Korean J Urol.
2014 Jan;55(1):23-28. 10.4111/kju.2014.55.1.23.
Interfraction Prostate Movement in Bone Alignment After Rectal Enema for Radiotherapy
- Affiliations
-
- 1Department of Urology, Dong-A University College of Medicine, Busan, Korea.
- 2Department of Radiation Oncology, Dong-A University College of Medicine, Busan, Korea. cymin00@dau.ac.kr
- KMID: 1988448
- DOI: http://doi.org/10.4111/kju.2014.55.1.23
Abstract
- PURPOSE
To assess the effect of a rectal enema on interfraction prostate movement in bone alignment (BA) for prostate radiotherapy (RT), we analyzed the spatial difference in prostates in a bone-matched setup.
MATERIALS AND METHODS
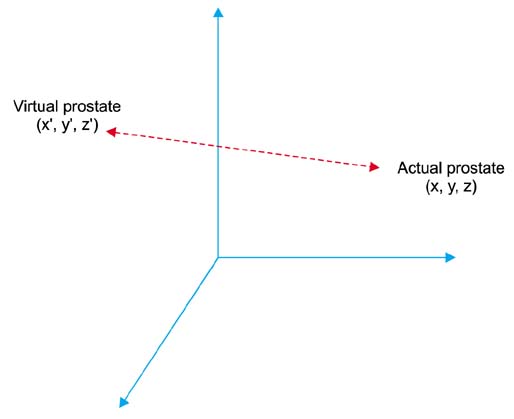
We performed BA retrospectively with data from prostate cancer patients who underwent image-guided RT (IGRT). The prostate was identified with implanted fiducial markers. The setup for the IGRT was conducted with the matching of three fiducial markers on RT planning computed tomography images and those on two oblique kV x-ray images. Offline BA was performed at the same position. The coordinates of a virtual prostate in BA and a real prostate were obtained by use of the ExaxTrac/NovalisBody system, and the distance between them was calculated as the spatial difference. Interfraction prostate displacement was drawn from the comparison of the spatial differences.
RESULTS
A total of 15 patients with localized prostate cancer treated with curative hypofractionated IGRT were enrolled. A total of 420 fractions were analyzed. The mean of the interfraction prostate displacements after BA was 3.12+/-2.00 mm (range, 0.20-10.53 mm). The directional difference was profound in the anterior-posterior and supero-inferior directions (2.14+/-1.73 mm and 1.97+/-1.44 mm, respectively) compared with the right-left direction (0.26+/-0.22 mm, p<0.05). The required margin around the clinical target volume was 4.97 mm with the formula of van Herk et al.
CONCLUSIONS
The interfraction prostate displacement was less frequent when a rectal enema was performed before the procedure. A rectal enema can be used to reduce interfraction prostate displacement and resulting clinical target volume-to-planning target volume margin.
MeSH Terms
Figure
Reference
-
1. Antolak JA, Rosen II, Childress CH, Zagars GK, Pollack A. Prostate target volume variations during a course of radiotherapy. Int J Radiat Oncol Biol Phys. 1998; 42:661–672.2. Melian E, Mageras GS, Fuks Z, Leibel SA, Niehaus A, Lorant H, et al. Variation in prostate position quantitation and implications for three-dimensional conformal treatment planning. Int J Radiat Oncol Biol Phys. 1997; 38:73–81.3. McNeal JE, Redwine EA, Freiha FS, Stamey TA. Zonal distribution of prostatic adenocarcinoma. Correlation with histologic pattern and direction of spread. Am J Surg Pathol. 1988; 12:897–906.4. de Crevoisier R, Tucker SL, Dong L, Mohan R, Cheung R, Cox JD, et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys. 2005; 62:965–973.5. Heemsbergen WD, Hoogeman MS, Witte MG, Peeters ST, Incrocci L, Lebesque JV. Increased risk of biochemical and clinical failure for prostate patients with a large rectum at radiotherapy planning: results from the Dutch trial of 68 GY versus 78 Gy. Int J Radiat Oncol Biol Phys. 2007; 67:1418–1424.6. Ogino I, Uemura H, Inoue T, Kubota Y, Nomura K, Okamoto N. Reduction of prostate motion by removal of gas in rectum during radiotherapy. Int J Radiat Oncol Biol Phys. 2008; 72:456–466.7. Fiorino C, Di Muzio N, Broggi S, Cozzarini C, Maggiulli E, Alongi F, et al. Evidence of limited motion of the prostate by carefully emptying the rectum as assessed by daily MVCT image guidance with helical tomotherapy. Int J Radiat Oncol Biol Phys. 2008; 71:611–617.8. Ghilezan MJ, Jaffray DA, Siewerdsen JH, Van Herk M, Shetty A, Sharpe MB, et al. Prostate gland motion assessed with cine-magnetic resonance imaging (cine-MRI). Int