J Korean Soc Radiol.
2010 May;62(5):427-434. 10.3348/jksr.2010.62.5.427.
The Cardiac MR Images and Causes of Paradoxical Septal Motion
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Korea.
- 2Department of Radiology, Seoul National University Bundang Hospital, Korea. dhk0827@schbc.ac.kr
- 3Department of Radiology, Ulsan University Hospital, Korea.
- 4Department of Radiology, Seoul National University Hospital, Korea.
- KMID: 2002949
- DOI: http://doi.org/10.3348/jksr.2010.62.5.427
Abstract
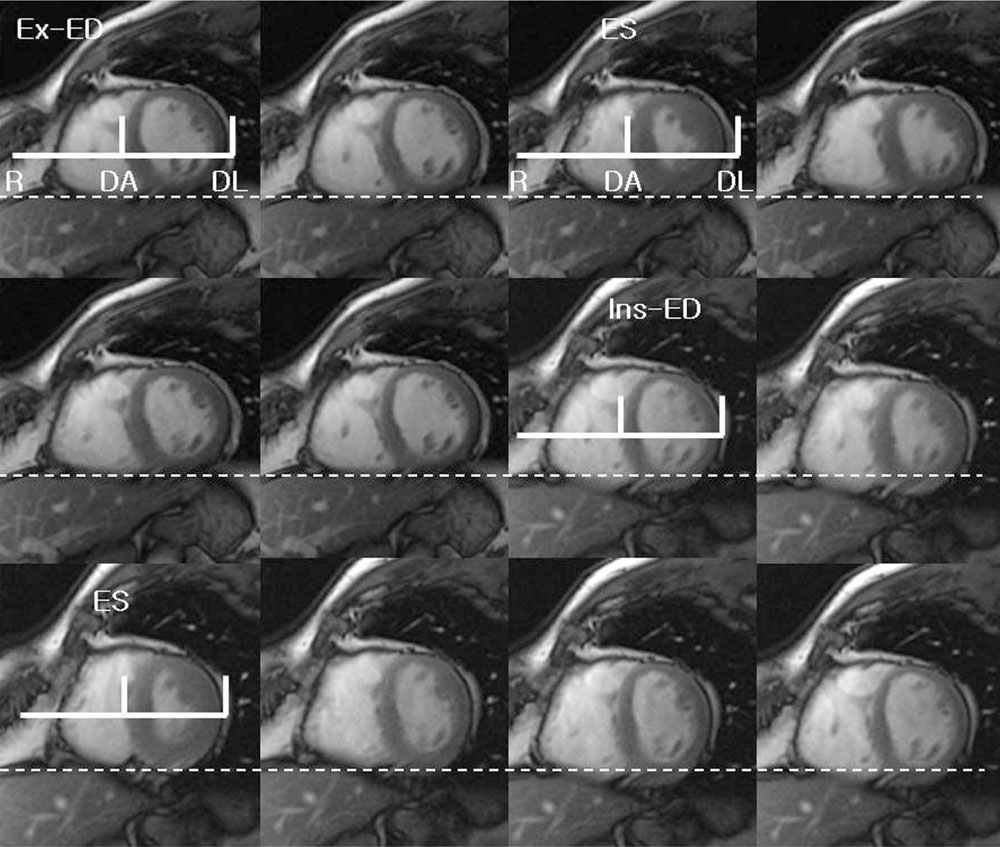
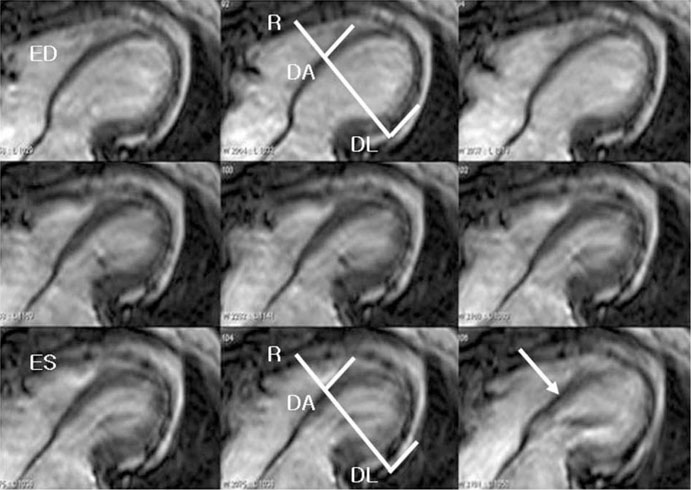
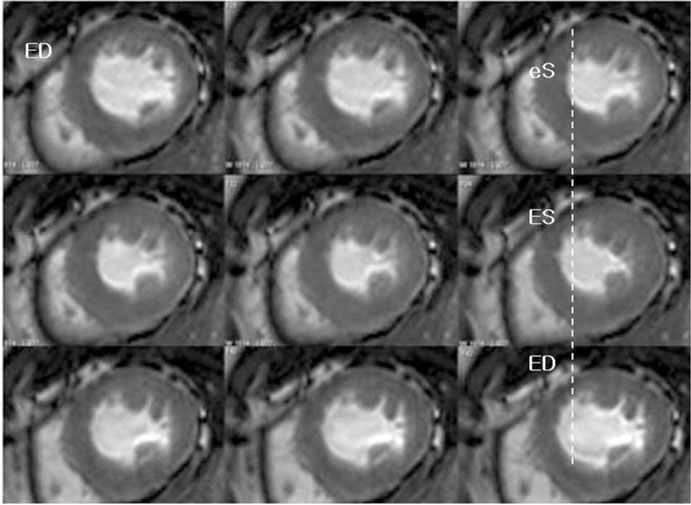
- Real-time cine MRI studies using the steady-state free precession (SSFP) technique are very useful for evaluating cardiac and septal motion. During diastole, the septum acts as a compliant membrane between the two ventricles, and its position and geometry respond to even small alterations in the trans-septal pressure gradients. Abnormal septal motion can be caused by an overload of the right ventricle, delayed ventricular filling and abnormal conduction. In this study, we illustrate, based on our experiences, the causes of abnormal septal motion such as corrective surgery for tetralogy of Fallot, an atrial septal defect, pulmonary thromboembolism, mitral stenosis, constrictive pericarditis and left bundle branch block. In addition, we discuss the significance of paradoxical septal motion in the context of cardiac MR imaging.
