J Korean Soc Radiol.
2010 May;62(5):477-481. 10.3348/jksr.2010.62.5.477.
Practical Application of a Coronal MR Image during a Uterine Fibroid Embolization (UFE)
- Affiliations
-
- 1Department of Diagnostic Radiology, CHA Bundang Medical Center, CHA University, Korea. mdkim@cha.ac.kr
- 2Department of Obstetrics & Gynecology, CHA Bundang Medical Center, CHA University, Korea.
- KMID: 2002957
- DOI: http://doi.org/10.3348/jksr.2010.62.5.477
Abstract
- PURPOSE
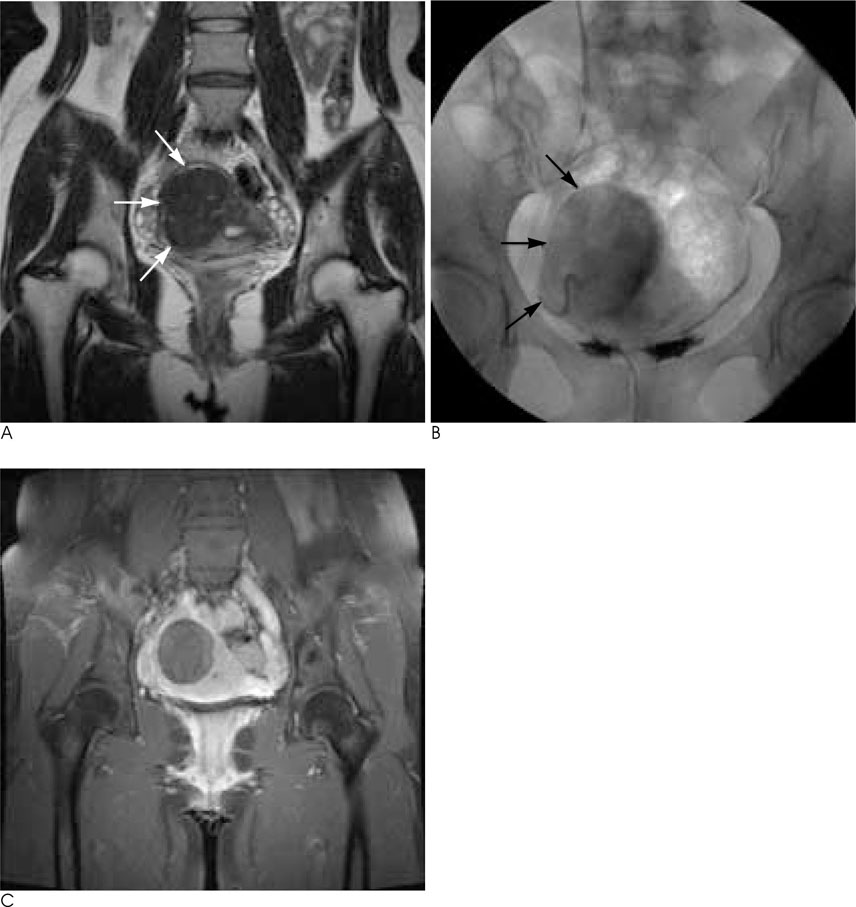
To assess the role of coronal MR images during uterine fibroid embolization (UFE).
MATERIALS AND METHODS
A prospective study of 100 consecutive patients who underwent a uterine fibroid embolization was performed. The average age at embolization was 40.2 years (range, 19-49 years). The size of the predominant fibroids ranged from 2.5 cm to 21.0 cm (mean, 7.5 cm). The embolic agents included non-spherical polyvinyl alcohol particles. The angiographic and spot images after embolization were compared with coronal MR images. The patterns were divided into three categories: Matching, Undetermined, and Mismatching.
