Korean J Urol.
2014 Mar;55(3):213-218. 10.4111/kju.2014.55.3.213.
Prevalence of Daytime Urinary Incontinence and Related Risk Factors in Primary School Children in Turkey
- Affiliations
-
- 1Department of Urology, Kayseri Training and Research Hospital, Kayseri, Turkey. drbolat@hotmail.com
- 2Department of Urology, Acibadem University, Faculty of Medicine, Istanbul, Turkey.
- 3Department of Urology, Pamukkale University, Faculty of Medicine, Denizli, Turkey.
- 4Department of Urology, Canakkale Onsekiz Mart University, Faculty of Medicine, Canakkale, Turkey.
- 5Department of Public Health, Pamukkale University, Faculty of Medicine, Denizli, Turkey.
- KMID: 1988427
- DOI: http://doi.org/10.4111/kju.2014.55.3.213
Abstract
- PURPOSE
Urinary incontinence is one of the major urinary symptoms in children and adolescents and can lead to major distress for the affected children and their parents. In accordance with the definitions of the Standardization Committee of the International Children's Continence Society, daytime urinary incontinence (DUI) is uncontrollable leakage of urine during the day. The aim of this cross-sectional study was to investigate the prevalence and associated risk factors of DUI in Turkish primary school children.
MATERIALS AND METHODS
The questionnaire, which covered sociodemographic variables and the voiding habits of the children, was completed by the parents of 2,353 children who were attending primary school in Denizli, a developing city of Turkey. The children's voiding habits were evaluated by use of the Dysfunctional Voiding and Incontinence Symptoms Score, which is a validated questionnaire. Children with a history of neurological or urological diseases were excluded.
RESULTS
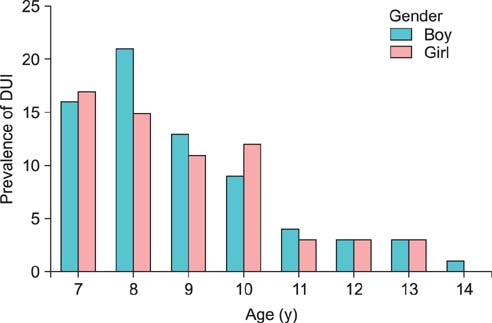
The participation rate was 91.9% (2,164 people). The overall prevalence of DUI was 8.0%. The incidence of DUI tended to decrease with increasing age and was not significantly different between genders (boys, 8.8%; girls, 7.3%; p=0.062). Age, maternal education level, family history of daytime wetting, settlement (urban/rural), history of constipation, urinary tract infection, and urgency were independent risk factors of DUI.
CONCLUSIONS
Our findings showed that DUI is a common health problem in primary school children. In an effort to increase awareness of children's voiding problems and the risk factors for urinary dysfunction in the population, educational programs and larger school-based screening should be carried out, especially in regions with low socioeconomic status.
Keyword
MeSH Terms
Figure
Reference
-
1. Hellstrom AL, Hanson E, Hansson S, Hjalmas K, Jodal U. Micturition habits and incontinence in 7-year-old Swedish school entrants. Eur J Pediatr. 1990; 149:434–437.2. Neveus T, von Gontard A, Hoebeke P, Hjalmas K, Bauer S, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society. J Urol. 2006; 176:314–324.3. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: American Psychiatry Press;1995.4. Bakker E, van Sprundel M, van der Auwera JC, van Gool JD, Wyndaele JJ. Voiding habits and wetting in a population of 4,332 Belgian schoolchildren aged between 10 and 14 years. Scand J Urol Nephrol. 2002; 36:354–362.5. Soderstrom U, Hoelcke M, Alenius L, Soderling AC, Hjern A. Urinary and faecal incontinence: a population-based study. Acta Paediatr. 2004; 93:386–389.6. Sureshkumar P, Jones M, Cumming R, Craig J. A population based study of 2,856 school-age children with urinary incontinence. J Urol. 2009; 181:808–815.7. Sureshkumar P, Craig JC, Roy LP, Knight JF. Daytime urinary incontinence in primary school children: a population-based survey. J Pediatr. 