J Periodontal Implant Sci.
2014 Jun;44(3):109-117. 10.5051/jpis.2014.44.3.109.
Improvement in periodontal healing after periodontal surgery supported by nutritional supplement drinks
- Affiliations
-
- 1Department of Medical Nutrition, Graduate School of East-West Medical Science, Kyung Hee University, Yongin, Korea. ypark@khu.ac.kr dentall@yuhs.ac
- 2Department of Periodontology, Research Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea. ypark@khu.ac.kr dentall@yuhs.ac
- KMID: 2012985
- DOI: http://doi.org/10.5051/jpis.2014.44.3.109
Abstract
- PURPOSE
The aim of this study was to determine the effects of nutritional supplements on periodontal health and tooth mobility after surgery.
METHODS
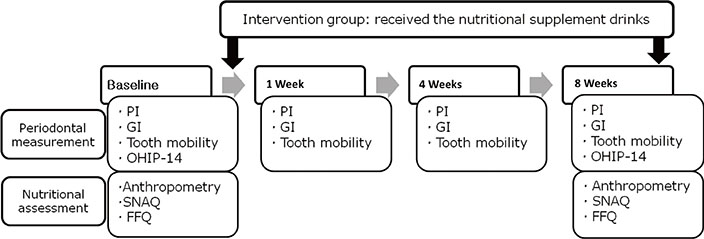
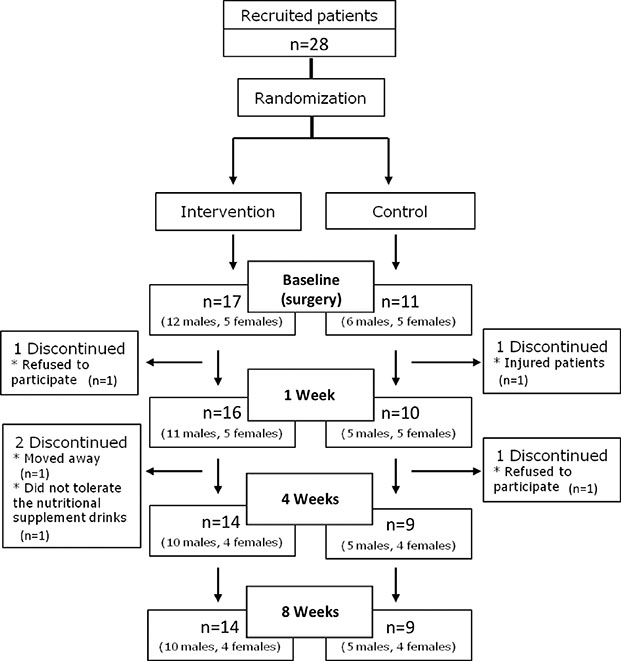
Patients were randomly assigned to an intervention group who consumed nutritional supplement drinks for 8 weeks, while the placebo group did not receive any such supplements. The gingival index (GI) and tooth mobility were measured at baseline and at 1, 4, and 8 weeks. In addition, the oral health impact profile-14 and anthropometric measurements along with loss of appetite and dietary intake were assessed at baseline and 8 weeks.
RESULTS
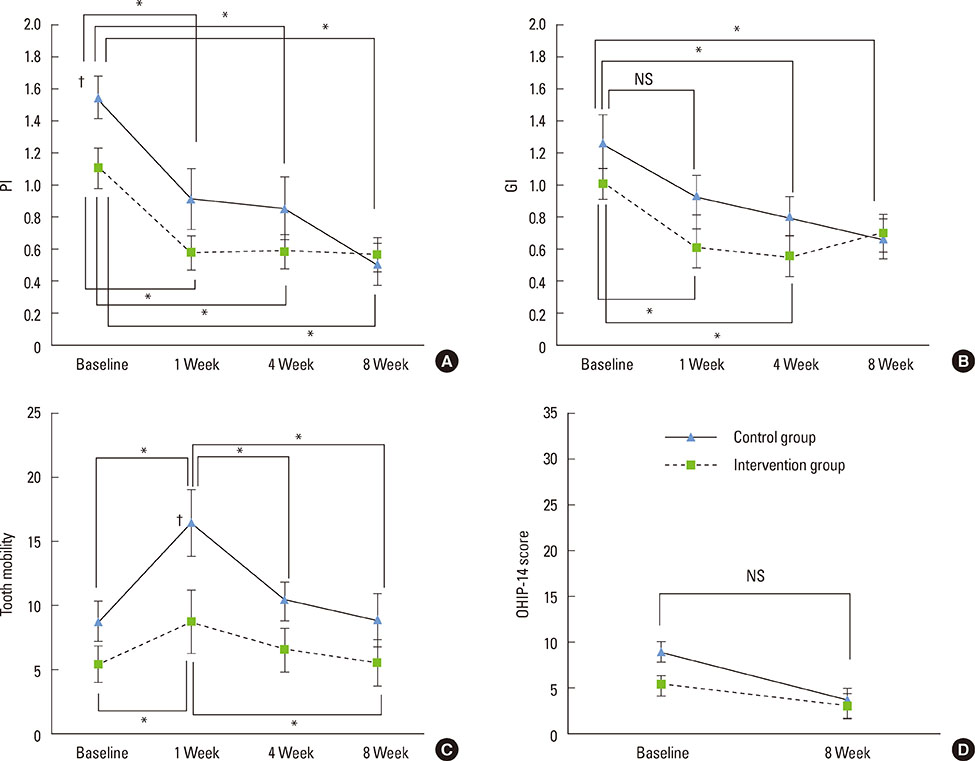
At 1 week, GI values were reduced in the intervention group (P<0.05), and tooth mobility had increased, but to a lesser extent in the intervention group (P<0.05). At 8 weeks, the intakes of protein, vitamins A and B1, and niacin were increased in the intervention group.