J Radiat Oncol Biol Phys. 2005; 62:406–417.9. Langen KM, Zhang Y, Andrews RD, Hurley ME, Meeks SL, Poole DO, et al. Initial experience with megavoltage (MV) CT guidance for daily prostate alignments. Int J Radiat Oncol Biol Phys. 2005; 62:1517–1524.10. Moseley DJ, White EA, Wiltshire KL, Rosewall T, Sharpe MB, Siewerdsen JH, et al. Comparison of localization performance with implanted fiducial markers and cone-beam computed tomography for on-line image-guided radiotherapy of the prostate. Int J Radiat Oncol Biol Phys. 2007; 67:942–953.11. Beard CJ, Kijewski P, Bussiere M, Gelman R, Gladstone D, Shaffer K, et al. Analysis of prostate and seminal vesicle motion: implications for treatment planning. Int J Radiat Oncol Biol Phys. 1996; 34:451–458.12. Roeske JC, Forman JD, Mesina CF, He T, Pelizzari CA, Fontenla E, et al. Evaluation of changes in the size and location of the prostate, seminal vesicles, bladder, and rectum during a course of external beam radiation therapy. Int J Radiat Oncol Biol Phys. 1995; 33:1321–1329.13. van Herk M, Bruce A, Kroes AP, Shouman T, Touw A, Lebesque JV. Quantification of organ motion during conformal radiotherapy of the prostate by three dimensional image registration. Int J Radiat Oncol Biol Phys. 1995; 33:1311–1320.14. van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys. 2000; 47:1121–1135.15. Ten Haken RK, Forman JD, Heimburger DK, Gerhardsson A, McShan DL, Perez-Tamayo C, et al. Treatment planning issues related to prostate movement in response to differential filling of the rectum and bladder. Int J Radiat Oncol Biol Phys. 1991; 20:1317–1324.16. Schild SE, Casale HE, Bellefontaine LP. Movements of the prostate due to rectal and bladder distension: implications for radiotherapy. Med Dosim. 1993; 18:13–15.17. Frank SJ, Dong L, Kudchadker RJ, De Crevoisier R, Lee AK, Cheung R, et al. Quantification of prostate and seminal vesicle interfraction variation during IMRT. Int J Radiat Oncol Biol Phys. 2008; 71:813–820.18. Zelefsky MJ, Crean D, Mageras GS, Lyass O, Happersett L, Ling CC, et al. Quantification and predictors of prostate position variability in 50 patients evaluated with multiple CT scans during conformal radiotherapy. Radiother Oncol. 1999; 50:225–234.19. Peng C, Ahunbay E, Chen G, Anderson S, Lawton C, Li XA. Characterizing interfraction variations and their dosimetric effects in prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 79:909–914.20. Tanyi JA, He T, Summers PA, Mburu RG, Kato CM, Rhodes SM, et al. Assessment of planning target volume margins for intensity-modulated radiotherapy of the prostate gland: role of daily inter- and intrafraction motion. Int J Radiat Oncol Biol Phys. 2010; 78:1579–1585.21. Beltran C, Herman MG, Davis BJ. Planning target margin calculations for prostate radiotherapy based on intrafraction and interfraction motion using four localization methods. Int J Radiat Oncol Biol Phys. 2008; 70:289–295.22. Kudchadker RJ, Lee AK, Yu ZH, Johnson JL, Zhang L, Zhang Y, et al. Effectiveness of using fewer implanted fiducial markers for prostate target alignment. Int J Radiat Oncol Biol Phys. 2009; 74:1283–1289.23. Merrick GS, Butler WM, Dorsey AT, Dorsey JT 3rd. The effect of constipation on rectal dosimetry following prostate brachytherapy. Med Dosim. 2000; 25:237–241.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intractable rectal stricture caused by hot water enema
- Interfraction variation and dosimetric changes during image-guided radiation therapy in prostate cancer patients
- Positional Reproducibility and Effects of a Rectal Balloon in Prostate Cancer Radiotherapy
- Preventive efficacy of hydrocortisone enema for radiation proctitis in rectal cancer patients undergoing short-course radiotherapy: a phase II randomized placebo-controlled clinical trial
- Should a Contrast Enema Be Performed Before Reversal of a Diverting Stoma in Lower Rectal Surgery?