J Korean Soc Transplant.
2012 Sep;26(3):188-195. 10.4285/jkstn.2012.26.3.188.
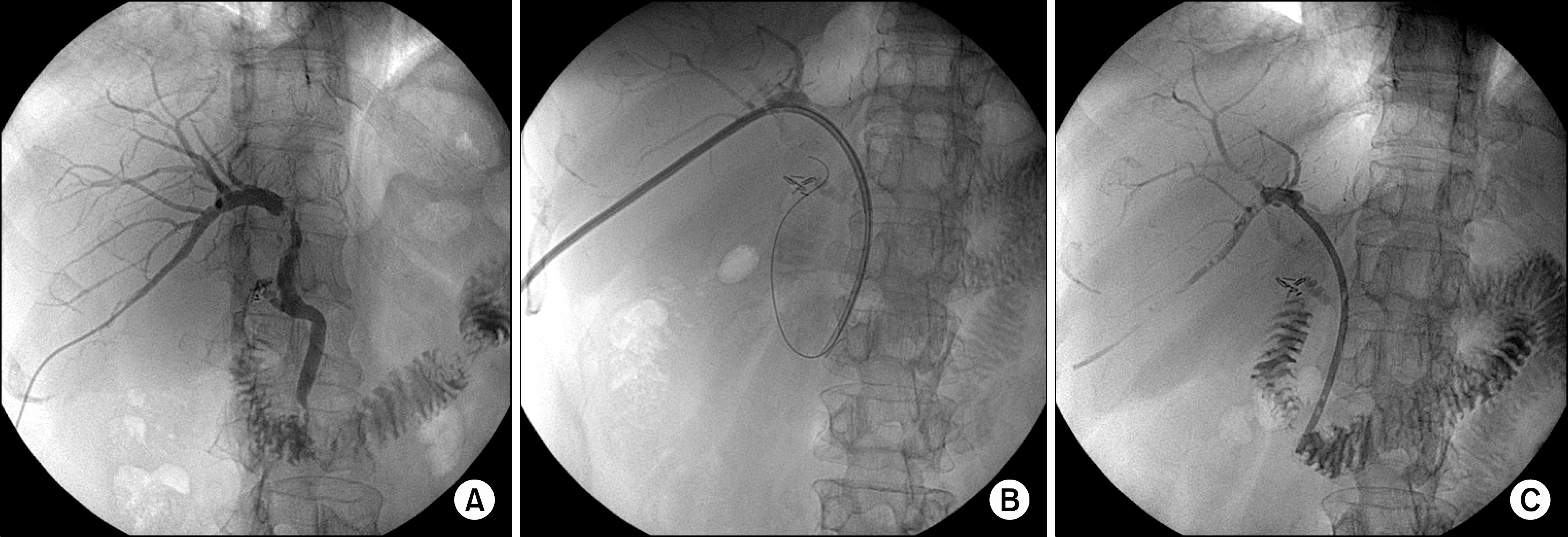
New Strategy in Cases of Failed Endoscopic Intervention of Biliary Strictures after Living Donor Liver Transplantation: Percutaneous Transhepatic Biliary Stent Insertion and Subsequent Endoscopic Treatment
- Affiliations
-
- 1Center for Liver Cancer, National Cancer Center, Goyang, Korea. kwleegs@gmail.com
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2003534
- DOI: http://doi.org/10.4285/jkstn.2012.26.3.188
Abstract
- BACKGROUND
In cases of endoscopic intervention treatment for biliary stricture which fail, a percutaneous approach can be subsequently attempted. However, the quality of life is lower for those patients with percutaneous transhepatic biliary drainage (PTBD) tubes than those with endoscopic retrograde biliary drainage tubes. In this study, we report the outcome of the application of percutaneous transhepatic biliary stenting (PTBS) for use in subsequent endoscopic treatment of biliary stricture after living donor liver transplantation (LDLT).
METHODS
Of 165 patients who underwent LDLT, 40 (24.2%) were diagnosed with anastomotic biliary strictures. Of these patients, seven agreed to treatment using PTBS using a plastic stent with endoscopic follow-up instead of treatment by insertion of a PTBD tube, and were enrolled in this study.
RESULTS
In all seven patients, the use of this technique enabled effective advancement of a guide wire and successful placement of one or two plastic stents (7 or 10 Fr) into the PTBD tract. There were no PTBS-related complications associated with the procedure. The median duration for stent use was 40.3 weeks (range; 27.6~65.0). Upon final removal of all stents, the stricture had been resolved in four (57%) of the seven patients.
CONCLUSIONS
Our study data suggested that, after failed use of ERCP in the treatment of biliary stricture after LDLT, the use of PTBS and ERCP may be an effective and safe treatment.
Keyword
MeSH Terms
Figure
Reference
-
1). Sharma S., Gurakar A., Jabbour N. Biliary strictures following liver transplantation: past, present and preventive strategies. Liver Transpl. 2008. 14:759–69.
