Korean J Urol.
2012 Jan;53(1):1-8. 10.4111/kju.2012.53.1.1.
Disorders of Sex Development
- Affiliations
-
- 1Department of Urology, University of Ulsan College of Medicine, Seoul, Korea. kskim2@amc.seoul.kr
- KMID: 1988815
- DOI: http://doi.org/10.4111/kju.2012.53.1.1
Abstract
- The birth of a new baby is one of the most dramatic events in a family, and the first question is usually "is it a boy or a girl?" The newborn infant with ambiguous external genitalia often comes as a surprise for the doctors as well as the parents and is sometimes described as an endocrine emergency situation presenting a problem of sex assignment. The nomenclature such as 'intersex', 'hermaphrodite', and 'pseudohermaphrodite' is out of date as well as confusing, and many urologists are concerned that these confusing terms could be perceived to be pejorative by some affected families. In response to concerns regarding outdated and controversial terms, the Chicago Consensus held in 2005 recommended new terminology based on the umbrella term disorders of sex differentiation (DSDs). The term DSD has a comprehensive definition including any problem noted at birth in which the genitalia are atypical in relation to the chromosomes or gonads. The karyotype is used as a prefix defining the classification of DSD. DSDs are rare and complex. The optimal management of patients with DSD must be individualized and multidisciplinary, considering all aspects, including psychological care and full disclosure of alternatives relating to surgery type and timing. Although further studies are necessary to confirm guidelines and recommendations fitting for the individual patients with DSD, this article is an attempt to provide a balanced perspective for new taxonomy, clinical evaluation, and medical, surgical, and psychological management of DSD.
Keyword
MeSH Terms
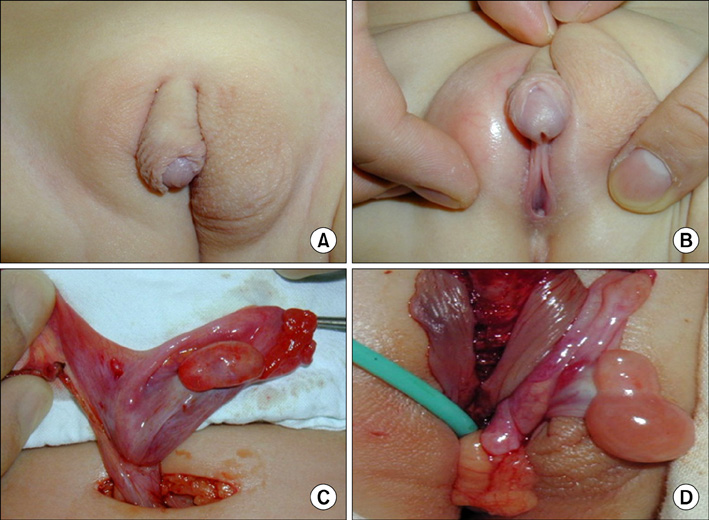
Figure
Reference
-
1. Conn J, Gillam L, Conway GS. Revealing the diagnosis of androgen insensitivity syndrome in adulthood. BMJ. 2005. 331:628–630.2. Hughes IA, Houk C, Ahmed SF, Lee PA. LWPES Consensus Group. ESPE Consensus Group. Consensus statement on management of intersex disorders. Arch Dis Child. 2006. 91:554–563.3. Houk CP, Hughes IA, Ahmed SF, Lee PA. Writing Committee for the International Intersex Consensus Conference Participants. Summary of consensus statement on intersex disorders and their management. International Intersex Consensus Conference. Pediatrics. 2006. 118:753–757.4. Lee PA, Houk CP, Ahmed SF, Hughes IA. International Consensus Conference on Intersex organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex. Pediatrics. 2006. 118:e488–e500.5. Blackless M, Charuvastra A, Derryck A, Fausto-Sterling A, Lauzanne K, Lee E. How sexually dimorphic are we? Review and synthesis. Am J Hum Biol. 2000. 12:151–166.6. Sax L. How common is intersex? A response to Anne Fausto-Sterling. J Sex Res. 2002. 39:174–178.7. Thyen U, Lanz K, Holterhus PM, Hiort O. Epidemiology and initial management of ambiguous genitalia at birth in Germany. Horm Res. 2006. 66:195–203.8. Pang SY, Wallace MA, Hofman L, Thuline HC, Dorche C, Lyon IC, et al. Worldwide experience in newborn screening for classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Pediatrics. 1988. 81:866–874.9. Skakkebaek NE. Testicular dysgenesis syndrome. Horm Res. 2003. 60:Suppl 3. 49.10. Lee PA. A perspective on the approach to the intersex child born with genital ambiguity. J Pediatr Endocrinol Metab. 2004. 17:133–140.11. Frader J, Alderson P, Asch A, Aspinall C, Davis D, Dreger A, et al. Health care professionals and intersex conditions. Arch Pediatr Adolesc Med. 2004. 158:426–428.12. Clayton PE, Miller WL, Oberfield SE, Ritzén EM, Sippell WG, Speiser PW. Consensus statement on 21-hydroxylase deficiency from the European Society for Paediatric Endocrinology and the Lawson Wilkins Pediatric Endocrine Society. Horm Res. 2002. 