J Periodontal Implant Sci.
2014 Jun;44(3):102-108. 10.5051/jpis.2014.44.3.102.
Long-term implant success at the Academy for Oral Implantology: 8-year follow-up and risk factor analysis
- Affiliations
-
- 1Academy for Oral Implantology, Vienna, Austria. pommer@implantatakademie.at
- KMID: 2012984
- DOI: http://doi.org/10.5051/jpis.2014.44.3.102
Abstract
- PURPOSE
Rehabilitation of the incomplete dentition by means of osseointegrated dental implants represents a highly predictable and widespread therapy; however, little is known about potential risk factors that may impair long-term implant success.
METHODS
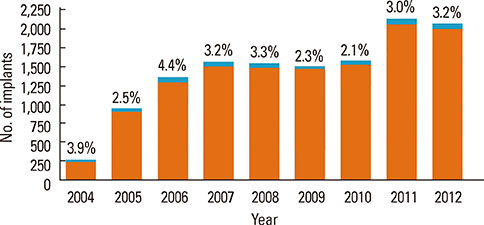
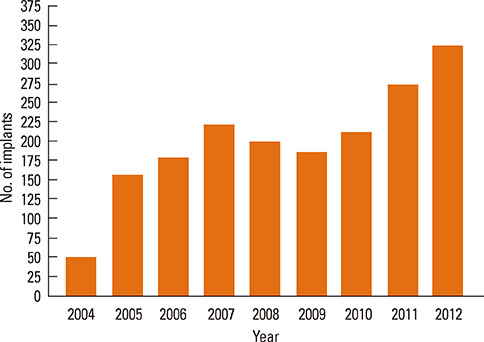
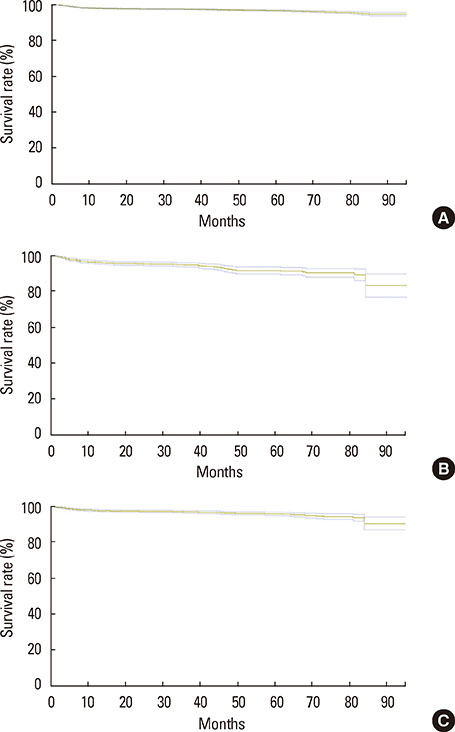
From 2004 to 2012, a total of 13,147 implants were placed in 4,316 patients at the Academy for Oral Implantology in Vienna. The survival rates after 8 years of follow-up were computed using the Kaplan-Meier method, and the impact of patient- and implant-related risk factors was assessed.
RESULTS
Overall implant survival was 97% and was not associated with implant length (P=0.930), implant diameter (P=0.704), jaw location (P=0.545), implant position (P=0.450), local bone quality (P=0.398), previous bone augmentation surgery (P=0.617), or patient-related factors including osteoporosis (P=0.661), age (P=0.575), or diabetes mellitus (P=0.928). However, smoking increased the risk of implant failure by 3 folds (P<0.001) and a positive history of periodontal disease doubled the failure risk (P=0.001).
