Korean J Urol.
2014 May;55(5):341-348. 10.4111/kju.2014.55.5.341.
Chronic Lower Urinary Tract Symptoms in Young Men Without Symptoms of Chronic Prostatitis: Urodynamic Analyses in 308 Men Aged 50 Years or Younger
- Affiliations
-
- 1Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea. urojsj@yahoo.co.kr
- 2Department of Urology, Kangwon National University Hospital, Chuncheon, Korea.
- KMID: 1988412
- DOI: http://doi.org/10.4111/kju.2014.55.5.341
Abstract
- PURPOSE
We investigated the etiologies of lower urinary tract symptoms (LUTS) and compared urodynamic characteristics between different diagnostic groups in young men with chronic LUTS.
MATERIALS AND METHODS
We reviewed the medical records of 308 men aged 18 to 50 years who had undergone a urodynamic study for chronic LUTS (> or =6 months) without symptoms suggestive of chronic prostatitis.
RESULTS
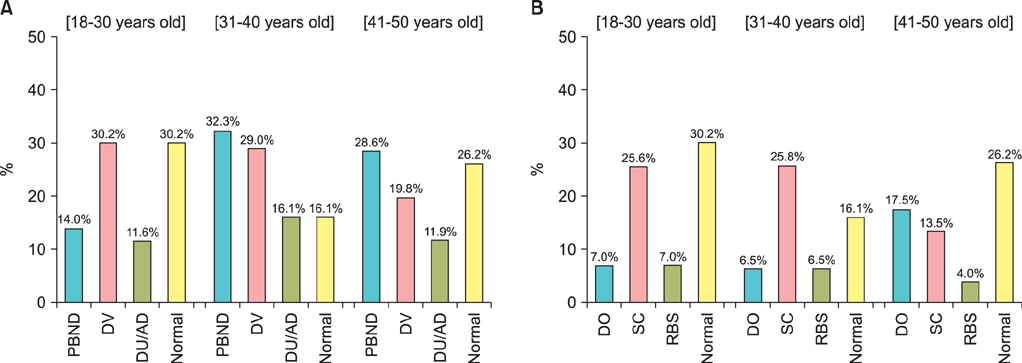
The men's mean age was 40.4 (+/-10.1) years and their mean duration of symptoms was 38.8 (+/-49.2) months. Urodynamic evaluation demonstrated voiding phase dysfunction in 62.1% of cases (primary bladder neck dysfunction [PBND] in 26.0%, dysfunctional voiding [DV] in 23.4%, and detrusor underactivity [DU]/acontractile detrusor [AD] in 12.7%) and a single storage phase dysfunction in 36.4% of cases (detrusor overactivity [DO] in 13.3%, small cystometric capacity in 17.9%, and reduced bladder sensation in 5.2%). Most of the demographic characteristics and clinical symptoms did not differ between these diagnostic groups. Whereas 53.9% of patients with voiding dysfunction had concomitant storage dysfunction, 69.6% of those with storage dysfunction had concomitant voiding dysfunction. Men with DV or DU/AD exhibited lower maximum cystometric capacity than did those with normal urodynamics. Low bladder compliance was most frequent among patients with PBND (10.0%, p=0.025). In storage dysfunctions, men with DO exhibited higher detrusor pressure during voiding than did those with other storage dysfunctions (p<0.01).
