J Cardiovasc Ultrasound.
2011 Jun;19(2):76-82. 10.4250/jcu.2011.19.2.76.
Prevalence and Patterns of Left Ventricular Dysfunction in Patients with Pheochromocytoma
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, School of Medicine, Chungnam National University, Regional Cardiocerebrovascular Center, Chungnam National University Hospital, Daejeon, Korea. jaehpark@cnuh.co.kr
- 2Department of Surgery, School of Medicine, Chungnam National University, Regional Cardiocerebrovascular Center, Chungnam National University Hospital, Daejeon, Korea.
- KMID: 1980355
- DOI: http://doi.org/10.4250/jcu.2011.19.2.76
Abstract
- BACKGROUND
Excessive catecholamine release in pheochromocytoma is known to cause transient reversible left ventricular (LV) dysfunction, such as in the case of pheochromocytoma-associated catecholamine cardiomyopathy. We investigated patterns of clinical presentation and incidence of LV dysfunction in patients with pheochromocytoma.
METHODS
From January 2004 to April 2011, consecutive patients with pheochromocytoma were retrospectively studied with clinical symptoms, serum catecholamine profiles, and radiologic findings. Patterns of electrocardiography and echocardiography were also analyzed.
RESULTS
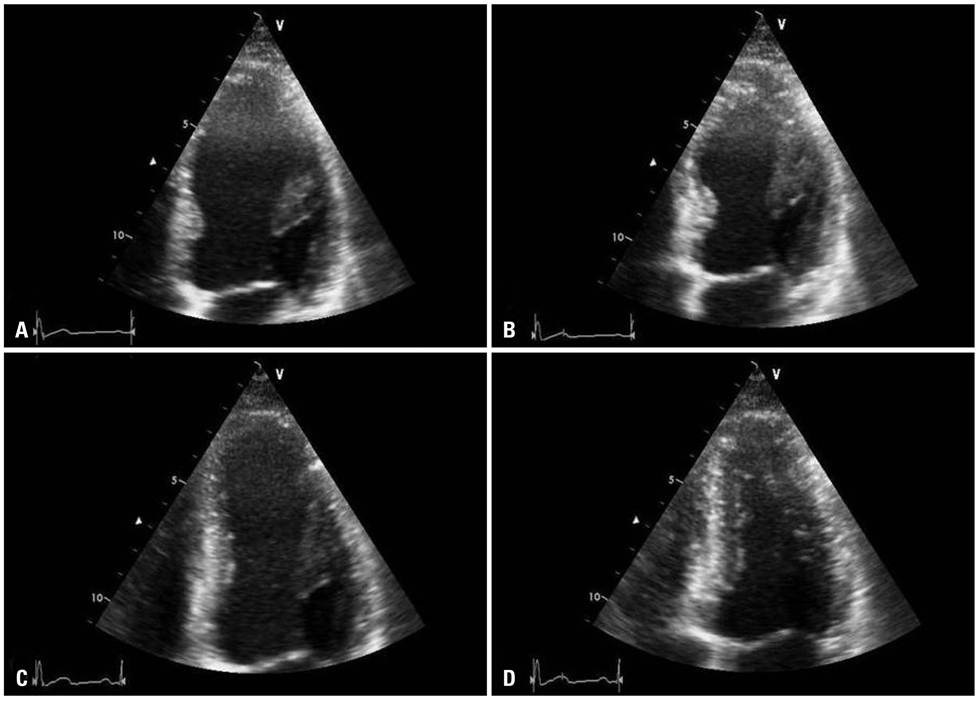
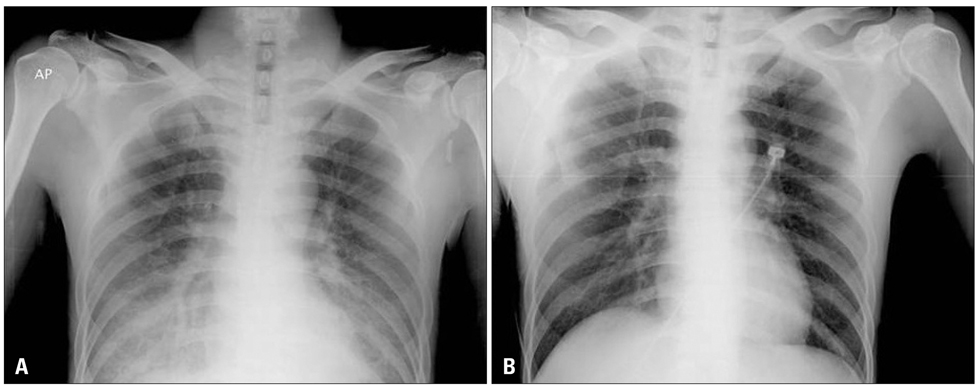
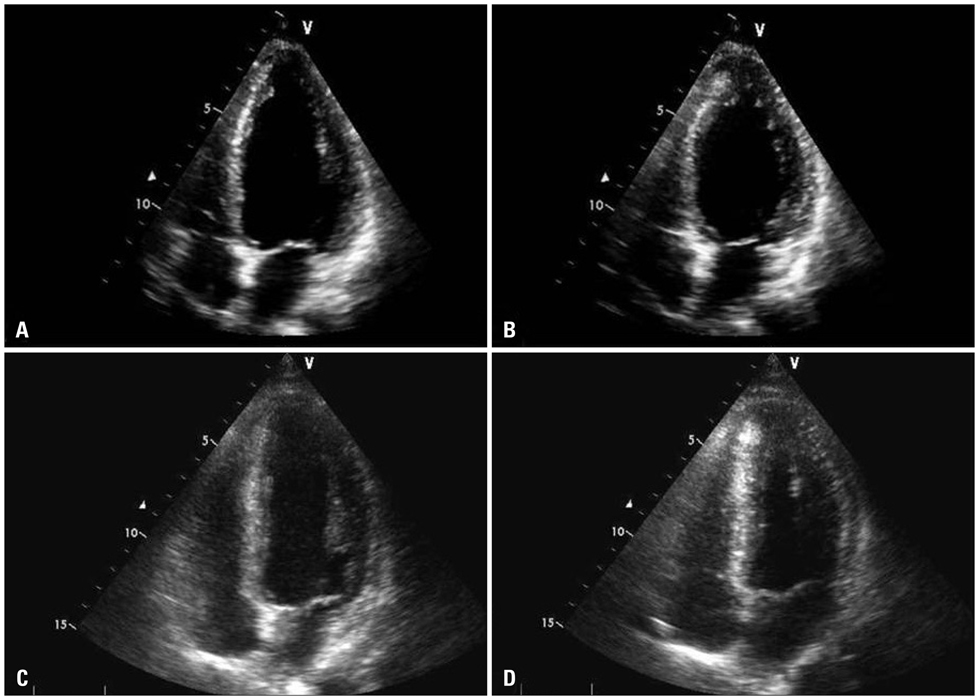
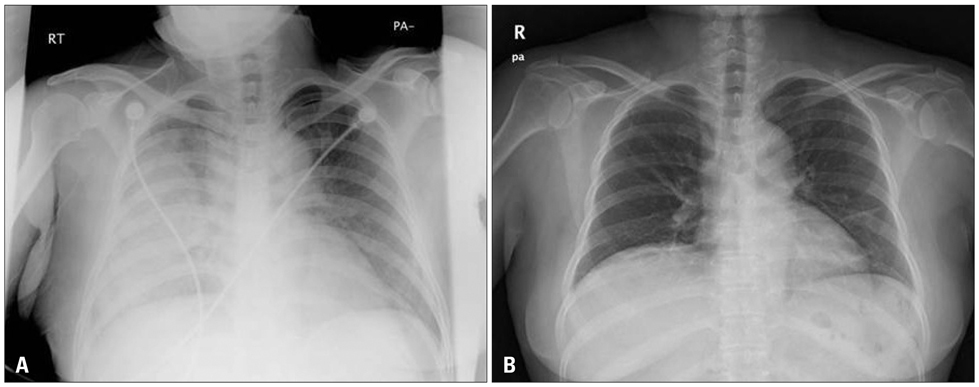
