Korean J Orthod.
2014 May;44(3):119-127. 10.4041/kjod.2014.44.3.119.
Long-term stability of dentoalveolar, skeletal, and soft tissue changes after non-extraction treatment with a self-ligating system
- Affiliations
-
- 1Department of Orthodontics, Faculty of Dentistry, Selcuk University, Konya, Turkey. zehra.ileri@gmail.com
- KMID: 1974997
- DOI: http://doi.org/10.4041/kjod.2014.44.3.119
Abstract
OBJECTIVE
To evaluate the long-term effects of self-ligating brackets (SLBs) on transverse dimensions of arches and skeletal and soft tissues and to quantitatively evaluate the treatment outcome after non-extraction treatment with SLBs.
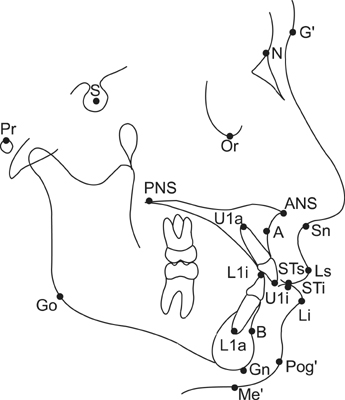
METHODS
The sample consisted of 24 (18 female and six male) subjects, with a mean age of 14.23 +/- 2.19 years, who received treatment with the Damon(R)3 appliances. Complete records including cephalometric radiographs and plaster models were obtained before treatment (T1), immediately after treatment (T2), six months after treatment (T3), and two years (T4) after treatment. Digital study models were generated. Twenty lateral cephalometric, six frontal cephalometric, and eight dental cast measurements were examined. The Peer Assessment Rating index was used to measure the treatment outcome. The Wilcoxon test was applied for statistical analysis of the changes.
RESULTS
There were significant increases in all transverse dental cast measurements with active treatment. There was some significant relapse in the long term, particularly in maxillary width (p < 0.05). Statistically significant increases were found in nasal (p < 0.001), maxillary base, upper molar, lower intercanine, and antigonial (p < 0.05) widths in T1-T2. Lower incisors were proclined and protruded in T1-T2.
CONCLUSIONS
SLBs correct crowding by mechanisms involving incisor proclination and protrusion and expansion of the dental arches, without induction of clinically significant changes in hard and soft tissues of the face.
Keyword
Figure
Reference
-
1. Weinberg M, Sadowsky C. Resolution of mandibular arch crowding in growing patients with Class I malocclusions treated nonextraction. Am J Orthod Dentofacial Orthop. 1996; 110:359–364.
Article2. Fleming PS, DiBiase AT, Sarri G, Lee RT. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009; 136:340–347.
Article3. Burke SP, Silveira AM, Goldsmith LJ, Yancey JM, Van Stewart A, Scarfe WC. A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod. 1998; 68:53–60.4. Mills JR. The long-term results of the proclination of lower incisors. Br Dent J. 1966; 120:355–363.5. Little RM. Stability and relapse of mandibular anterior alignment: University of Washington studies. Semin Orthod. 1999; 5:191–204.
Article6. Harradine NW. Self-ligating brackets: where are we now? J Orthod. 2003; 30:262–273.
Article7. Eberting JJ, Straja SR, Tuncay OC. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001; 4:228–234.
Article8. Harradine NW. Self-ligating brackets and treatment efficiency. Clin Orthod Res. 2001; 4:220–227.
Article9. Kim H, Kim KY, Kang YG, Kim SH, Kook YA. Clinical considerations with self-ligating brackets. Korean J Orthod. 2006; 36:474–482.10. Pandis N, Polychronopoulou A, Makou M, Eliades T. Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets. Eur J Orthod. 2010; 32:248–253.
Article11. Damon DH. The rationale, evolution and clinical application of the self-ligating bracket. Clin Orthod Res. 1998; 1:52–61.
