Korean J Gastroenterol.
2014 Oct;64(4):224-228. 10.4166/kjg.2014.64.4.224.
Overtube-related Delayed Esophageal Perforation with Mediastinitis
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University Hospital, Konkuk University School of Medicine, Seoul, Korea. 20050101@kuh.ac.kr
- 2Department of Radiology, Konkuk University Hospital, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 1979207
- DOI: http://doi.org/10.4166/kjg.2014.64.4.224
Abstract
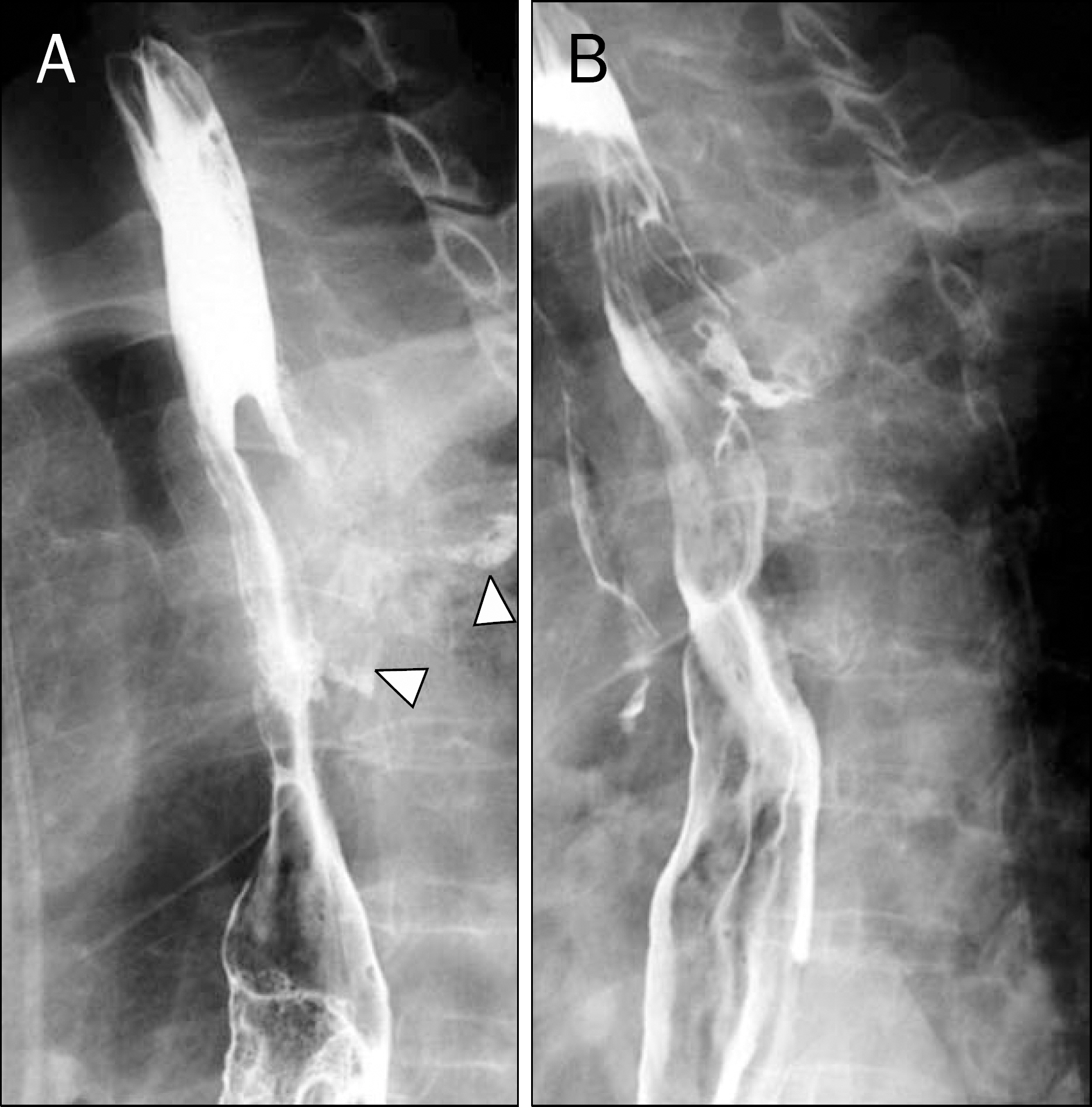
- Overtube provides a conduit for the passage of endoscope into the digestive tract. Esophageal perforation with mediastinitis is a rare overtube-related complication. Until now, no reports have been published regarding the esophageal perforation which developed many months after the original procedure using the overtube. A 56-year-old female visited our hospital complaining of chest pain and back pain that began 14 days ago. The patient underwent esophageal variceal ligation using the overtube 12 months earlier. She was diagnosed with esophageal perforation with mediastinitis which extended to intervertebral and epidural space. The cause of this condition was considered to have been related to the use of overtube. Management of delayed perforation remains controversial. Although surgical management might be the preferred mode of treatment, she underwent local N-butyl 2-cyanoacrylate injection therapy and temporary stent therapy with antibiotics due to high operative risk. Herein, we report a case of overtube-related delayed esophageal perforation with mediastinitis that was successfully treated by nonoperative management.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Schmitz RJ, Sharma P, Badr AS, Qamar MT, Weston AP. Incidence and management of esophageal stricture formation, ulcer bleeding, perforation, and massive hematoma formation from sclerotherapy versus band ligation. Am J Gastroenterol. 2001; 96:437–441.
Article2. Goldschmiedt M, Haber G, Kandel G, Kortan P, Marcon N. A safe-ty maneuver for placing overtubes during endoscopic variceal ligation. Gastrointest Endosc. 1992; 38:399–400.
Article3. Lindenmann J, Matzi V, Neuboeck N, et al. Management of esophageal perforation in 120 consecutive patients: clinical impact of a structured treatment algorithm. J Gastrointest Surg. 2013; 17:1036–1043.