RESULTS
Coronal MR images were correlated with angiographic or single shot images of the uterus after embolization in 94 cases, undeterminined in three cases, and mismatched in three cases. Post-embolization aortographies were not helpful in patients showing complete matching images. In three cases of mismatching, two had ovarian collateral supplies to predominant fibroids in the uterine fundus and the remaining patient had an internal pudendal artery of collaterals to fibroid. Mismatching spot images combined with MRI allowed us to find other collateral vascularities.
CONCLUSION
Coronal MR images provided comprehensive information for the appropriate UFE. When perfectly matched, we could make sure that a particular UFE is appropriate without concern for collaterals.
MeSH Terms
Figure
Reference
-
1. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001; 98:29–34.2. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002; 109:1262–1272.3. Goodwin SC, Spies JB, Worthington-Kirsch R, Peterson E, Pron G, Li S, et al. Uterine artery embolization for treatment of leiomyomata: long-term outcomes from the FIBROID Registry. Obstet Gynecol. 2008; 111:22–33.4. Nikolic B, Spies JB, Abbara S, Goodwin SC. Ovarian artery supply of uterine fibroids as a cause of treatment failure after uterine artery embolization: a case report. J Vasc Interv Radiol. 1999; 10:1167–1170.5. Barth MM, Spies JB. Ovarian artery embolization supplementing uterine embolization for leiomyomata. J Vasc Interv Radiol. 2003; 14:1177–1182.6. Andrews RT, Bromley PJ, Pfister ME. Successful embolization of collaterals from the ovarian artery during uterine artery embolization for fibroids: a case report. J Vasc Interv Radiol. 2000; 11:607–610.7. White AM, Banovac F, Spies JB. Patient radiation exposure during uterine fibroid embolization and the dose attributable to aortography. J Vasc Interv Radiol. 2007; 18:573–576.8. White AM, Banovac F, Yousefi S, Slack RS, Spies JB. Uterine fibroid embolization: the utility of aortography in detecting ovarian artery collateral supply. Radiology. 2007; 244:291–298.9. Goodwin SC, McLucas B, Lee M, Chen G, Perrella R, Vedantham S, et al. Uterine artery embolization for the treatment of uterine leiomyomata: mid-term results. J Vasc Interv Radiol. 1999; 10:1159–1165.10. Pelage JP, Le Dref O, Soyer P, Kardache M, Dahan H, Abitbol M, et al. Fibroid-related menorrhagia: treatment with superselective embolization of the uterine arteries and mid-term follow-up. Radiology. 2000; 215:428–431.11. Spies JB, Bruno J, Czeyda-Pommersheim F, Magee ST, Ascher SA, Jha RC. Long-term outcome of uterine artery embolization of leiomyomata. Obstet Gynecol. 2005; 106:933–939.12. Matson M, Nicholson A, Belli AM. Anastomoses of the ovarian and uterine arteries: a potential pitfall and cause of failure of uterine embolization. Cardiovasc Intervent Radiol. 2000; 23:393–396.13. Barth MM, Spies JB. Ovarian artery embolization supplementing uterine embolization for leiomyomata. J Vasc Interv Radiol. 2003; 14:1177–1182.14. Binkert CA, Andrews RT, Kaufman JA. Utility of nonselective abdominal aortography in demonstrating ovarian artery collaterals in patients undergoing uterine artery embolization for fibroids. J Vasc Interv Radiol. 2001; 12:841–845.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Ultrasonographic Findings after a Uterine Fibroid Embolization: The Value of Differentiate from Procedure-Related Uterine Infection
- Hounsfield Number Measurement after a Uterine Fibroid Embolization: Significance as a Predictive Factor of Embolization Success
- Ovarian Protection by Selective Coil Embolization of a Uteroovarian Anastomosis before Uterine Fibroid Embolization: A Report of Two Cases
- A Case of Uterine Fibroids Necrosis after Transarterial Embolization for Treatment of Uterine Fibroids
- A Case of Vaginal Expulsion of Submucosal Fibroid after Uterine Artery Embolization