Current Status of the Continuity of Ambulatory Diabetes Care and its Impact on Health Outcomes and Medical Cost in Korea Using National Health Insurance Database
- Affiliations
-
- 1Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus of Korean Diabetes Association, Korea.
- 2Department of Research, Health Insurance Review Agency, Korea.
- 3Department of Internal Medicine, College of Medicine, Eulji University, Korea.
- 4Department of Internal Medicine, Pochon CHA University, Korea.
- 5Department of Endocrinology, Gachon University of Science and Medicine, Gil Medical Center, Korea.
- 6Department of Internal Medicine, Pusan Paik Hospital, Inje College of Medicine, Korea.
- 7Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University, Korea.
- 8Department of Internal Medicine, The Catholic University of Korea, Korea.
- 9Department of Internal Medicine, Yonsei University College of Medicine, Korea.
- 10Division of Endocrinology and Metabolism, Ewha Womans University College of Medicine, Korea.
- 11Department of Biostatistics, College of Medicine, Korea University, Korea.
- 12Department of Internal Medicine, Wonju College of Medicine, Yonsei University, Korea.
- 13Department of Endocrinology and Metabolism, Ajou University School of Medicine, Korea.
- KMID: 2008268
- DOI: http://doi.org/10.4093/jkda.2006.30.5.377
Abstract
-
BACKGROUND: The continuity of care in chronic diseases, especially in diabetes, was emphasized from many studies. But large scale studies with long-term observation which confirm the impact of continuity of care on health outcomes are rare. This study tried national level 3 year observation to find differences in hospitalization, mortality and medical costs among patient groups with different utilization pattern.
METHODS
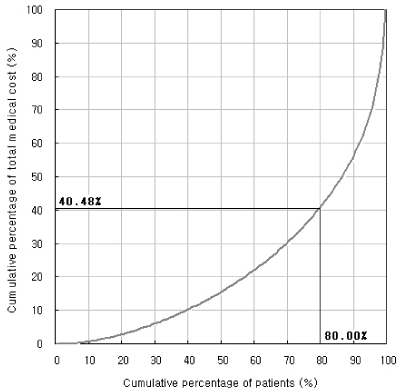
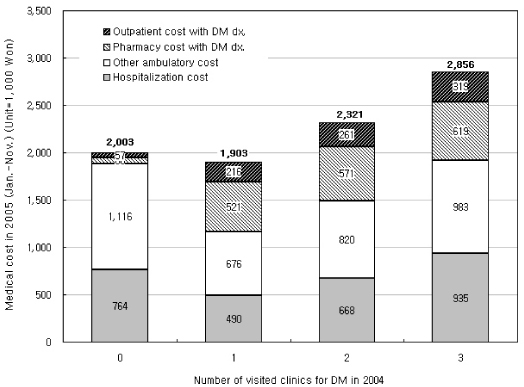
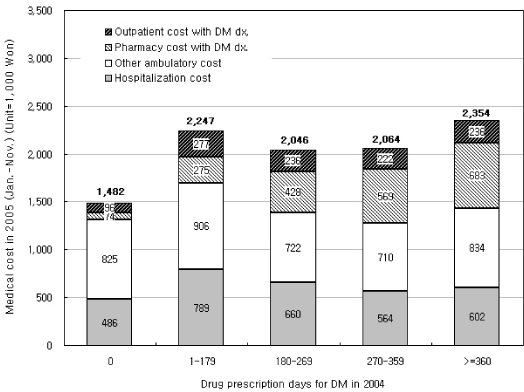
The 1,088,564 patients with diabetes diagnosis and diabetes drug prescription in 2002, from 20 to 79 years old, and survived until the end of 2004 were included. Annual drug prescription days, number of visited clinics and quarterly continuity of care were measured. Gender, age group, living area, health insurance premium level (as a proxy of the income level), years of first DM diagnosis, five co-morbidities (hypertension, heart disease, stroke, renal disease, admission with DM), hospitalization experience and the type of main attending clinic were adjusted. Hospitalization, mortality and high costs group (top quintile) in 2005 were predicted by multiple logistic regression model.
RESULTS
Patients who failed in continuity of care in 2003 and 2004 showed higher hospitalization (OR =1.29), higher mortality (OR =1.75) and they are more likely to be high costs group (OR =1.34) in 2005 than who fulfilled the continuity of care. Patients who have single attending clinic also showed lower hospitalization, lower mortality and lower cost. Completeness in diabetic drug prescription were correlated with lower hospitalization, lower mortality but with higher cost. Possible cost saving from continual care with single attending clinic was estimated at Won 417 billion (Dollar 1 = Won 943.7). Possible expenditure from complete drug prescription was Won 228 billion. So, net saving was Won 139 billion in our study population.
CONCLUSION
Continual care and single attending clinic saves patient's life and national costs. Fragmented primary care system in Korea should be reformed for more effective care of chronic diseases. National Health Insurance Database in Korea enables nationwide long-term observation study which overcomes the many limitations found in hospital-based studies and cross-sectional surveys.