During the study period, a total of 36 patients (21 males, 49.8 +/- 15.8 years, range 14-81 years) with pheochromocytoma were included. In the electrocardiographic examinations, normal findings were the most common findings (19, 52.8%). LV hypertrophy in 12 cases (33.3%), sinus tachycardia in 3 (8.3%), ischemic pattern in 1 (2.8%) and supraventricular tachycardia in 1 (2.8%). Echocardiographic exam was done in 29 patients (80.6%). Eighteen patients (62.1%) showed normal finding, 8 (27.6%) revealed concentric LV hypertrophy with normal LV systolic function, and 3 (10.3%) demonstrate LV systolic dysfunction (LV ejection fraction < 50%). Three showed transient LV dysfunction (2 with inverted Takotsubo-type cardiomyopathy and 1 with a diffuse hypokinesia pattern). Common presenting symptoms in the 3 cases were new onset chest discomfort and dyspnea which were not common in the other patients. Their echocardiographic abnormalities were normalized with conventional treatment within 3 days.
CONCLUSION
Out of total 36 patients with pheochromocytoma, 3 showed transient LV systolic dysfunction (catecholamine cardiomyopathy). Pheochromocytoma should be included as one of possible causes of transient LV systolic dysfunction.
MeSH Terms
Figure
Reference
-
1. Sheps SG, Jiang NS, Klee GG, van Heerden JA. Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clin Proc. 1990. 65:88–95.
Article2. Bravo EL, Gifford RW Jr. Current concepts. Pheochromocytoma: diagnosis, localization and management. N Engl J Med. 1984. 311:1298–1303.
