J Korean Neuropsychiatr Assoc.
2015 Aug;54(3):316-321. 10.4306/jknpa.2015.54.3.316.
Comparisons of Depressive Symptoms of the Hamilton Depression Rating Scale between Elderly and Non-Elderly Outpatients with Major Depressive Disorder
- Affiliations
-
- 1Department of Psychiatry, Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jeonhj@skku.edu
- 2Department of Health Sciences & Technology, Department of Clinical Research Design and Evaluation, and Department of Medical Device Management and Research, Samsung Advanced Institute for Health Sciences & Technology (SAIHST), Seoul, Korea.
- 3Depression Clinical and Research Program, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
- KMID: 2035965
- DOI: http://doi.org/10.4306/jknpa.2015.54.3.316
Abstract
OBJECTIVES
Previous studies have reported that symptoms of patients with major depressive disorder (MDD) are different according to age groups, and the Hamilton Depression Rating Scale (HDRS) is the most widely used measure to evaluate the symptoms of MDD. However, few previous studies have compared the symptoms of HDRS between the elderly and non-elderly groups.
METHODS
The study population consisted of 574 subjects with MDD who were > or =18 years old, evaluated using the Mini International Neuropsychiatric Interview and 17 items of HDRS. Differences between two groups were analyzed using independent t-test. A multivariate logistic regression model was used to evaluate associations between age and 17 items from HDRS after controlling for gender, years of education, marital status, and employment status.
RESULTS
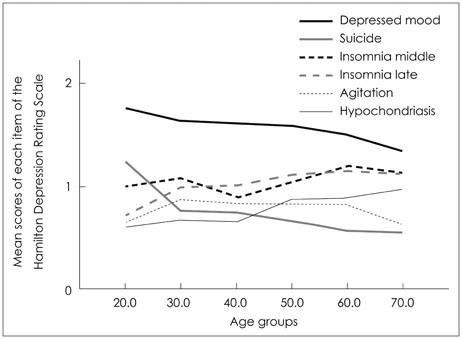
Among 574 patients with MDD, there were 80 elderly patients (age> or =65) and 494 non-elderly patients (age between 18 and 64). Elderly patients had higher scores on item 5 (middle insomnia) (t=-2.271, p=0.024) and item 6 (late insomnia) (t=-2.280, p=0.023), whereas they had lower scores on item 1 (depressed mood) (t=2.860, p=0.004), item 3 (suicide) (t=2.258, p=0.024), and item 9 (agitation) (t=2.031, p=0.043), although no significant difference in the total HDRS scores was observed between elderly and non-elderly. Multivariate logistic regression showed significant association of elderly with hypochondriasis [adjusted odds ratio (AOR)=1.894, 95% confidence interval (CI) 1.01-3.56] and agitation (AOR=0.50, 95% CI 0.29-0.87).
CONCLUSION
Elderly MDD patients showed more insomnia and hypochondriasis and less depressed mood, suicidal ideation, and agitation than non-elderly.
MeSH Terms
Figure
Reference
-
1. Cho MJ, Park JI, Bae A, Bae JN, Sohn JW, Ahn JH, et al. The epidemiological survey of mental disorders in Korea [Internet]. Seoul: Seoul National University College of Medicine;2011. cited 2014 Oct 6. Available from: http://www.google.co.kr/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCIQFjAA&url=http%3A%2F%2Fstat.mw.go.kr%2Ffront%2Finclude%2Fdownload.jsp%3FbbsSeq%3D13%26nttSeq%3D18458%26atchSeq%3D3026&ei=shYqVJKXEoeE8gWkk4GADg&usg=AFQjCNGSD11Yht8HJQLZnkYnvaRS14aYlQ&bvm=bv.76477589,d.dGc&cad=rjt.2. Parkar SR. Elderly mental health: needs. Mens Sana Monogr. 2015; 13:91–99.
Article3. Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock's Synopsis of Psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer Health;2014.4. Arai H, Ouchi Y, Yokode M, Ito H, Uematsu H, Eto F, et al. Toward the realization of a better aged society: messages from gerontology and geriatrics. Geriatr Gerontol Int. 2012; 12:16–22.
Article5. Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF 3rd, Alexopoulos GS, Bruce ML, et al. Diagnosis and treatment of depression in late life. Consensus statement update. JAMA. 1997; 278:1186–1190.
