J Cardiovasc Ultrasound.
2011 Dec;19(4):176-182. 10.4250/jcu.2011.19.4.176.
The Effect of Metabolic Syndrome on Myocardial Contractile Reserve during Exercise in Non-Diabetic Hypertensive Subjects
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea.
- 2Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea. haesunfree@hotmail.com
- KMID: 1980379
- DOI: http://doi.org/10.4250/jcu.2011.19.4.176
Abstract
- BACKGROUND
Metabolic syndrome (MS) is associated with increased left ventricular (LV) mass and diastolic dysfunction. This study uses relatively load-independent Doppler tissue echocardiography to examine whether MS is associated with decreased longitudinal contractile reserve during dynamic exercise.
METHODS
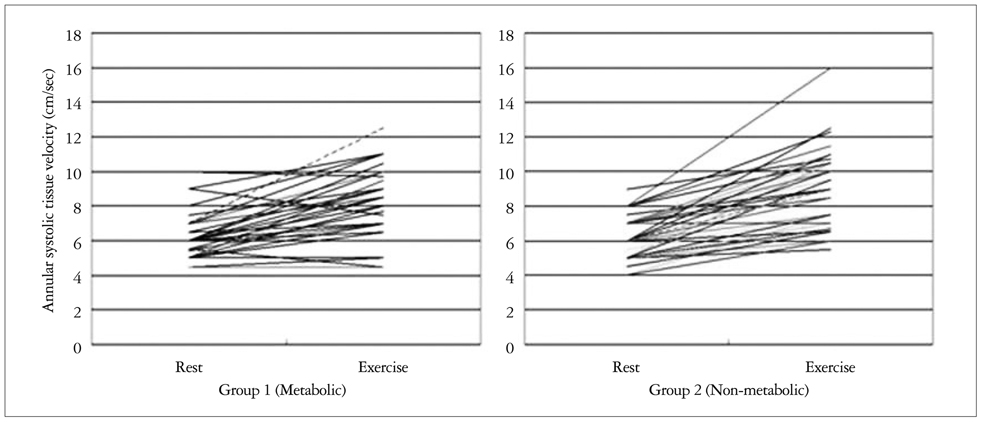
A total of 112 patients with relatively well-controlled, treated hypertension who complained of exertional dyspnea were enrolled (average age: 56.7 +/- 10.5 years). Fifty-six were non-diabetic patients with MS (Group 1), and 56 were age-sex matched hypertensive patients without MS (Group 2). Exercise stress echo was performed using a symptom-limited, multistage, supine bicycle exercise test. Multiple Doppler parameters were obtained at baseline, at each stage of exercise, and during recovery.
RESULTS
There was no significant difference between the two groups in terms of age, gender, and hemodynamic variables. E/E', an index of LV filling pressure, was significantly higher in the MS group at rest and during exercise. The longitudinal contractile reserve, the change in S' (longitudinal tissue velocity) from baseline to peak exercise, was significantly lower in the MS group (2.00 +/- 1.65 vs. 2.90 +/- 1.66, p = 0.015). Multiple regression analysis showed independent association of MS with longitudinal contractile reserve when controlled for confounding factors, such as LV mass index, gender, blood pressure, and age (beta = -0.235, p = 0.035).
CONCLUSION
Longitudinal contractile reserve was reduced in MS patients compared to others, although both groups demonstrated similar longitudinal contractile function at rest. We present the first demonstration that metabolic syndrome is independently associated with LV systolic dysfunction during exercise in hypertensive patients.
Figure
Reference
-
1. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001. 24:683–689.
Article2. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002. 288:2709–2716.
Article3. Schillaci G, Pirro M, Vaudo G, Gemelli F, Marchesi S, Porcellati C, Mannarino E. Prognostic value of the metabolic syndrome in essential hypertension. J Am Coll Cardiol. 2004. 43:1817–1822.
Article4. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan RS. Obesity and the risk of heart failure. N Engl J Med. 2002. 347:305–313.
Article5. Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, Dávila-Román VG. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004. 43:1399–1404.
Article6. Gustafsson F, Kragelund CB, Torp-Pedersen C, Seibaek M, Burchardt H, Akkan D, Thune JJ, Køber L. DIAMOND study group. Effect of obesity and being overweight on long-term mortality in congestive heart failure: influence of left ventricular systolic function. Eur Heart J. 2005. 26:58–64.
Article7. Wong CY, O'Moore-Sullivan T, Leano R, Byrne N, Beller E, Marwick TH. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation. 2004. 110:3081–3087.
Article8. Grandi AM, Maresca AM, Giudici E, Laurita E, Marchesi C, Solbiati F, Nicolini E, Guasti L, Venco A. Metabolic syndrome and morphofunctional characteristics of the left ventricle in clinically hypertensive nondiabetic subjects. Am J Hypertens. 2006. 19:199–205.
Article9. Sasso FC, Carbonara O, Nasti R, Marfella R, Esposito K, Rambaldi P, Mansi L, Salvatore T, Torella R, Cozzolino D. Effects of insulin on left ventricular function during dynamic exercise in overweight and obese subjects. Eur Heart J. 2005. 26:1205–1212.
Article10. Pascual M, Pascual DA, Soria F, Vicente T, Hernández AM, Tébar FJ, Valdés M. Effects of isolated obesity on systolic and diastolic left ventricular function. Heart. 2003. 89:1152–1156.
