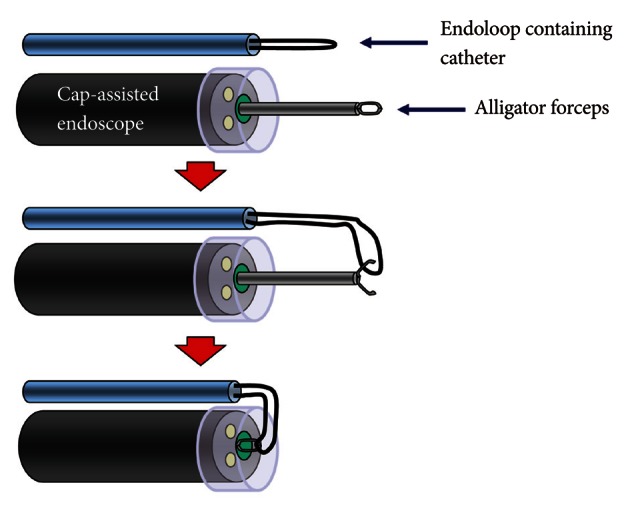
Article17. Lee TH, Bang BW, Jeong JI, et al. Primary endoscopic approximation suture under cap-assisted endoscopy of an ERCP-induced duodenal perforation. World J Gastroenterol. 2010; 16:2305–2310. PMID: 20458771.
Article18. Endo M, Inomata M, Terui T, et al. New endoscopic technique to close large mucosal defects after endoscopic mucosal resection in patients with gastric mucosal tumors. Dig Endosc. 2004; 16:372–375.
Article19. Matsuda T, Fujii T, Emura F, et al. Complete closure of a large defect after EMR of a lateral spreading colorectal tumor when using a two-channel colonoscope. Gastrointest Endosc. 2004; 60:836–838. PMID: 15557972.
Article20. Sanders MK, Malick J, Fasanella KE, Watson AR. Endoscopic closure of iatrogenic duodenal perforation during EUS in a patient with unusual anatomy. Gastrointest Endosc. 2008; 68:802–804. PMID: 18513724.
Article21. Kim DH, Kwon CI, Chung JG, et al. Endoscopic hemostasis with multiple hemoclips and an endoloop for uncontrolled peptic ulcer bleeding. Endoscopy. 2011; 43(Suppl 2 UCTN):E3–E4. PMID: 21271528.
Article22. Schepers NJ, van Buuren HR. Pneumothorax following ERCP: report of four cases and review of the literature. Dig Dis Sci. 2012; 57:1990–1995. PMID: 22466080.
Article23. Al-Ashaal YI, Hefny AF, Safi F, Abu-Zidan FM. Tension pneumothorax complicating endoscopic retrograde cholangiopancreatography: case report and systematic literature review. Asian J Surg. 2011; 34:46–49. PMID: 21515213.
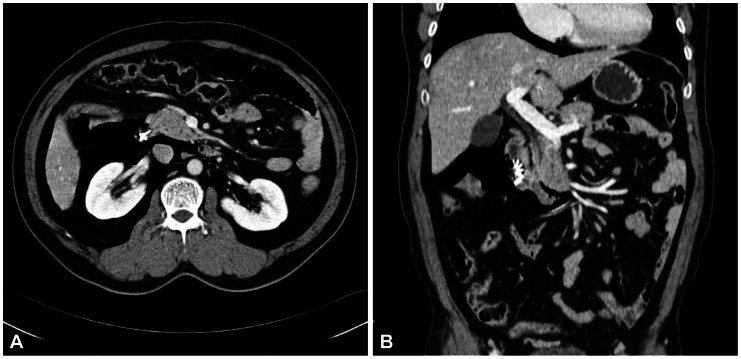
Article24. Ortega Deballon P, Fernández Lobato R, García Septiem J, Nieves Vázquez MA, Martínez Santos C, Moreno Azcoita M. Liver hematoma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 2000; 14:767. PMID: 11287996.25. Del Pozo D, Moral I, Poves E, Sanz C, Martín M. Subcapsular hepatic hematoma following ERCP: case report and review. Endoscopy. 2011; 43(Suppl 2 UCTN):E164–E165. PMID: 21563064.
Article26. Nayagam J, Ho KM, Liang J. Fatal systemic air embolism during endoscopic retrograde cholangio-pancreatography. Anaesth Intensive Care. 2004; 32:260–264. PMID: 15957727.
Article27. Kennedy C, Larvin M, Linsell J. Fatal hepatic air embolism following ERCP. Gastrointest Endosc. 1997; 45:187–188. PMID: 9041008.
Article28. Cha ST, Kwon CI, Seon HG, et al. Fatal biliary-systemic air embolism during endoscopic retrograde cholangiopancreatography: a case with multifocal liver abscesses and choledochoduodenostomy. Yonsei Med J. 2010; 51:287–290. PMID: 20191026.
Article29. Kalaitzakis E, Stern N, Sturgess R. Portal vein cannulation: an uncommon complication of endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2011; 17:5131–5132. PMID: 22171149.