Article6. Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED. Older age and the underreporting of depressive symptoms. J Am Geriatr Soc. 1995; 43:216–221.
Article7. Gottfries CG. Is there a difference between elderly and younger patients with regard to the symptomatology and aetiology of depression? Int Clin Psychopharmacol. 1998; 13:Suppl 5. S13–S18.
Article8. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association;2013.9. VanItallie TB. Subsyndromal depression in the elderly: underdiagnosed and undertreated. Metabolism. 2005; 54:5 Suppl 1. 39–44.
Article10. Beheydt LL, Schrijvers D, Docx L, Bouckaert F, Hulstijn W, Sabbe B. Psychomotor retardation in elderly untreated depressed patients. Front Psychiatry. 2015; 5:196.
Article11. Shahpesandy H. Different manifestation of depressive disorder in the elderly. Neuro Endocrinol Lett. 2005; 26:691–695.12. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003; 160:1147–1156.
Article13. Tan LL, Ng LL, Tan S, Roy K, Brodaty H, Parker G. Depression in Singapore: failure to demonstrate an age effect on clinical features. Int J Geriatr Psychiatry. 2001; 16:1054–1060.
Article14. Hong SW, Lee DS, Jae YM, Jang SH, Choi JH, Jang YK, et al. Comparison of Depressive Symptoms of Major Depressive Disorder between Elderly and Non-Elderly Group in Busan City in South Korea. J Korean Soc Biol Ther Psychiatry. 2008; 14:58–63.15. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967; 6:278–296.
Article16. Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE Jr, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000; 157:1873–1875.
Article17. Angst J, Adolfsson R, Benazzi F, Gamma A, Hantouche E, Meyer TD, et al. The HCL-32: towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord. 2005; 88:217–233.
Article18. Oh MY, Angst J, Sung TH, Lee EH, Hong KS, Lee DS, et al. Reliability and validity of the Hypomania Symptom Checklist-32 in Korea. Korean J Clin Psychol. 2009; 28:321–338.
Article19. Jon DI, Hong N, Yoon BH, Jung HY, Ha K, Shin YC, et al. Validity and reliability of the Korean version of the Mood Disorder Questionnaire. Compr Psychiatry. 2009; 50:286–291.
Article20. Salzman C. Pharmacologic treatment of depression in the elderly. J Clin Psychiatry. 1993; 54:Suppl. 23–28.21. Livingston G, Watkin V, Milne B, Manela MV, Katona C. The natural history of depression and the anxiety disorders in older people: the Islington community study. J Affect Disord. 1997; 46:255–262.
Article22. Sloan EP, Flint AJ, Reinish L, Shapiro CM. Circadian rhythms and psychiatric disorders in the elderly. J Geriatr Psychiatry Neurol. 1996; 9:164–170.
Article23. Leblanc MF, Desjardins S, Desgagné A. The relationship between sleep habits, anxiety, and depression in the elderly. Nat Sci Sleep. 2015; 7:33–42.24. Leblanc MF, Desjardins S, Desgagné A. Sleep cognitions associated with anxiety and depression in the elderly. Clin Interv Aging. 2015; 10:575–582.25. Lôo H, Gallarda T, Fabre I, Olié JP. [Depression and aging]. Bull Acad Natl Med. 2004; 188:999–1007. discussion 1007-101026. DeLamater J, Karraker A. Sexual functioning in older adults. Curr Psychiatry Rep. 2009; 11:6–11.
Article27. Lyness JM, Kim J, Tang W, Tu X, Conwell Y, King DA, et al. The clinical significance of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2007; 15:214–223.
Article28. Small GW. Differential diagnoses and assessment of depression in elderly patients. J Clin Psychiatry. 2009; 70:e47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Symptoms between Early and Late Onset Depression in Elderly Depressive Patients in Korea
- Comorbid Anxiety in Elderly Patients with Depression
- Symptom Patterns of Depressive Disorder in the Elderly Medical Inpatients: Focused on Major Depressive Disorder
- Folate Augmentation Therapy in Depression
- Comparison of Effect of SSRIs and SNRIs on Depression, Pain and Somatic Symptoms in Elderly Patients with Major Depressive Disorder