Article11. Iacobellis G, Ribaudo MC, Leto G, Zappaterreno A, Vecci E, Di Mario U, Leonetti F. Influence of excess fat on cardiac morphology and function: study in uncomplicated obesity. Obes Res. 2002. 10:767–773.
Article12. Trovato GM, Catalano D, Caruso G, Squatrito R, Venturino M, Degano C, Fazzio SD. Relationship between cardiac function and insulin resistance in obese patients. Diabetes Nutr Metab. 2001. 14:325–328.13. Lee WY, Park JS, Noh SY, Rhee EJ, Kim SW, Zimmet PZ. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Res Clin Pract. 2004. 65:143–149.
Article14. World Health Organization, International Association for the Study of Obesity, International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. 2000. Sydney: Health Communications.15. Quinones MA, Waggoner AD, Reduto LA, Nelson JG, Young JB, Winters WL Jr, Ribeiro LG, Miller RR. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981. 64:744–753.
Article16. Ha JW, Oh JK, Pellikka PA, Ommen SR, Stussy VL, Bailey KR, Seward JB, Tajik AJ. Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography. J Am Soc Echocardiogr. 2005. 18:63–68.
Article17. Wong CY, O'Moore-Sullivan T, Fang ZY, Haluska B, Leano R, Marwick TH. Myocardial and vascular dysfunction and exercise capacity in the metabolic syndrome. Am J Cardiol. 2005. 96:1686–1691.
Article18. Sundström J, Lind L, Nyström N, Zethelius B, Andrén B, Hales CN, Lithell HO. Left ventricular concentric remodeling rather than left ventricular hypertrophy is related to the insulin resistance syndrome in elderly men. Circulation. 2000. 101:2595–2600.
Article19. Paolisso G, Galderisi M, Tagliamonte MR, de Divitis M, Galzerano D, Petrocelli A, Gualdiero P, de Divitis O, Varricchio M. Myocardial wall thickness and left ventricular geometry in hypertensives. Relationship with insulin. Am J Hypertens. 1997. 10:1250–1256.
Article20. Cuspidi C, Meani S, Fusi V, Severgnini B, Valerio C, Catini E, Leonetti G, Magrini F, Zanchetti A. Metabolic syndrome and target organ damage in untreated essential hypertensives. J Hypertens. 2004. 22:1991–1998.
Article21. Burchfiel CM, Skelton TN, Andrew ME, Garrison RJ, Arnett DK, Jones DW, Taylor HA Jr. Metabolic syndrome and echocardiographic left ventricular mass in blacks: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2005. 112:819–827.
Article22. Palmieri V, Bella JN, Arnett DK, Liu JE, Oberman A, Schuck MY, Kitzman DW, Hopkins PN, Morgan D, Rao DC, Devereux RB. Effect of type 2 diabetes mellitus on left ventricular geometry and systolic function in hypertensive subjects: Hypertension Genetic Epidemiology Network (HyperGEN) study. Circulation. 2001. 103:102–107.
Article23. Milani RV, Lavie CJ, Ventura HO, Kurtz J, Messerli FH. Effect of left ventricular remodeling on mortality in 35,602 patients with normal systolic function. J Am Coll Cardiol. 2003. 41:459A.
Article24. Brutsaert DL, De Keulenaer GW. Diastolic heart failure: a myth. Curr Opin Cardiol. 2006. 21:240–248.
Article25. Aurigemma GP, Silver KH, Priest MA, Gaasch WH. Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol. 1995. 26:195–202.
Article26. Vinereanu D, Nicolaides E, Tweddel AC, Fraser AG. "Pure" diastolic dysfunction is associated with long-axis systolic dysfunction. Implications for the diagnosis and classification of heart failure. Eur J Heart Fail. 2005. 7:820–828.
Article27. Jones CJ, Raposo L, Gibson DG. Functional importance of the long axis dynamics of the human left ventricle. Br Heart J. 1990. 63:215–220.
Article28. Derumeaux G, Ovize M, Loufoua J, André-Fouet X, Minaire Y, Cribier A, Letac B. Doppler tissue imaging quantitates regional wall motion during myocardial ischemia and reperfusion. Circulation. 1998. 97:1970–1977.
Article29. Nikitin NP, Witte KK, Thackray SD, de Silva R, Clark AL, Cleland JG. Longitudinal ventricular function: normal values of atrioventricular annular and myocardial velocities measured with quantitative two-dimensional color Doppler tissue imaging. J Am Soc Echocardiogr. 2003. 16:906–921.
Article30. Al Suwaidi J, Higano ST, Holmes DR Jr, Lennon R, Lerman A. Obesity is independently associated with coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteries. J Am Coll Cardiol. 2001. 37:1523–1528.
Article31. Turhan H, Erbay AR, Yasar AS, Bicer A, Sasmaz H, Yetkin E. Impaired coronary blood flow in patients with metabolic syndrome: documented by Thrombolysis in Myocardial Infarction (TIMI) frame count method. Am Heart J. 2004. 148:789–794.
Article32. Engeli S, Negrel R, Sharma AM. Physiology and pathophysiology of the adipose tissue renin-angiotensin system. Hypertension. 2000. 35:1270–1277.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Metabolic Syndrome on Myocardial Contractile Reserve during Exercise in Non-Diabetic Hypertensive Subjects
- Metabolic Syndrome and Myocardial Contractile Reserve
- Exercise Therapy for Hypertensive Patients
- Diabetic Cardiomyopathy
- Myocardial fractional flow reserve in acute myocardial infarction