Article3. Wood R, Commerford PJ, Rose AG, Tooke A. Reversible catecholamine-induced cardiomyopathy. Am Heart J. 1991. 121:610–613.
Article4. Bybee KA, Prasad A. Stress-related cardiomyopathy syndromes. Circulation. 2008. 118:397–409.
Article5. Gerlo EA, Sevens C. Urinary and plasma catecholamines and urinary catecholamine metabolites in pheochromocytoma: diagnostic value in 19 cases. Clin Chem. 1994. 40:250–256.
Article6. Moyer TP, Jiang NS, Tyce GM, Sheps SG. Analysis for urinary catecholamines by liquid chromatography with amperometric detection: methodology and clinical interpretation of results. Clin Chem. 1979. 25:256–263.
Article7. Stein PP, Black HR. A simplified diagnostic approach to pheochromocytoma. A review of the literature and report of one institution's experience. Medicine (Baltimore). 1991. 70:46–66.
Article8. Shub C, Cueto-Garcia L, Sheps SG, Ilstrup DM, Tajik AJ. Echocardiographic findings in pheochromocytoma. Am J Cardiol. 1986. 57:971–975.
Article9. Bolli R, Marbán E. Molecular and cellular mechanisms of myocardial stunning. Physiol Rev. 1999. 79:609–634.
Article10. Yamanaka O, Yasumasa F, Nakamura T, Ohno A, Endo Y, Yoshimi K, Miura K, Yamaguchi H. "Myocardial stunning"-like phenomenon during a crisis of pheochromocytoma. Jpn Circ J. 1994. 58:737–742.
Article11. Shaw TR, Rafferty P, Tait GW. Transient shock and myocardial impairment caused by phaeochromocytoma crisis. Br Heart J. 1987. 57:194–198.
Article12. Schuiki ER, Jenni R, Amann FW, Ziegler WH. A reversible form of apical left ventricular hypertrophy associated with pheochromocytoma. J Am Soc Echocardiogr. 1993. 6:327–331.
Article13. Takizawa M, Kobayakawa N, Uozumi H, Yonemura S, Kodama T, Fukusima K, Takeuchi H, Kaneko Y, Kaneko T, Fujita K, Honma Y, Aoyagi T. A case of transient left ventricular ballooning with pheochromocytoma, supporting pathogenetic role of catecholamines in stress-induced cardiomyopathy or takotsubo cardiomyopathy. Int J Cardiol. 2007. 114:e15–e17.
Article14. Lassnig E, Weber T, Auer J, Nömeyer R, Eber B. Pheochromocytoma crisis presenting with shock and tako-tsubo-like cardiomyopathy. Int J Cardiol. 2009. 134:e138–e140.
Article15. Hurst RT, Askew JW, Reuss CS, Lee RW, Sweeney JP, Fortuin FD, Oh JK, Tajik AJ. Transient midventricular ballooning syndrome: a new variant. J Am Coll Cardiol. 2006. 48:579–583.16. Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, Honda T, Hase M, Kai R, Morii I. Angina Pectoris-Myocardial Infarction Investigations in Japan. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001. 38:11–18.
Article17. Lacy CR, Contrada RJ, Robbins ML, Tannenbaum AK, Moreyra AE, Chelton S, Kostis JB. Coronary vasoconstriction induced by mental stress (simulated public speaking). Am J Cardiol. 1995. 75:503–505.
Article18. Pierpont GL, DeMaster EG, Cohn JN. Regional differences in adrenergic function within the left ventricle. Am J Physiol. 1984. 246:H824–H829.
Article19. Kawano H, Okada R, Yano K. Histological study on the distribution of autonomic nerves in the human heart. Heart Vessels. 2003. 18:32–39.
Article20. Kim EM, Park JH, Park YS, Lee JH, Choi SW, Jeong JO, Seong IW. Catecholamines may play an important role in the pathogenesis of transient mid- and basal ventricular ballooning syndrome. J Korean Med Sci. 2008. 23:898–902.
Article21. Kim S, Yu A, Filippone LA, Kolansky DM, Raina A. Inverted-Takotsubo pattern cardiomyopathy secondary to pheochromocytoma: a clinical case and literature review. Clin Cardiol. 2010. 33:200–205.
Article22. Kim TS, Chu EH, Kang HH, Chun SW, Cho EJ, Kim JH. A case of reversal of takotsubo cardiomyopathy in patient with pheochromocytoma. J Cardiovasc Ultrasound. 2007. 15:50–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Catecholamine-Induced Cardiomyopathy in a Patient With a Pheochromocytoma
- A Case of Normalized Hypertrophic Cardiomyopathy after Removal of Pheochromocytoma
- Reversal of Dilated Cardiomyopathy with medical therapy in a case of Pheochromocytoma
- A Case of Malignant Pheochromocytoma Presenting as Inverted Takotsubo-Like Cardiomyopathy
- The Role of Doppler Time Index for Evaluation of Left Ventricular Diastolic Function by Patterns of Left Ventricular Hypertrophy in Hypertensive Patients