Korean J Orthod.
2011 Jun;41(3):164-173. 10.4041/kjod.2011.41.3.164.
Gender-wise analysis of the cephalometric factors affecting obstructive sleep apnea
- Affiliations
-
- 1Department of Dentistry, College of Medicine, Keimyung University, Korea. hsh99@dsmc.or.kr
- KMID: 1975428
- DOI: http://doi.org/10.4041/kjod.2011.41.3.164
Abstract
OBJECTIVE
The purpose of this study was to perform gender-wise analysis of the related cephalometric factors affecting Korean patients with obstructive sleep apnea (OSA).
METHODS
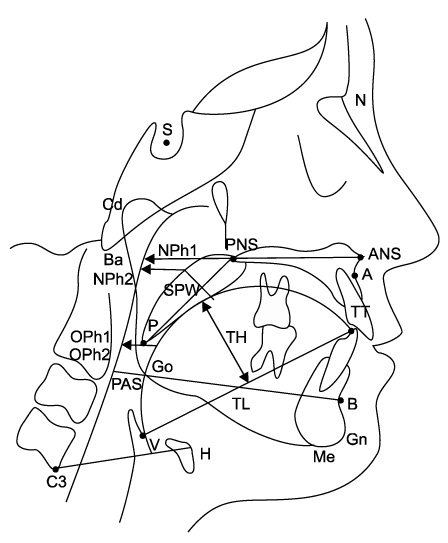
We examined 118 adults who had visited the Sleep Disorder Clinic Center in Keimyung university, Daegu, Korea, and evaluated them by using polysomnography (PSG) and lateral cephalograms. The patients were divided into 4 groups (male simple snorers, male OSA patients, female simple snorers, and female OSA patients) according to AHI (apnea-hypopnea index) and sex.
RESULTS
The position of the hyoid bone in the female OSA group was inferior to that in the female simple snorer group. Multiple regression analysis showed that tongue length and soft palate width were significant determinants for the severity of AHI in male OSA patients. However, inferior position of the hyoid was a significant determinant only in women.
CONCLUSIONS
From a cephalometric point of view, OSA in male and female adult patients may be characterized by different pathogeneses. In particular, in female OSA patients, they might be managed by individualized treatments such as hormone replacement therapy in addition to conventional treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Banno K, Kryger MH. Sleep apnea: clinical investigations in humans. Sleep Med. 2007. 8:400–426.
Article2. Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976. 27:465–484.
Article3. The Report of an American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999. 22:667–689.4. Hoffstein V, Mateika S. Differences in abdominal and neck circumferences in patients with and without obstructive sleep apnoea. Eur Respir J. 1992. 5:377–381.5. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993. 328:1230–1235.
Article6. Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001. 163:608–613.7. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004. 170:1108–1113.
Article8. Practice parameters for the indications for polysomnography and related procedures. Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Sleep. 1997. 20:406–422.9. Haraldsson PO, Carenfelt C, Diderichsen F, Nygren A, Tingvall C. Clinical symptoms of sleep apnea syndrome and automobile accidents. ORL J Otorhinolaryngol Relat Spec. 1990. 52:57–62.
Article10. George CF, Smiley A. Sleep apnea & automobile crashes. Sleep. 1999. 22:790–795.11. Riley R, Guilleminault C, Herran J, Powell N. Cephalometric analyses and flow-volume loops in obstructive sleep apnea patients. Sleep. 1983. 6:303–311.
Article12. Tangugsorn V, Krogstad O, Espeland L, Lyberg T. Obstructive sleep apnea: a canonical correlation of cephalometric and selected demographic variables in obese and nonobese patients. Angle Orthod. 2001. 71:23–35.13. Ono T, Lowe AA, Ferguson KA, Fleetham JA. Associations among upper airway structure, body position, and obesity in skeletal Class I male patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996. 109:625–634.
Article14. Guilleminault C, Quera-Salva MA, Partinen M, Jamieson A. Women and the obstructive sleep apnea syndrome. Chest. 1988. 93:104–109.
Article15. Ong KC, Clerk AA. Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med. 1998. 92:843–848.
Article16. Li KK, Powell NB, Kushida C, Riley RW, Adornato B, Guilleminault C. A comparison of Asian and white patients with obstructive sleep apnea syndrome. Laryngoscope. 1999. 109:1937–1940.
Article17. Liu Y, Lowe AA, Zeng X, Fu M, Fleetham JA. Cephalometric comparisons between Chinese and Caucasian patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2000. 117:479–485.
Article18. Hwang SH, Park IS, Nam KY, Kim JB, Cho YW, Suh YS, et al. Cephalometric differences in obstructive sleep apnea between obese and non-obese Korean male patients. Korean J Orthod. 2008. 38:202–213.
Article19. Walker RP, Durazo-Arvizu R, Wachter B, Gopalsami C. Preoperative differences between male and female patients with sleep apnea. Laryngoscope. 2001. 111:1501–1505.
Article20. Yu X, Fujimoto K, Urushibata K, Matsuzawa Y, Kubo K. Cephalometric analysis in obese and nonobese patients with obstructive sleep apnea syndrome. Chest. 2003. 124:212–218.
Article21. Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ. Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax. 1999. 54:323–328.
Article22. deBerry-Borowiecki B, Kukwa A, Blanks RH. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988. 98:226–234.
Article23. Tsuchiya M, Lowe AA, Pae EK, Fleetham JA. Obstructive sleep apnea subtypes by cluster analysis. Am J Orthod Dentofacial Orthop. 1992. 101:533–542.
Article24. Cistulli PA, Grunstein RR, Sullivan CE. Effect of testosterone administration on upper airway collapsibility during sleep. Am J Respir Crit Care Med. 1994. 149(2 Pt 1):530–532.
Article25. Regensteiner JG, Woodard WD, Hagerman DD, Weil JV, Pickett CK, Bender PR, et al. Combined effects of female hormones and metabolic rate on ventilatory drives in women. J Appl Physiol. 1989. 66:808–813.
Article26. Popovic RM, White DP. Upper airway muscle activity in normal women: influence of hormonal status. J Appl Physiol. 1998. 84:1055–1062.
Article27. Greenberg-Dotan S, Reuveni H, Simon-Tuval T, Oksenberg A, Tarasiuk A. Gender differences in morbidity and health care utilization among adult obstructive sleep apnea patients. Sleep. 2007. 30:1173–1180.
Article28. Valipour A, Lothaller H, Rauscher H, Zwick H, Burghuber OC, Lavie P. Gender-related differences in symptoms of patients with suspected breathing disorders in sleep: a clinical population study using the sleep disorders questionnaire. Sleep. 2007. 30:312–319.
Article29. Suarez EC. Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. Brain Behav Immun. 2008. 22:960–968.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mean values of cephalometric analysis from Korean adults with abnormal occlusion in relation to the diagnosis of obstructive sleep apnea syndrome
- Predictors for Presence and Severity of Obstructive Sleep Apnea in Snoring Patients: Significance of Neck Circumference
- The Clinical Usefulness of Cephalometric Analysis in the Obstructive Sleep Apnea Syndrome
- Effects of Menopause on Obstructive Sleep Apnea
- Measuring and Predicting Success of Uvulopalatopharyngoplasty in Obstructive Sleep Apnea Patients