Korean Circ J.
2009 Oct;39(10):414-417. 10.4070/kcj.2009.39.10.414.
Perinatal Changes in Size of the Fetal Great Arteries
- Affiliations
-
- 1Department of Pediatrics, Ewha Womans University School of Medicine, Seoul, Korea. hyesk@ewha.ac.kr
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2028921
- DOI: http://doi.org/10.4070/kcj.2009.39.10.414
Abstract
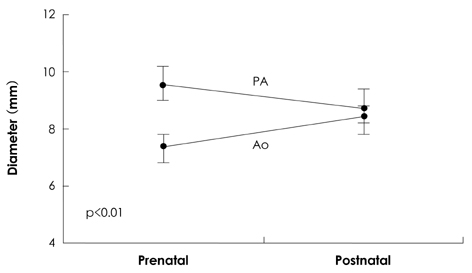
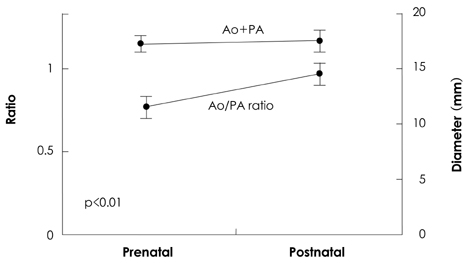
- BACKGROUND AND OBJECTIVES
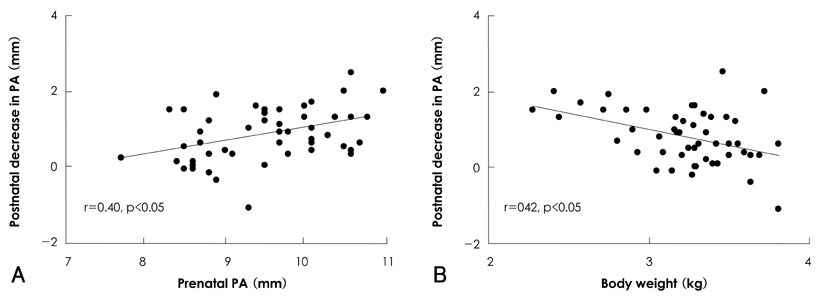
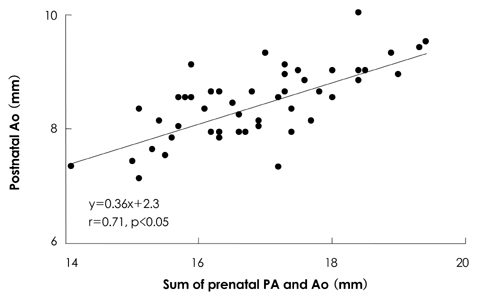
At birth, the fetal circulation must immediately adapt to extrauterine life. Our goal was to evaluate perinatal changes in the size of the aorta (Ao) and pulmonary artery (PA), and to investigate factors influencing these changes. SUBJECTS AND METHODS: Aortic and PA diameters were measured by echocardiography in 50 healthy term babies one day before and 4 to 5 days after birth. RESULTS: Compared with prenatal measurements, the Ao increased (from 7.4+/-0.6 mm to 8.4+/-0.6 mm, p<0.01) and the PA decreased (from 9.5+/-0.8 mm to 8.7+/-0.8 mm, p<0.01) in size after birth. The Ao/PA ratio increased from 0.78+/-0.07 before birth to 0.97+/-0.08 after birth (p<0.01), but there was no significant difference in the sum of the diameters of the great arteries between pre- and postnatal measurements. Postnatal increases in aortic size correlated negatively with prenatal aortic diameter (r=-0.37, p<0.05), but was not related to body weight. According to multiple regression analysis, significant variables for predicting perinatal changes in size of the Ao and PA were the prenatal Ao/PA ratio and the prenatal PA diameter, respectively. CONCLUSION: Despite a difference existing in prenatal diameters between Ao and PA, circulatory changes at birth make the great artery sizes equal, and do so regardless of body weight.
Keyword
Figure
Reference
-
1. Hong JS, Choi JY, Zhu L, et al. Echocardiographic assessment of left ventricular diastolic function in transitional circulation period. Korean Circ J. 2006. 36:652–660.2. Achiron R, Golan-Porat N, Gabbay U, et al. In utero ultrasonographic measurements of fetal aortic and pulmonary artery diameters during the first half of gestation. Ultrasound Obstet Gynecol. 1998. 11:180–184.3. Sahn DJ, Lange LW, Allen HD, et al. Quantitative real-time corss-sectional echocardiography in the developing normal human fetus and newborn. Circulation. 1980. 62:588–597.4. Shapiro I, Degani S, Leibovitz Z, Ohel G, Tal Y, Abinader EG. Fetal cardiac measurements derived by transvaginal and transabdominal cross-sectional echocardiography from 14 weeks of gestation to term. Ultrasound Obstet Gynecol. 1998. 12:404–418.5. Sharland GK, Allan LD. Normal fetal cardiac measurements derived by cross-sectional echocardiography. Ultrasound Obstet Gynecol. 1992. 2:175–181.6. Tan J, Silverman NH, Hoffman JI, Villegas M, Schmidt KG. Cardiac dimensions determined by cross-sectional echocardiography in the normal human fetus from 18 weeks to term. Am J Cardiol. 1992. 70:1459–1467.7. Winsberg F. Echocardiography of the fetal and newborn heart. Invest Radiol. 1972. 7:152–158.8. Wladimiroff JW, Vosters R, McGhie JS. Normal cardiac ventricular geometry and function during the last trimester of pregnancy and early neonatal period. Br J Obstet Gynaecol. 1982. 89:839–844.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prenatal diagnosis of transposition of the great arteries: an updated review
- Perinatal Stroke Associated with Placental Chorioangioma: A Rare Case and Review of Literature
- Transposition of the Great Arteries: Historical Background
- Prenatal screening of DiGeorge (22q11.2 deletion) syndrome by abnormalities of the great arteries among Thai pregnant women
- Natural Course and Treatment of Fetal Ovarian Cysts