CONCLUSIONS
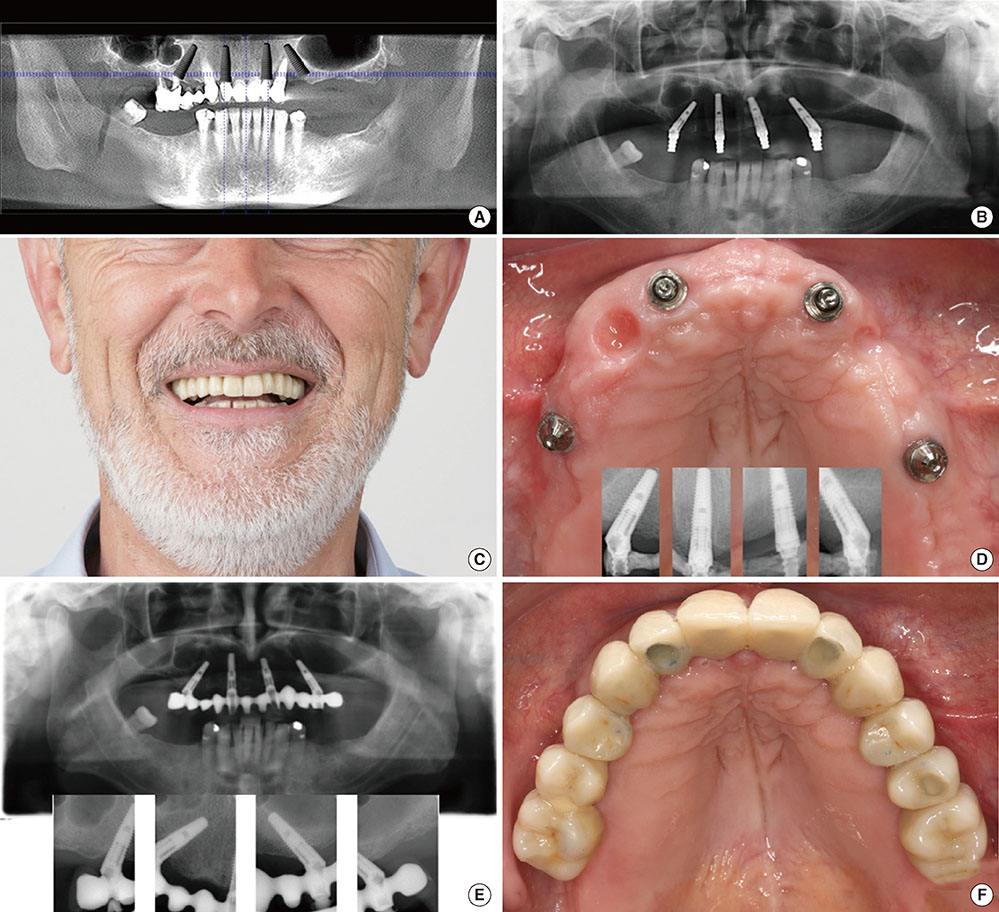
Summing up the long-term results of well over 10,000 implants at the Academy for Oral Implantology in Vienna it can be concluded that there is only a limited number of patients that do not qualify for implant therapy and may thus not benefit from improved quality of life associated with fixed implant-retained prostheses.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The feasibility of immediately loading dental implants in edentulous jaws
Anders Henningsen, Ralf Smeets, Aria Wahidi, Lan Kluwe, Frank Kornmann, Max Heiland, Till Gerlach
J Periodontal Implant Sci. 2016;46(4):234-243. doi: 10.5051/jpis.2016.46.4.234.Risk indicators related to peri-implant disease: an observational retrospective cohort study
Pier Paolo Poli, Mario Beretta, Giovanni Battista Grossi, Carlo Maiorana
J Periodontal Implant Sci. 2016;46(4):266-276. doi: 10.5051/jpis.2016.46.4.266.
Reference
-
1. Pommer B, Zechner W, Watzek G, Palmer R. To graft or not to graft? Evidence-based guide to decision making in oral bone graft surgery. In : Zorzi A, Miranda J, editors. Bone Grafting. Rijeka: InTech;2012. p. 159–182.2. Levin L. Dealing with dental implant failures. J Appl Oral Sci. 2008; 16:171–175.
Article3. Palma-Carrio C, Maestre-Ferrín L, Penarrocha-Oltra D, Penarrocha-Diago MA, Penarrocha-Diago M. Risk factors associated with early failure of dental implants: a literature review. Med Oral Patol Oral Cir Bucal. 2011; 16:e514–e517.
Article4. Lee JH, Frias V, Lee KW, Wright RF. Effect of implant size and shape on implant success rates: a literature review. J Prosthet Dent. 2005; 94:377–381.
Article5. Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006; 17:Suppl 2. 136–159.
Article6. Pommer B, Hof M, Fadler A, Gahleitner A, Watzek G, Watzak G. Primary implant stability in the atrophic sinus floor of human cadaver maxillae: impact of residual ridge height, bone density, and implant diameter. Clin Oral Implants Res. 2014; 25:e109–e113.
Article7. Diz P, Scully C, Sanz M. Dental implants in the medically compromised patient. J Dent. 2013; 41:195–206.
Article8. Clementini M, Rossetti PH, Penarrocha D, Micarelli C, Bonachela WC, Canullo L. Systemic risk factors for peri-implant bone loss: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2014; 43:323–334.