58:188–195.13. American Academy of Pediatrics Council on Children with Disabilities. Care coordination in the medical home: integrating health and related systems of care for children with special health care needs. Pediatrics. 2005. 116:1238–1244.14. Nihoul-Fékété C. The Isabel Forshall Lecture. Surgical management of the intersex patient: an overview in 2003. J Pediatr Surg. 2004. 39:144–145.15. Dreger AD, Chase C, Sousa A, Gruppuso PA, Frader J. Changing the nomenclature/taxonomy for intersex: a scientific and clinical rationale. J Pediatr Endocrinol Metab. 2005. 18:729–733.16. Cohen-Bendahan CC, van de Beek C, Berenbaum SA. Prenatal sex hormone effects on child and adult sex-typed behavior: methods and findings. Neurosci Biobehav Rev. 2005. 29:353–384.17. Meyer-Bahlburg HF. Gender and sexuality in classic congenital adrenal hyperplasia. Endocrinol Metab Clin North Am. 2001. 30:155–171.18. Goy RW, Bercovitch FB, McBrair MC. Behavioral masculinization is independent of genital masculinization in prenatally androgenized female rhesus macaques. Horm Behav. 1988. 22:552–571.19. Wallen K. Hormonal influences on sexually differentiated behavior in nonhuman primates. Front Neuroendocrinol. 2005. 26:7–26.20. Moore CL. The role of maternal stimulation in the development of sexual behavior and its neural basis. Ann N Y Acad Sci. 1992. 662:160–177.21. Wallen K. Nature needs nurture: the interaction of hormonal and social influences on the development of behavioral sex differences in rhesus monkeys. Horm Behav. 1996. 30:364–378.22. Donahoe PK, Powell DM, Lee MM. Clinical management of intersex abnormalities. Curr Probl Surg. 1991. 28:513–579.23. Creighton S, Alderson J, Brown S, Minto CL. Medical photography: ethics, consent and the intersex patient. BJU Int. 2002. 89:67–71.24. Honour JW, Torresani T. Evaluation of neonatal screening for congenital adrenal hyperplasia. Horm Res. 2001. 55:206–211.25. MacLaughlin DT, Donahoe PK. Sex determination and differentiation. N Engl J Med. 2004. 350:367–378.26. Ahmed SF, Cheng A, Dovey L, Hawkins JR, Martin H, Rowland J, et al. Phenotypic features, androgen receptor binding, and mutational analysis in 278 clinical cases reported as androgen insensitivity syndrome. J Clin Endocrinol Metab. 2000. 85:658–665.27. Morel Y, Rey R, Teinturier C, Nicolino M, Michel-Calemard L, Mowszowicz I, et al. Aetiological diagnosis of male sex ambiguity: a collaborative study. Eur J Pediatr. 2002. 161:49–59.28. Quillin JM, Jackson-Cook C, Bodurtha J. The link between providers and patients: how laboratories can ensure quality results with genetic testing. Clin Leadersh Manag Rev. 2003. 17:351–357.29. Park JG, Cha YB, Kim CI, Kim KS. Impalpable testis: localization and management. Korean J Urol. 1990. 31:665–670.30. Kim KR, Kwon Y, Joung JY, Kim KS, Ayala AG, Ro JY. True hermaphroditism and mixed gonadal dysgenesis in young children: a clinicopathologic study of 10 cases. Mod Pathol. 2002. 15:1013–1019.31. Joung JY, Yoo HW, Kim KR, Kim KS. Critical histopathologic findings for differential diagnosis between true hermaphroditism and mixed gonadal dysgenesis. Korean J Urol. 2002. 43:877–886.32. Byne W. Developmental endocrine influences on gender identity: implications for management of disorders of sex development. Mt Sinai J Med. 2006. 73:950–959.33. Dessens AB, Slijper FM, Drop SL. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch Sex Behav. 2005. 34:389–397.34. Diamond DA, Burns JP, Mitchell C, Lamb K, Kartashov AI, Retik AB. Sex assignment for newborns with ambiguous genitalia and exposure to fetal testosterone: attitudes and practices of pediatric urologists. J Pediatr. 2006. 148:445–449.35. Mazur T. Gender dysphoria and gender change in androgen insensitivity or micropenis. Arch Sex Behav. 2005. 34:411–421.36. Cohen-Kettenis PT. Gender change in 46,XY persons with 5alpha-reductase-2 deficiency and 17beta-hydroxysteroid dehydrogenase-3 deficiency. Arch Sex Behav. 2005. 