Article30. Furuzono M, Hirata N, Saitou J, Nakaji S. A rare complication during ERCP and sphincterotomy: placement of an endoscopic nasobiliary drainage tube in the portal vein. Gastrointest Endosc. 2009; 70:588–590. PMID: 19555937.
Article31. Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR. Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc. 2012; 75:221–223. PMID: 21470606.
Article32. Zyromski NJ, Camp CM. Splenic injury: a rare complication of endoscopic retrograde cholangiopancreatography. Am Surg. 2004; 70:737–739. PMID: 15328812.33. Deist TJ, Freytag A. Splenic rupture after ERCP. Z Gastroenterol. 2003; 41:579–582. PMID: 12806544.34. Lo AY, Washington M, Fischer MG. Splenic trauma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 1994; 8:692–693. PMID: 8059310.
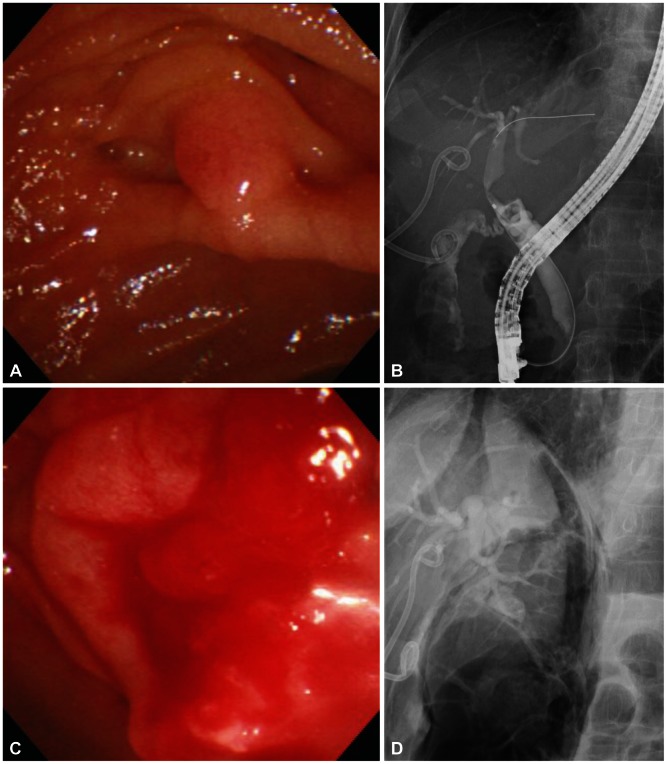
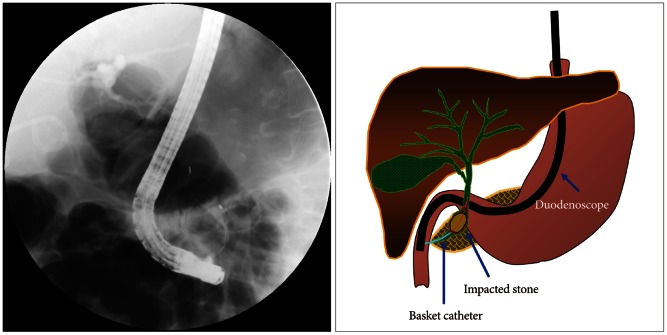
Article35. Payne WG, Norman JG, Pinkas H. Endoscopic basket impaction. Am Surg. 1995; 61:464–467. PMID: 7733558.36. Kim WH, Kwon CI, Han JH. Rescue lithotripsy to treat basket impaction. Endoscopy. 2012; 44(Suppl 2 UCTN):E209–E210. PMID: 22622749.
Article37. Katsinelos P, Fasoulas K, Beltsis A, et al. Large-balloon dilation of the biliary orifice for the management of basket impaction: a case series of 6 patients. Gastrointest Endosc. 2011; 73:1298–1301. PMID: 21492853.
Article38. Kwon JH, Lee JK, Lee JH, Lee YS. Percutaneous transhepatic release of an impacted lithotripter basket and its fractured traction wire using a goose-neck snare: a case report. Korean J Radiol. 2011; 12:247–251. PMID: 21430943.
Article39. Attila T, May GR, Kortan P. Nonsurgical management of an impacted mechanical lithotriptor with fractured traction wires: endoscopic intracorporeal electrohydraulic shock wave lithotripsy followed by extraendoscopic mechanical lithotripsy. Can J Gastroenterol. 2008; 22:699–702. PMID: 18701948.
Article40. Fukino N, Oida T, Kawasaki A, et al. Impaction of a lithotripsy basket during endoscopic lithotomy of a common bile duct stone. World J Gastroenterol. 2010; 16:2832–2834. PMID: 20533607.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation
- Basic knowledge of endoscopic retrograde cholangiopancreatography
- Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
- Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
- Preparation of High-Risk Patients and the Choice of Guidewire for a Successful Endoscopic Retrograde Cholangiopancreatography Procedure