Article9. Pommer B, Frantal S, Willer J, Posch M, Watzek G, Tepper G. Impact of dental implant length on early failure rates: a meta-analysis of observational studies. J Clin Periodontol. 2011; 38:856–863.
Article10. Andersen E, Saxegaard E, Knutsen BM, Haanaes HR. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int J Oral Maxillofac Implants. 2001; 16:217–224.11. Polizzi G, Rangert B, Lekholm U, Gualini F, Lindstrom H. Branemark System Wide Platform implants for single molar replacement: clinical evaluation of prospective and retrospective materials. Clin Implant Dent Relat Res. 2000; 2:61–69.
Article12. Arisan V, Bolukbasi N, Ersanli S, Ozdemir T. Evaluation of 316 narrow diameter implants followed for 5-10 years: a clinical and radiographic retrospective study. Clin Oral Implants Res. 2010; 21:296–307.
Article13. Atwood DA. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971; 26:266–279.
Article14. Lekholm U, Zarb GA. Patient selection and preparation. In : Branemark PI, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence;1985. p. 199–220.15. Charyeva O, Altynbekov K, Zhartybaev R, Sabdanaliev A. Long-term dental implant success and survival: a clinical study after an observation period up to 6 years. Swed Dent J. 2012; 36:1–6.16. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10-16-year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010; 21:772–777.
Article17. Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002; 29:Suppl 3. 197–212.
Article18. Monje A, Chan HL, Fu JH, Suarez F, Galindo-Moreno P, Wang HL. Are short dental implants (<10 mm) effective? A meta-analysis on prospective clinical trials. J Periodontol. 2013; 84:895–904.
Article19. Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res. 2012; 23:515–525.
Article20. Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Kuchler I. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007; 34:523–544.
Article21. Safii SH, Palmer RM, Wilson RF. Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: a systematic review and meta-analysis. Clin Implant Dent Relat Res. 2010; 12:165–174.
Article22. Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 12–27.23. Salvi GE, Carollo-Bittel B, Lang NP. Effects of diabetes mellitus on periodontal and peri-implant conditions: update on associations and risks. J Clin Periodontol. 2008; 35:8 Suppl. 398–409.
Article24. Chao YL, Chen HH, Mei CC, Tu YK, Lu HK. Meta-regression analysis of the initial bone height for predicting implant survival rates of two sinus elevation procedures. J Clin Periodontol. 2010; 37:456–465.
Article25. Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, et al. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2010; (3):CD008397.
Article26. Graziani F, Donos N, Needleman I, Gabriele M, Tonetti M. Comparison of implant survival following sinus floor augmentation procedures with implants placed in pristine posterior maxillary bone: a systematic review. Clin Oral Implants Res. 2004; 15:677–682.
Article27. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008; 35:8 Suppl. 216–240.
Article28. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007; 22:Suppl. 49–70.29. Bernstein S, Cooke J, Fotek P, Wang HL. Vertical bone augmentation: where are we now? Implant Dent. 2006; 15:219–228.
Article30. Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 237–259.31. Clementini M, Morlupi A, Canullo L, Agrestini C, Barlattani A. Success rate of dental implants inserted in horizontal and vertical guided bone regenerated areas: a systematic review. Int J Oral Maxillofac Surg. 2012; 41:847–852.
Article32. Donos N, Mardas N, Chadha V. Clinical outcomes of implants following lateral bone augmentation: systematic assessment of available options (barrier membranes, bone grafts, split osteotomy). J Clin Periodontol. 2008; 35:8 Suppl. 173–202.
Article33. Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 218–236.34. Rocchietta I, Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. J Clin Periodontol. 2008; 35:8 Suppl. 203–215.
Article35. Waasdorp J, Reynolds MA. Allogeneic bone onlay grafts for alveolar ridge augmentation: a systematic review. Int J Oral Maxillofac Implants. 2010; 25:525–531.36. Sbordone L, Toti P, Menchini-Fabris G, Sbordone C, Guidetti F. Implant survival in maxillary and mandibular osseous onlay grafts and native bone: a 3-year clinical and computerized tomographic follow-up. Int J Oral Maxillofac Implants. 2009; 24:695–703.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Criteria for Dental Implant Success: A Systematic Literature Review
- Implant Placement on a Cementoosseous Dysplastic Mandible with a Long-term Follow-up: A Case Report
- Surgical Removal of Dental Implants Dislocated Into the Mandibular Body
- Horizontal ridge augmentation with porcine bone-derived grafting material: a long-term retrospective clinical study with more than 5 years of follow-up
- Retrospective Observational Study of Narrow Diameter Implants