MeSH Terms
Figure
Cited by 7 articles
-
Continuity of Care for Elderly Patients with Diabetes Mellitus, Hypertension, Asthma, and Chronic Obstructive Pulmonary Disease in Korea
Jae Seok Hong, Hee Chung Kang, Jaiyong Kim
J Korean Med Sci. 2010;25(9):1259-1271. doi: 10.3346/jkms.2010.25.9.1259.Chasms in Achievement of Recommended Diabetes Care among Geographic Regions in Korea
Sanghyun Cho, Ji-Yeon Shin, Hyun Joo Kim, Sang Jun Eun, Sungchan Kang, Won Mo Jang, Hyemin Jung, Yoon Kim, Jin Yong Lee
J Korean Med Sci. 2019;34(31):. doi: 10.3346/jkms.2019.34.e190.Factors associated with the hypertension outpatients' choice of healthcare providers in Korea
Jung Chan Lee, Kye Hyun Kim, Han Nah Kim, Yoon Hyung Park
J Korean Med Assoc. 2011;54(9):961-970. doi: 10.5124/jkma.2011.54.9.961.Factors associated with diabetes outpatient use of tertiary or general hospitals as their usual source of care in Korea
Jung Chan Lee, Kye Hyun Kim, Han Nah Kim, Nam Soon Kim
J Korean Med Assoc. 2012;55(12):1215-1225. doi: 10.5124/jkma.2012.55.12.1215.Strategies for improvement of primary care in Korea
Heui Sug Jo
J Korean Med Assoc. 2012;55(10):959-968. doi: 10.5124/jkma.2012.55.10.959.Factors associated with Hospitalization among Patients with Diabetes Mellitus
Mi Ra Guk, Ja Yun Choi
Korean J Adult Nurs. 2017;29(1):1-11. doi: 10.7475/kjan.2017.29.1.1.Impact of Continuous Care on Health Outcomes and Cost for Type 2 Diabetes Mellitus: Analysis Using National Health Insurance Cohort Database
Ji Hyun Nam, Changwoo Lee, Nayoung Kim, Keun Young Park, Jeonghoon Ha, Jaemoon Yun, Dong Wook Shin, Euichul Shin
Diabetes Metab J. 2019;43(6):776-784. doi: 10.4093/dmj.2018.0189.
Reference
-
1. International Diabetes Federation. Diabetes Atlas. 2003. 2nd ed.2. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000. 321:405–412.3. Vijan S, Stevens DI, Herman WH, Funnel MN, Stanford CJ. Screeing, preventing, counseling, and treatment for the complications of type II diabetes mellitus: putting evidence into practice. J Gen Intern Med. 1997. 12:567–580.4. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993. 329:977–986.5. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.6. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, Rhodes S, Shekelle P. Meta-analysis: Chronic disease self-management programs for older adults. Ann Intern Med. 2005. 143:427–438.7. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2001. 24:S33–S43.9. Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions, Qual Saf Healt. Care. 2004. 13:299–305.10. Ibrahim MA, Saviz LA, Carey TS, Wagner EH. Population-based health principles in medical and public health practice. Journal of Public Health Management and Practice. 2001. 7:75–81.11. Norris SL, Glasgow RE, Engelgau MM, O'Connor PJ, McCulloch D. Chronic Disease Management -A Definition and Systematic Approach To Component Interventions. Dis Manage Health Outcomes. 2003. 11:477–488.12. Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetics and heart failure teams. Ann Behav Med. 2002. 27:80–87.13. WHO Noncommunicable Disease and Mental Health. Innovative care for chronic conditions: building blocks for action: global report. 2002. WHO.14. Desai J, Geiss L, Mukhtar Q, Harwell T, Benjamin S, Bell R, Tierney E. Public health surveillance of diabetes in United States. Journal of Public Health Management and Practice. 2003. Suppl. S44–S51.16. National Quality Forum. Pay-for-performance programs: Guiding principles and design strategies-Conference proceedings. 2005.17. Darden PM, Ector W, Moran C, Quattlebaum TG. Comparison of continuity in resident versus private practice. Pediatrics. 2001. 108:1263–1268.21. Starfield B. Longitudinality and Managed Care. Primary Care: Concepts, Evaluation, and Policy. 1992. New York: Oxford University Press. Inc;41–55.22. Center for Chronic Disease Prevention and Control. Diabetes in Canada. 2002. Health Canada.23. American Diabetes Association. Standards of Medical Care in Diabetes. Diabetes Care. 2004. 27:S15–S35.26. Diabetes care analysis-savings estimate. Bridges to Excellence. 2005. Available at http://www.bridgestoexcellence.org/pdf/DCL_analysis1207051.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic Characteristics of Diabetes Mellitus in Korea: Current Status of Diabetic Patients Using Korean Health Insurance Database
- Continuity of Care for Elderly Patients with Diabetes Mellitus, Hypertension, Asthma, and Chronic Obstructive Pulmonary Disease in Korea
- Effects of Continuity of Care on Diabetes-Related Avoidable Hospitalizations among Middle- and Old-Aged Patients: Analysis of National Health Insurance Claims Data
- Associations Between the Continuity of Ambulatory Care of Adult Diabetes Patients in Korea and the Incidence of Macrovascular Complications
- Continuity of Care of Patient with Diabetes and Its Affecting Factors in Korea