CONCLUSIONS
These results demonstrate that nutritional supplementation improves early periodontal healing after surgery.
MeSH Terms
Figure
Cited by 1 articles
-
Use of Oral Nutritional Supplements for Patients with Diabetes
Mi Ra Kang
J Korean Diabetes. 2017;18(3):181-188. doi: 10.4093/jkd.2017.18.3.181.
Reference
-
1. Jenzsch A, Eick S, Rassoul F, Purschwitz R, Jentsch H. Nutritional intervention in patients with periodontal disease: clinical, immunological and microbiological variables during 12 months. Br J Nutr. 2009; 101:879–885.
Article2. Choi YK, Do SR, Park DY. Change in number of outpatients with periodontal diseases during recent 20 years based on patient survey. J Korean Acad Oral Health. 2011; 35:331–339.3. Canakci CF, Canakci V. Pain experienced by patients undergoing differentperiodontal therapies. J Am Dent Assoc. 2007; 138:1563–1573.4. Pereira LJ, Gazolla CM, Magalhaes IB, Dominguete MH, Vilela GR, Castelo PM, et al. Influence of periodontal treatment on objective measurement of masticatory performance. J Oral Sci. 2012; 54:151–157.
Article5. Fleszar TJ, Knowles JW, Morrison EC, Burgett FG, Nissle RR, Ramfjord SP. Tooth mobility and periodontal therapy. J Clin Periodontol. 1980; 7:495–505.
Article6. Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol. 1994; 65:25–29.
Article7. Alkan A, Keskiner I, Arici S, Sato S. The effect of periodontal surgery on bite force, occlusal contact area and bite pressure. J Am Dent Assoc. 2006; 137:978–983.
Article8. Feller L, Lemmer J. Tooth mobility after periodontal surgery. SADJ. 2004; 59:407409–411.9. Kerry GJ, Morrison EC, Ramfjord SP, Hill RW, Caffesse RG, Nissle RR, et al. Effect of periodontal treatment on tooth mobility. J Periodontol. 1982; 53:635–638.
Article10. Budtz-Jorgensen E, Chung JP, Rapin CH. Nutrition and oral health. Best Pract Res Clin Gastroenterol. 2001; 15:885–896.
Article11. Tanaka K, Miyake Y, Sasaki S, Ohya Y, Matsunaga I, Yoshida T, et al. Relationship between intake of vegetables, fruit, and grains and the prevalence of tooth loss in Japanese women. J Nutr Sci Vitaminol (Tokyo). 2007; 53:522–528.
Article12. Van der Velden U, Kuzmanova D, Chapple IL. Micronutritional approaches to periodontal therapy. J Clin Periodontol. 2011; 38:Suppl 11. 142–158.
Article13. Neiva RF, Steigenga J, Al-Shammari KF, Wang HL. Effects of specific nutrients on periodontal disease onset, progression and treatment. J Clin Periodontol. 2003; 30:579–589.
Article14. San Miguel SM, Opperman LA, Allen EP, Zielinski J, Svoboda KK. Bioactive antioxidant mixtures promote proliferation and migration on human oral fibroblasts. Arch Oral Biol. 2011; 56:812–822.
Article15. De Marchi RJ, Hugo FN, Hilgert JB, Padilha DM. Association between oral health status and nutritional status in south Brazilian independent-living older people. Nutrition. 2008; 24:546–553.