Article2). Fondevila C., Ghobrial RM., Fuster J., Bombuy E., Garcia-Valdecasas JC., Busuttil RW. Biliary complications after adult living donor liver transplantation. Transplant Proc. 2003. 35:1902–3.
Article3). Shah SA., Grant DR., McGilvray ID., Greig PD., Selzner M., Lilly LB, et al. Biliary strictures in 130 consecutive right lobe living donor liver transplant recipients: results of a Western center. Am J Transplant. 2007. 7:161–7.
Article4). Tsujino T., Isayama H., Sugawara Y., Sasaki T., Kogure H., Nakai Y, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2006. 101:2230–6.
Article5). Yazumi S., Yoshimoto T., Hisatsune H., Hasegawa K., Kida M., Tada S, et al. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006. 13:502–10.
Article6). Seo JK., Ryu JK., Lee SH., Park JK., Yang KY., Kim YT, et al. Endoscopic treatment for biliary stricture after adult living donor liver transplantation. Liver Transpl. 2009. 15:369–80.
Article7). Lee SH., Ryu JK., Woo SM., Park JK., Yoo JW., Kim YT, et al. Optimal interventional treatment and long-term outcomes for biliary stricture after liver transplantation. Clin Transplant. 2008. 22:484–93.
Article8). Morelli G., Fazel A., Judah J., Pan JJ., Forsmark C., Draganov P. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc. 2008. 67:879–85.
Article9). Pfau PR., Kochman ML., Lewis JD., Long WB., Lucey MR., Olthoff K, et al. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation. Gastrointest Endosc. 2000. 52:55–63.
Article10). Thuluvath PJ., Atassi T., Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int. 2003. 23:156–62.
Article11). Graziadei IW., Schwaighofer H., Koch R., Nachbaur K., Koenigsrainer A., Margreiter R, et al. Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transpl. 2006. 12:718–25.
Article12). Kato H., Kawamoto H., Tsutsumi K., Harada R., Fujii M., Hirao K, et al. Long-term outcomes of endoscopic management for biliary strictures after living donor liver transplantation with duct-to-duct reconstruction. Transpl Int. 2009. 22:914–21.
Article13). Kobayashi T., Sato Y., Shioji K., Yamamoto S., Oya H., Hara Y, et al. Early regular examination of biliary strictures by endoscopic retrograde cholangiography for duct-to-duct biliary reconstruction after adult living donor liver transplantation. Transplant Proc. 2009. 41:268–70.
Article14). Kim ES., Lee BJ., Won JY., Choi JY., Lee DK. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Gastrointest Endosc. 2009. 69:38–46.
Article15). Hisatsune H., Yazumi S., Egawa H., Asada M., Hasegawa K., Kodama Y, et al. Endoscopic management of biliary strictures after duct-to-duct biliary reconstruction in right-lobe living-donor liver transplantation. Transplantation. 2003. 76:810–5.
Article16). Williams ED., Draganov PV. Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol. 2009. 15:3725–33.
Article17). Kimmings AN., van Deventer SJ., Obertop H., Rauws EA., Huibregtse K., Gouma DJ. Endotoxin, cytokines, and endotoxin binding proteins in obstructive jaundice and after preoperative biliary drainage. Gut. 2000. 46:725–31.
Article18). Pascher A., Neuhaus P. Bile duct complications after liver transplantation. Transpl Int. 2005. 18:627–42.
Article19). Park JS., Kim MH., Lee SK., Seo DW., Lee SS., Han J, et al. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003. 57:78–85.
Article20). Calvo MM., Bujanda L., Heras I., Cabriada JL., Bernal A., Orive V, et al. The rendezvous technique for the treatment of choledocholithiasis. Gastrointest Endosc. 2001. 54:511–3.
Article21). Dickey W. Parallel cannulation technique at ERCP rendezvous. Gastrointest Endosc. 2006. 63:686–7.
Article22). Lammer J., Hausegger KA., Flückiger F., Winkelbauer FW., Wildling R., Klein GE, et al. Common bile duct obstruction due to malignancy: treatment with plastic versus metal stents. Radiology. 1996. 201:167–72.
Article23). Mueller PR., Ferrucci JT Jr., Teplick SK., vanSonnenberg E., Haskin PH., Butch RJ, et al. Biliary stent endoprosthesis: analysis of complications in 113 patients. Radiology. 1985. 156:637–9.
Article24). Kahaleh M., Behm B., Clarke BW., Brock A., Shami VM., De La Rue SA, et al. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm (with video)? Gastrointest Endosc. 2008. 67:446–54.
Article25). Cantù P., Hookey LC., Morales A., Le Moine O., Devière J. The treatment of patients with symptomatic common bile duct stenosis secondary to chronic pancreatitis using partially covered metal stents: a pilot study. Endoscopy. 2005. 37:735–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Biliary Strictures after Liver Transplantation
- Biliary complications after living donor right lobe liver transplantation in adults
- De novo hepatico-gastric stent placement for biliary stricture via percutaneous transhepatic biliary approach
- Magnetic compression anastomosis for treatment of post-transplant biliary stricture: A case report with dual-graft living donor liver transplantation