MeSH Terms
Figure
Reference
-
1. Lima JA, Guzman PA, Yin FC, Brawley RK, Humphrey L, Traill TA, et al. Septal geometry in the unloaded living human heart. Circulation. 1986; 74:463–468.2. Weyman AE, Wann S, Feigenbaum H, Dillon JC. Mechanism of abnormal septal motion in patients with right ventricular volume overload: a cross-sectional echocardiographic study. Circulation. 1976; 54:179–186.3. Giorgi B, Mollet NR, Dymarkowski S, Rademaakers FE, Bogaert J. Clinically suspected constrictive pericarditis: MR imaging assessment of ventricular septal motion and configuration in patients and healthy subjects. Radiology. 2003; 228:417–424.4. Francone M, Dymarkowski S, Kalantzi M, Bogaert J. Real-time cine MRI of ventricular septal motion: a novel approach to assess ventricular coupling. J Magn Reson Imaging. 2005; 21:305–309.5. Joshi SB, Salah AK, Mendoza DD, Goldstein SA, Fuisz AR, Lindsay J. Mechanism of paradoxical ventricular septal motion after coronary artery bypass grafting. Am J Cardiol. 2009; 103:212–215.6. Dong SJ, Crawley AP, MacGregor JH, Petrank YF, Bergman DW, Belenkie I, et al. Regional left ventricular systolic function in relation to the cavity geometry in patients with chronic right ventricular pressure overload: a three-dimensional tagged magnetic resonance imaging study. Circulation. 1995; 91:2359–2370.7. King ME, Braun H, Goldblatt A, Liberthson R, Weyman AE. Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation. 1983; 68:68–75.8. Vliegen HW, van Straten A, de Roos A, Roest AA, Schoof PH, Zwinderman AH, et al. Magnetic resonance imaging to assess the hemodynamic effects of pulmonary valve replacement in adults late after repair of tetralogy of Fallot. Circulation. 2002; 106:1703–1707.9. Abd El Rahman MY, Hui W, Dsebissowa F, Schubert S, Gutberlet M, Hetzer R, et al. Quantitative analysis of paradoxical interventricular septal motion following corrective surgery of tetralogy of fallot. Pediatr Cardiol. 2005; 26:379–384.10. Popio KA, Gorlin R, Teichholz LE, Cohn PF, Bechtel D, Herman MV. Abnormalities of left ventricular function and geometry in adults with an atrial septal defect. Ventriculographic, hemodynamic and echocardiographic studies. Am J Cardiol. 1975; 36:302–330.11. Marcus JT, Vonk Noordegraaf A, Roeleveld RJ, Postmus PE, Heethaar RM, Van Rossum AC, et al. Impaired left ventricular filling due to right ventricular pressure overload in primary pulmonary hypertension: noninvasive monitoring using MRI. Chest. 2001; 119:1761–1765.12. Roeleveld RJ, Marcus JT, Faes TJ, Gan TJ, Boonstra A, Postmus PE, et al. Interventricular septal configuration at MR imaging and pulmonary arterial pressure in pulmonary hypertension. Radiology. 2005; 234:710–717.13. Thompson CR, Kingma I, MacDonald RP, Belenkie I, Tyberg JV, Smith ER. Transseptal pressure gradient and diastolic ventricular septal motion in patients with mitral stenosis. Circulation. 1987; 76:974–980.14. Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol. 1985; 5:918–927.15. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block. Circulation. 1989; 79:845–853.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative and Postoperative Echocardiographic Findings in Atrial Septal Defect
- Changes of Echocardiographic Findings after Surgical Correction of Atrial Septal Defect in Adult
- Outcomes and dynamic changes of the mitral valve after surgical repair of mitral regurgitation in patients with an atrial septal defect
- Cardiac Magnetic Resonance Imaging Using Multi-physiological Intelligent Trigger System
- Tentatively Diagnosed as Myxoma : Transit Thrombus Entrapped in Patent Foramen Ovale