Article16. Wouters-Wesseling W, Van Hooijdonk C, Wagenaar L, Bindels J, de Groot L, Van Staveren W. The effect of a liquid nutrition supplement on body composition and physical functioning in elderly people. Clin Nutr. 2003; 22:371–377.
Article17. Collins CE, Kershaw J, Brockington S. Effect of nutritional supplements on wound healing in home-nursed elderly: a randomized trial. Nutrition. 2005; 21:147–155.
Article18. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.
Article19. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.
Article20. Tanaka E, Ueki K, Kikuzaki M, Yamada E, Takeuchi M, Dalla-Bona D, et al. Longitudinal measurements of tooth mobility during orthodontic treatment using a periotest. Angle Orthod. 2005; 75:101–105.21. Bae KH, Kim HD, Jung SH, Park DY, Kim JB, Paik DI, et al. Validation of the Korean version of the oral health impact profile among the Korean elderly. Community Dent Oral Epidemiol. 2007; 35:73–79.
Article22. Wilson MM, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, et al. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr. 2005; 82:1074–1081.
Article23. Ahn YJ, Lee JE, Paik HY, Lee HK, Jo IH, Kim KC. Development of a semi-quantitative food frequency questionnaire based on dietary data from the Korea National Health and Nutrition Examination Survey. Korean J Nutr. 2003; 6:173–184.24. Alfano MC. Controversies, perspectives, and clinical implications of nutrition in periodontal disease. Dent Clin North Am. 1976; 20:519–548.25. Woolfe SN, Kenney EB, Hume WR, Carranza FA Jr. Relationship of ascorbic acid levels of blood and gingival tissue with response to periodontal therapy. J Clin Periodontol. 1984; 11:159–165.
Article26. Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012; 11:278–296.
Article27. Seifter E, Crowley LV, Rettura G, Nakao K, Gruber C, Kan D, et al. Influence of vitamin A on wound healing in rats with femoral fracture. Ann Surg. 1975; 181:836–841.
Article28. Staudte H, Sigusch BW, Glockmann E. Grapefruit consumption improves vitamin C status in periodontitis patients. Br Dent J. 2005; 199:213–217.
Article29. Leggott PJ, Robertson PB, Rothman DL, Murray PA, Jacob RA. The effect of controlled ascorbic acid depletion and supplementation on periodontal health. J Periodontol. 1986; 57:480–485.
Article30. Neiva RF, Al-Shammari K, Nociti FH Jr, Soehren S, Wang HL. Effects of vitamin-B complex supplementation on periodontal wound healing. J Periodontol. 2005; 76:1084–1091.
Article31. Collins TM, Denish A, Sheffield J, Mitra A, Stueber K, Smith YR. Nicotinamide enhances skin flap survival. Scand J Plast Reconstr Surg Hand Surg. 1989; 23:177–179.
Article32. Vaxman F, Olender S, Lambert A, Nisand G, Aprahamian M, Bruch JF, et al. Effect of pantothenic acid and ascorbic acid supplementation on human skin wound healing process. A double-blind, prospective and randomized trial. Eur Surg Res. 1995; 27:158–166.
Article33. Wikesjo UM, Nilveus RE, Selvig KA. Significance of early healing events on periodontal repair: a review. J Periodontol. 1992; 63:158–165.
Article34. Alkan A, Keskiner I, Arici S, Sato S. The effect of periodontitis on biting abilities. J Periodontol. 2006; 77:1442–1445.
Article35. Lindhe J, Nyman S. Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol. 1984; 11:504–514.
Article36. Wong RM, Ng SK, Corbet EF, Keung Leung W. Non-surgical periodontal therapy improves oral health-related quality of life. J Clin Periodontol. 2012; 39:53–61.
Article37. Bosley BN, Weiner DK, Rudy TE, Granieri E. Is chronic nonmalignant pain associated with decreased appetite in older adults? Preliminary evidence. J Am Geriatr Soc. 2004; 52:247–251.
Article38. Wood N, Johnson RB, Streckfus CF. Comparison of body composition and periodontal disease using nutritional assessment techniques: Third National Health and Nutrition Examination Survey (NHANES III). J Clin Periodontol. 2003; 30:321–327.
Article39. Kong YM, Han GS. Relationships between obesity types and periodontitis according to characteristics of subjects. J Dent Hyg Sci. 2012; 12:279–286.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient-reported outcome measures on intake of nutrition drink for nutritional supplements after periodontal surgery
- Waiting for innovations in periodontal disease diagnosis
- Reply on "Relationship between maternal periodontal disease and Apgar score of newborns"
- Future endeavors needed to close the socioeconomic gap in periodontal health
- Opening a new chapter of Journal of Periodontal & Implant Science