J Korean Acad Conserv Dent.
2011 May;36(3):211-218. 10.5395/JKACD.2011.36.3.211.
Clinical evaluation of a new extraction method for intentional replantation
- Affiliations
-
- 1Department of Conservative Dentistry, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea. yhchoi@snubh.org
- KMID: 1986685
- DOI: http://doi.org/10.5395/JKACD.2011.36.3.211
Abstract
- PURPOSE
Intentional replantation (IR) is a suitable treatment option when nonsurgical retreatment and periradicular surgery are unfeasible. For successful IR, fracture-free safe extraction is crucial step. Recently, a new extraction method of atraumatic safe extraction (ASE) for IR has been introduced.
PATIENTS AND METHODS
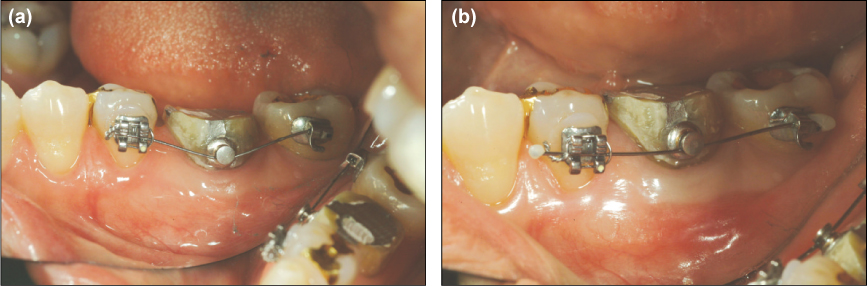
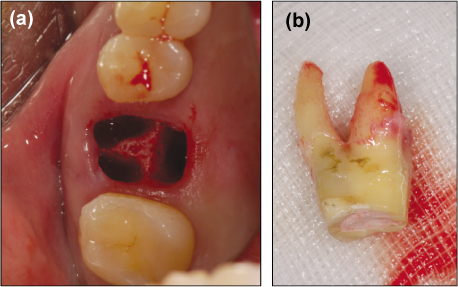
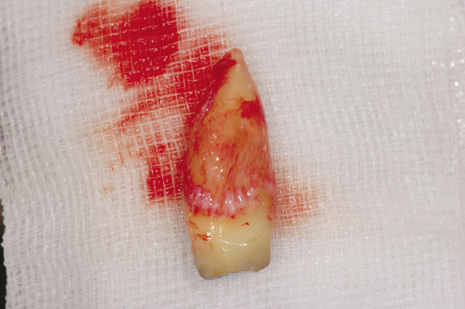
Ninety-six patients with the following conditions who underwent IR at the Department of Conservative Dentistry, Seoul National University Bundang Hospital, in 2010 were enrolled in this study: failed nonsurgical retreatment and periradicular surgery not recommended because of anatomical limitations or when rejected by the patient. Preoperative orthodontic extrusive force was applied for 2-3 weeks to increase mobility and periodontal ligament volume. A Physics Forceps was used for extraction and the success rate of ASE was assessed.
RESULTS
Ninety-six premolars and molars were treated by IR. The complete success rate (no crown and root fracture) was 93% (n = 89); the limited success rates because of partial root tip fracture and partial osteotomy were 2% (n = 2) and 5% (n = 5), respectively. The clinical and overall success rates of ASE were 95% and 100%, respectively; no failure was observed.
CONCLUSIONS
ASE can be regarded as a reproducible, predictable method of extraction for IR.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Surgical extrusion of a maxillary premolar after orthodontic extrusion: a retrospective study
Yong-Hoon Choi, Hyo-Jung Lee
J Korean Assoc Oral Maxillofac Surg. 2019;45(5):254-259. doi: 10.5125/jkaoms.2019.45.5.254.
Reference
-
1. Grossman LI. Intentional replantation of teeth: a clinical evaluation. J Am Dent Assoc. 1982. 104:633–639.
Article2. Kingsbury BC Jr, Wiesenbaugh JM Jr. Intentional replantation of mandibular premolars and molars. J Am Dent Assoc. 1971. 83:1053–1057.
Article3. Benenati FW. Intentional replantation of a mandibular second molar with long-term follow-up: report of a case. Dent Traumatol. 2003. 19:233–236.
Article4. Peer M. Intentional replantation - a 'last resort' treatment or a conventional treatment procedure? nine case reports. Dent Traumatol. 2004. 20:48–55.
Article5. Kratchman S. Intentional replantation. Dent Clin North Am. 1997. 41:603–617.6. Bender IB, Rossman LE. Intentional replantation of endodontically treated teeth. Oral Surg Oral Med Oral Pathol. 1993. 76:623–630.
Article7. Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994. 71:565–567.
Article8. Al-Shammari KF, Kazor CE, Wang HL. Molar root anatomy and management of furcation defects. J Clin Periodontol. 2001. 28:730–740.
Article9. Misch CE, Perez HM. Atraumatic extractions: a biomechanical rationale. Dent Today. 2008. 27:98100–101.10. Choi YH, Bae JH, Kim YK. Atraumatic safe extraction for intentional replantation. J Korean Dent Assoc. 2010. 48:531–537.11. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990. 63:529–536.
Article12. Hayashi H. Ortho-transplantation. 2006. 1st ed. Seoul: Narae Publishing Co.;18–28.13. Tsukiboshi M, Andreasen J, Asai Y. Autotransplantation of teeth. 2001. 1st ed. Tokyo: Quintessence;22–40.14. Kany FM. Single-tooth osteotomy for intention replantation. J Endod. 2002. 28:408–410.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intentional replantation with preapplication of orthodontic force on mandibular second molar
- Treatment of a tooth with severe periodontal involvement using intentional replantation: case report
- Short-term clinical outcome of intentionally replanted posterior molars
- Changes in periodontium after extraction of a periodontally-involved tooth in rats
- Surgical management with intentional replantation on a tooth with palato-radicular groove