Article4. Carrott PW Jr, Low DE. Advances in the management of esophageal perforation. Thorac Surg Clin. 2011; 21:541–555.
Article5. Wells CD, Fleischer DE. Overtubes in gastrointestinal endoscopy. Am J Gastroenterol. 2008; 103:745–752.
Article6. Dinning JP, Jaffe PE. Delayed presentation of esophageal perforation as a result of overtube placement. J Clin Gastroenterol. 1997; 24:250–252.
Article7. Michel L, Grillo HC, Malt RA. Operative and nonoperative management of esophageal perforations. Ann Surg. 1981; 194:57–63.
Article8. Hasan S, Jilaihawi AN, Prakash D. Conservative management of iatrogenic oesophageal perforations–a viable option. Eur J Car-diothorac Surg. 2005; 28:7–10.9. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004; 77:1475–1483.
Article10. Kim HG, Cho JW, Park SJ, et al. Two cases of alimentary tract fistula treated by endoscopic local injection therapy. Korean J Gastrointest Endosc. 2003; 26:426–430.11. van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ. Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol. 2010; 105:1515–1520.
Article12. Radecke K, Gerken G, Treichel U. Impact of a self-expanding, plastic esophageal stent on various esophageal stenoses, fistu- las, and leakages: a single-center experience in 39 patients. Gastrointest Endosc. 2005; 61:812–818.13. Langer FB, Wenzl E, Prager G, et al. Management of post-operative esophageal leaks with the Polyflex self-expanding cov-ered plastic stent. Ann Thorac Surg. 2005; 79:398–403.
Article14. Shim CS. Esophageal stent for cervical esophagus and esophagogastric junction. Clin Endosc. 2012; 45:235–239.
Article15. El Hajj II, Imperiale TF, Rex DK, et al. Treatment of esophageal leaks, fistulae, and perforations with temporary stents: evaluation of efficacy, adverse events, and factors associated with successful outcomes. Gastrointest Endosc. 2014; 79:589–598.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Esophageal Perforation during Endoscopic Variceal Ligation
- Mediastinitis and Pneumomediastinum in a Preterm Infant with Iatrogenic Esophageal Perforation: A Case Report
- Mediastinitis due to Esophageal Perforation as a Complication of Diagnostic Esophagogastroduodenoscopy
- Endoscopic Vacuum-assisted Closure in a Patient with an Overtube-induced Esophageal Perforation
- Acute Phlegmonous Esophagitis with Mediastinitis Complicated by an Esophageal Perforation: A Case Report