CONCLUSIONS
Because clinical symptoms are not useful for predicting the specific urodynamic etiology of LUTS in this population, urodynamic investigation can help to make an accurate diagnosis and, potentially, to guide appropriate treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Irwin DE, Milsom I, Kopp Z, Abrams P, Artibani W, Herschorn S. Prevalence, severity, and symptom bother of lower urinary tract symptoms among men in the EPIC study: impact of overactive bladder. Eur Urol. 2009; 56:14–20.2. Nitti VW, Lefkowitz G, Ficazzola M, Dixon CM. Lower urinary tract symptoms in young men: videourodynamic findings and correlation with noninvasive measures. J Urol. 2002; 168:135–138.3. Kaplan SA, Te AE, Jacobs BZ. Urodynamic evidence of vesical neck obstruction in men with misdiagnosed chronic nonbacterial prostatitis and the therapeutic role of endoscopic incision of the bladder neck. J Urol. 1994; 152(6 Pt 1):2063–2065.4. Wang CC, Yang SS, Chen YT, Hsieh JH. Videourodynamics identifies the causes of young men with lower urinary tract symptoms and low uroflow. Eur Urol. 2003; 43:386–390.5. Toh KL, Ng CK. Urodynamic studies in the evaluation of young men presenting with lower urinary tract symptoms. Int J Urol. 2006; 13:520–523.6. Kaplan SA, Ikeguchi EF, Santarosa RP, D'Alisera PM, Hendricks J, Te AE, et al. Etiology of voiding dysfunction in men less than 50 years of age. Urology. 1996; 47:836–839.7. Kaplan SA, Santarosa RP, D'Alisera PM, Fay BJ, Ikeguchi EF, Hendricks J, et al. Pseudodyssynergia (contraction of the external sphincter during voiding) misdiagnosed as chronic nonbacterial prostatitis and the role of biofeedback as a therapeutic option. J Urol. 1997; 157:2234–2237.8. Karami H, Valipour R, Lotfi B, Mokhtarpour H, Razi A. Urodynamic findings in young men with chronic lower urinary tract symptoms. Neurourol Urodyn. 2011; 30:1580–1585.9. Coyne KS, Tubaro A, Brubaker L, Bavendam T. Development and validation of patient-reported outcomes measures for overactive bladder: a review of concepts. Urology. 2006; 68:2 Suppl. 9–16.10. Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002; 21:261–274.11. Tubaro A, La Vecchia C. Uroscreening Study Group. The relation of lower urinary tract symptoms with life-style factors and objective measures of benign prostatic enlargement and obstruction: an Italian survey. Eur Urol. 2004; 45:767–772.12. Wein AJ. Lower urinary tract dysfunction in neurologic injury and disease. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders;2007. p. 2011–2045.13. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61:37–49.14. Glassberg KI, Combs AJ, Horowitz M. Nonneurogenic voiding disorders in children and adolescents: clinical and videourodynamic findings in 4 specific conditions. J Urol. 2010; 184:2123–2127.15. Padmanabhan P, Nitti VW. Primary bladder neck obstruction in men, women, and children. Curr Urol Rep. 2007; 8:379–384.16. Hruz P, Danuser H, Studer UE, Hochreiter WW. Non-inflammatory chronic pelvic pain syndrome can be caused by bladder neck hypertrophy. Eur Urol. 2003; 44:106–110.17. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236–237.18. Hellstrom WJ, Schmidt RA, Lue TF, Tanagho EA. Neuromuscular dysfunction in nonbacterial prostatitis. Urology. 1987; 30:183–188.19. Barbalias GA, Meares EM Jr, Sant GR. Prostatodynia: clinical and urodynamic characteristics. J Urol. 1983; 130:514–517.20. Jeong SJ, Lee SC, Jeong CW, Hong SK, Byun SS, Lee SE. Clinical and urodynamic differences among women with overactive bladder according to the presence of detrusor overactivity. Int Urogynecol J. 2013; 24:255–261.21. Elbadawi A, Yalla SV, Resnick NM. Structural basis of geriatric voiding dysfunction II Aging detrusor: normal versus impaired contractility. J Urol. 1993; 150(5 Pt 2):1657–1667.22. Resnick NM, Yalla SV, Laurino E. The pathophysiology of urinary incontinence among institutionalized elderly persons. N Engl J Med. 1989; 320:1–7.23. Guralnick ML, Grimsby G, Liss M, Szabo A, O'Connor RC. Objective differences between overactive bladder patients with and without urodynamically proven detrusor overactivity. Int Urogynecol J. 2010; 21:325–329.24. Hashim H, Abrams P. Is the bladder a reliable witness for predicting detrusor overactivity? J Urol. 2006; 175:191–194.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Pain and Urinary Symptoms by Chronic Prostatitis-like Symptoms on Quality of Life in Young Men
- Urodynamic Findings of Chronic Nonbacterial Prostatitis Patients with Urinary Symptoms
- Comparison of Lower Urinary Tract Symptoms and Urodynamic Study in BPH Patients with or without Prostatitis
- Chronic Bacterial Prostatitis
- Epidemiologic Study of Chronic Prostatitis-like Symptoms Surveyed among Young Men in the Area of Taejeon and Chung-nam: Prevalence and Influence of Weather