34:399–410.37. Migeon CJ, Wisniewski AB, Gearhart JP, Meyer-Bahlburg HF, Rock JA, Brown TR, et al. Ambiguous genitalia with perineoscrotal hypospadias in 46,XY individuals: long-term medical, surgical, and psychosexual outcome. Pediatrics. 2002. 110:e31.38. Mendonca BB, Inacio M, Costa EM, Arnhold IJ, Russell DW, Wilson JD. Male pseudohermaphroditism due to 5 alpha-reductase 2 deficiency: outcome of a Brazilian cohort. Endocrinologist. 2003. 13:201–204.39. Crouch NS, Minto CL, Laio LM, Woodhouse CR, Creighton SM. Genital sensation after feminizing genitoplasty for congenital adrenal hyperplasia: a pilot study. BJU Int. 2004. 93:135–138.40. Rink RC, Adams MC. Feminizing genitoplasty: state of the art. World J Urol. 1998. 16:212–218.41. Farkas A, Chertin B, Hadas-Halpren I. 1-Stage feminizing genitoplasty: 8 years of experience with 49 cases. J Urol. 2001. 165:2341–2346.42. Baskin LS. Anatomical studies of the female genitalia: surgical reconstructive implications. J Pediatr Endocrinol Metab. 2004. 17:581–587.43. American Academy of Pediatrics. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996. 97:590–594.44. Warne G, Grover S, Hutson J, Sinclair A, Metcalfe S, Northam F, et al. A long-term outcome study of intersex conditions. J Pediatr Endocrinol Metab. 2005. 18:555–567.45. Lee PA, Witchel SF. Genital surgery among females with congenital adrenal hyperplasia: changes over the past five decades. J Pediatr Endocrinol Metab. 2002. 15:1473–1477.46. Kogan SJ, Smey P, Levitt SB. Subtunical total reduction clitoroplasty: a safe modification of existing techniques. J Urol. 1983. 130:746–748.47. Gearhart JP, Burnett A, Owen JH. Measurement of pudendal evoked potentials during feminizing genitoplasty: technique and applications. J Urol. 1995. 153:486–487.48. Schnitzer JJ, Donahoe PK. Surgical treatment of congenital adrenal hyperplasia. Endocrinol Metab Clin North Am. 2001. 30:137–154.49. Gonzalez R, Fernandes ET. Single-stage feminization genitoplasty. J Urol. 1990. 143:776–778.50. Snyder HM 3rd, Retik AB, Bauer SB, Colodny AH. Feminizing genitoplasty: a synthesis. J Urol. 1983. 129:1024–1026.51. Frimberger D, Gearhart JP. Ambiguous genitalia and intersex. Urol Int. 2005. 75:291–297.52. Kwon JB, Yoo ES, Chung SK. Surgical correction of intersex with feminizing genitoplasty. Korean J Urol. 2004. 45:1028–1034.53. Oesterling JE, Gearhart JP, Jeffs RD. A unified approach to early reconstructive surgery of the child with ambiguous genitalia. J Urol. 1987. 138:1079–1082.54. Mouriquand PD, Mure PY. Current concepts in hypospadiology. BJU Int. 2004. 93:Suppl 3. 26–34.55. Rangecroft L. British Association of Paediatric Surgeons Working Party on the Surgical Management of Children Born With Ambiguous Genitalia. Surgical management of ambiguous genitalia. Arch Dis Child. 2003. 88:799–801.56. Rørth M, Rajpert-De Meyts E, Andersson L, Dieckmann KP, Fosså SD, Grigor KM, et al. Carcinoma in situ in the testis. Scand J Urol Nephrol Suppl. 2000. 205:166–186.57. Ramani P, Yeung CK, Habeebu SS. Testicular intratubular germ cell neoplasia in children and adolescents with intersex. Am J Surg Pathol. 1993. 17:1124–1133.58. Warne GL, Grover S, Zajac JD. Hormonal therapies for individuals with intersex conditions: protocol for use. Treat Endocrinol. 2005. 4:19–29.59. Drobac S, Rubin K, Rogol AD, Rosenfield RL. A workshop on pubertal hormone replacement options in the United States. J Pediatr Endocrinol Metab. 2006. 19:55–64.60. Rogol AD. New facets of androgen replacement therapy during childhood and adolescence. Expert Opin Pharmacother. 2005. 6:1319–1336.61. Ahmed SF, Tucker P, Mayo A, Wallace AM, Hughes IA. Randomized, crossover comparison study of the short-term effect of oral testosterone undecanoate and intramuscular testosterone depot on linear growth and serum bone alkaline phosphatase. J Pediatr Endocrinol Metab. 2004. 17:941–950.62. Mayo A, Macintyre H, Wallace AM, Ahmed SF. Transdermal testosterone application: pharmacokinetics and effects on pubertal status, short-term growth, and bone turnover. J Clin Endocrinol Metab. 2004. 89:681–687.