2000; 137:814–818.8. Akbal C, Genc Y, Burgu B, Ozden E, Tekgul S. Dysfunctional voiding and incontinence scoring system: quantitative evaluation of incontinence symptoms in pediatric population. J Urol. 2005; 173:969–973.9. Achenbach TM, Edelbrock CS. Manual for the child behaviour check-list and revised child behaviour profile. Burlington: University of Vermont;1983.10. Bower WF, Moore KH, Shepherd RB, Adams RD. The epidemiology of childhood enuresis in Australia. Br J Urol. 1996; 78:602–606.11. Rushton HG. Wetting and functional voiding disorders. Urol Clin North Am. 1995; 22:75–93.12. Kajiwara M, Inoue K, Usui A, Kurihara M, Usui T. The micturition habits and prevalence of daytime urinary incontinence in Japanese primary school children. J Urol. 2004; 171:403–407.13. Lee SD, Sohn DW, Lee JZ, Park NC, Chung MK. An epidemiological study of enuresis in Korean children. BJU Int. 2000; 85:869–873.14. Toktamis A, Demirel Y, Ozkan KU, Garipardic M, Gozukucuk A, Nur N. Prevalence and associated factors of day wetting and combined day and night wetting. Urol Int. 2008; 81:54–59.15. Serel TA, Akhan G, Koyuncuoglu HR, Ozturk A, Dogruer K, Unal S, et al. Epidemiology of enuresis in Turkish children. Scand J Urol Nephrol. 1997; 31:537–539.16. Oge O, Kocak I, Gemalmaz H. Enuresis: point prevalence and associated factors among Turkish children. Turk J Pediatr. 2001; 43:38–43.17. Ozkan KU, Garipardic M, Toktamis A, Karabiber H, Sahinkanat T. Enuresis prevalence and accompanying factors in schoolchildren: a questionnaire study from southeast Anatolia. Urol Int. 2004; 73:149–155.18. Uğuralp S, Karaoglu L, Karaman A, Demircan M, Yakinci C. Frequency of enuresis, constipation and enuresis association with constipation in a group of school children aged 5-9 years in Malatya, Turkey. Turk J Med Sci. 2003; 33:315–320.19. Swithinbank LV, Brookes ST, Shepherd AM, Abrams P. The natural history of urinary symptoms during adolescence. Br J Urol. 1998; 81:Suppl 3. 90–93.20. Hoebeke P, Van Laecke E, Van Camp C, Raes A, Van De Walle J. One thousand video-urodynamic studies in children with non-neurogenic bladder sphincter dysfunction. BJU Int. 2001; 87:575–580.21. Chung JM, Lee SD, Kang DI, Kwon DD, Kim KS, Kim SY, et al. Prevalence and associated factors of overactive bladder in Korean children 5-13 years old: a nationwide multicenter study. Urology. 2009; 73:63–67.22. Esperanca M, Gerrard JW. Nocturnal enuresis: studies in bladder function in normal children and enuretics. Can Med Assoc J. 1969; 101:324–327.23. Hansen A, Hansen B, Dahm TL. Urinary tract infection, day wetting and other voiding symptoms in seven- to eight-year-old Danish children. Acta Paediatr. 1997; 86:1345–1349.24. Swithinbank LV, Heron J, von Gontard A, Abrams P. The natural history of daytime urinary incontinence in children: a large British cohort. Acta Paediatr. 2010; 99:1031–1036.25. Koff SA, Wagner TT, Jayanthi VR. The relationship among dysfunctional elimination syndromes, primary vesicoureteral reflux and urinary tract infections in children. J Urol. 1998; 160(3 Pt 2):1019–1022.26. Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007; 92:486–489.27. Gur E, Turhan P, Can G, Akkus S, Sever L, Guzeloz S, et al. Enuresis: prevalence, risk factors and urinary pathology among school children in Istanbul, Turkey. Pediatr Int. 2004; 46:58–63.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and therapy for functional urinary incontinence in childhood
- The role of primary care of voiding dysfunction in rehabilitation and convalescent hospitals
- A Study on Discomfort of Daily Life and Self-Esteem of Urinary Incontinence in Middle-Aged Women
- The Epidemiology of Childhood Enuresis in Seoul and Kyunggi Province
- Factors Affecting the Severity of Urinary Incontinence and the Quality of Life of Women with Urinary Incontinence