Article12. Damon DH. The Damon low-friction bracket: a biologically compatible straight-wire system. J Clin Orthod. 1998; 32:670–680.13. Pandis N, Polychronopoulou A, Katsaros C, Eliades T. Comparative assessment of conventional and self-ligating appliances on the effect of mandibular intermolar distance in adolescent nonextraction patients: a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011; 140:e99–e105.
Article14. Cattaneo PM, Treccani M, Carlsson K, Thorgeirsson T, Myrda A, Cevidanes LH, et al. Transversal maxillary dento-alveolar changes in patients treated with active and passive self-ligating brackets: a randomized clinical trial using CBCT-scans and digital models. Orthod Craniofac Res. 2011; 14:222–233.
Article15. Scott P, DiBiase AT, Sherriff M, Cobourne MT. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2008; 134:470.e1–470.e8.
Article16. Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR Index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod. 1992; 14:180–187.
Article17. Birkeland K, Furevik J, Bøe OE, Wisth PJ. Evaluation of treatment and post-treatment changes by the PAR Index. Eur J Orthod. 1997; 19:279–288.
Article18. Stalpers MJ, Booij JW, Bronkhorst EM, Kuijpers-Jagtman AM, Katsaros C. Extraction of maxillary first permanent molars in patients with Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2007; 132:316–323.
Article19. Freitas KM, Freitas DS, Valarelli FP, Freitas MR, Janson G. PAR evaluation of treated Class I extraction patients. Angle Orthod. 2008; 78:270–274.
Article20. Tweed CH. The application of the principles of the edgewise arch in the treatment of class II, division 1, malocclusion. Angle Orthod. 1936; 6:198–208.21. Peck S. So what's new? Arch expansion, again. Angle Orthod. 2008; 78:574–575.
Article22. Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 2007; 132:208–215.
Article23. Kuijpers-Jagtman AM, Al Yami EA, van't Hof MA. Long-term stability of orthodontic treatment. Ned Tijdschr Tandheelkd. 2000; 107:178–181.24. Tecco S, Tetè S, Perillo L, Chimenti C, Festa F. Maxillary arch width changes during orthodontic treatment with fixed self-ligating and traditional straight-wire appliances. World J Orthod. 2009; 10:290–294.25. Yu YL, Tang GH, Gong FF, Chen LL, Qian YF. A comparison of rapid palatal expansion and Damon appliance on non-extraction correction of dental crowding. Shanghai Kou Qiang Yi Xue. 2008; 17:237–242.26. DiBiase AT, Nasr IH, Scott P, Cobourne MT. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients: a prospective randomized clinical trial. Am J Orthod Dentofacial Orthop. 2011; 139:e111–e116.
Article27. Machibya FM, Bao X, Zhao L, Hu M. Treatment time, outcome, and anchorage loss comparisons of self-ligating and conventional brackets. Angle Orthod. 2013; 83:280–285.
Article28. Poulton D, Vlaskalic V, Baumrind S. Treatment outcomes in 4 modes of orthodontic practice. Am J Orthod Dentofacial Orthop. 2005; 127:351–354.
Article29. Ileri Z, Basciftci FA, Malkoc S, Ramoglu SI. Comparison of the outcomes of the lower incisor extraction, premolar extraction and non-extraction treatments. Eur J Orthod. 2012; 34:681–685.
Article30. Hess DR. Retrospective studies and chart reviews. Respir Care. 2004; 49:1171–1174.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mandibular arch orthodontic treatment stability using passive self-ligating and conventional systems in adults: A randomized controlled trial
- An Evaluation of Postoperative Stability and Soft-tissue Changes of the Long Face Syndrome Patients
- Analysis of dentoalveolar compensation and discrimination of skeletal types
- Dentoalveolar Compensation according to Skeletal Patterns of Normal Occlusion
- Camouflage treatment in adult skeletal Class III cases by extraction of two lower premolars