Tuberc Respir Dis.
2006 Nov;61(5):484-489. 10.4046/trd.2006.61.5.484.
A Case of Primary Endobronchial Leiomyosarcoma Noticed by Massive Hemoptysis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Masan Samsung Hospital, Sungkyunkwan University School of Medicine, Masan, Korea. kangkw9@naver.com
- KMID: 1970255
- DOI: http://doi.org/10.4046/trd.2006.61.5.484
Abstract
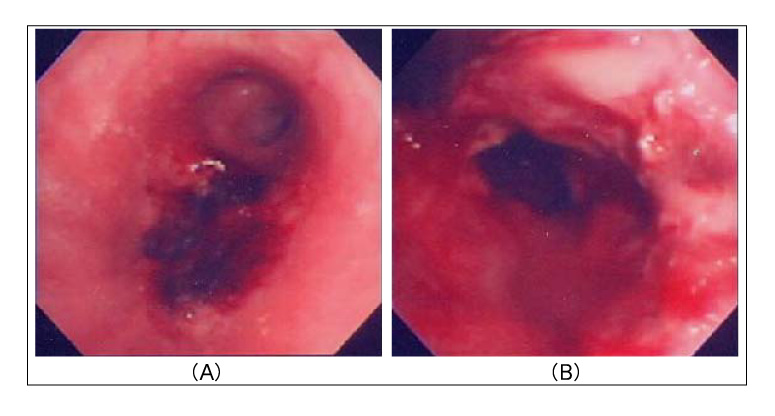
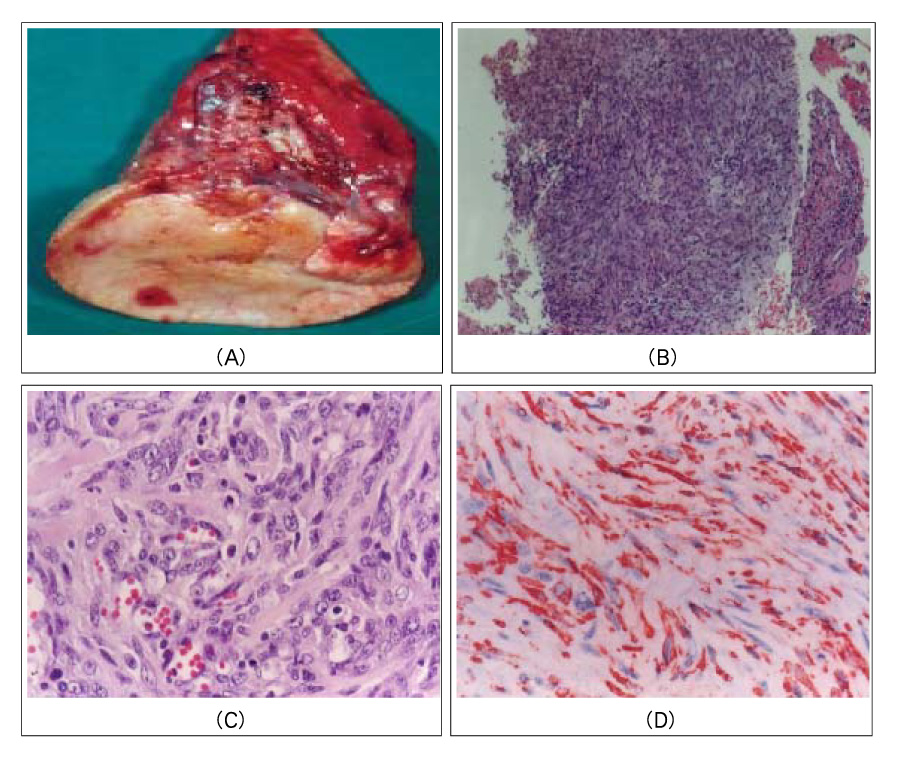
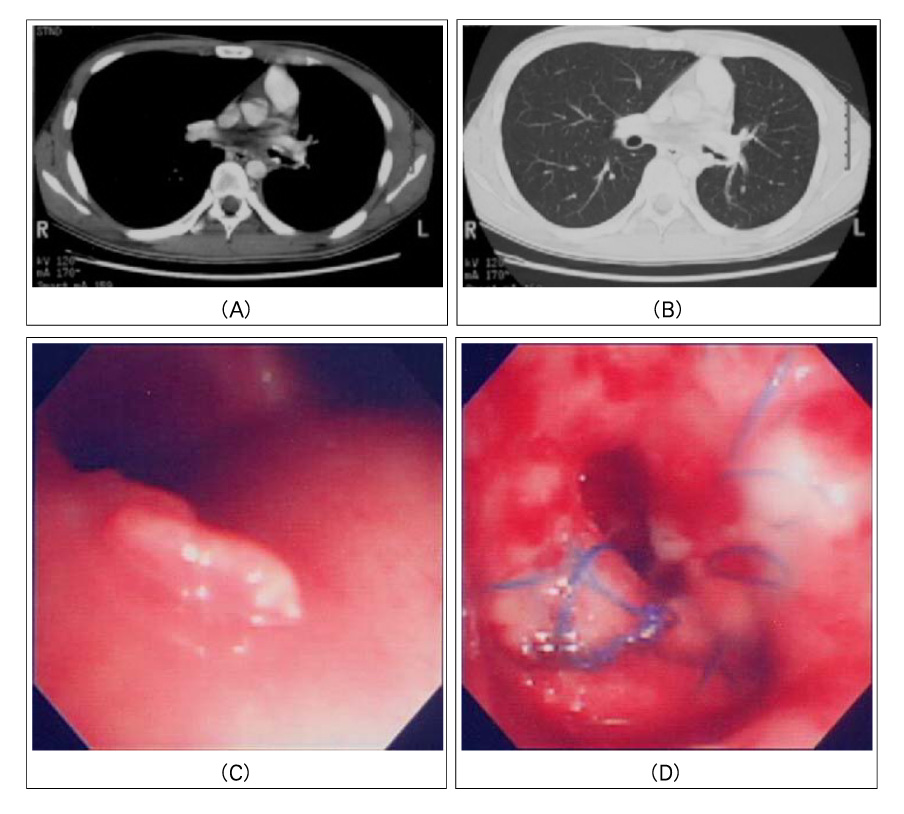
- A primary pulmonary leiomyosarcoma is a very rare pulmonary malignancy that arises from smooth muscle of either the bronchial or arterial walls. Common symptoms of the tumor are cough, dyspnea, chest pain and hemoptysis. The diagnosis of a primary pulmonary sarcoma can be established only after extensive clinical and radiologic examinations have failed to identify an alternative primary source. The only effective treatment for the tumor is a complete surgical resection when feasible. The type of resection is dictated by the local anatomic extent of the tumor. We report a case of a 21-year-old male with a primary endobronchial leiomyosarcoma who presented with massive hemoptysis. A necrotic ulcerative endobronchial lesion was observed in the orifice of left lower lobe bronchus on a bronchoscopic examination. He was treated with a complete sleeve resection of the left lower lobe. Three months later, local recurrence of the tumor was noticed on the follow up bronchoscopy and a then left pneumonectomy was then performed. Fifteen months later, the patient died from empyema with a bronchopleural fistula that was associated with tumor recurrence at the stump of the pneumonectomy.
MeSH Terms
Figure
Reference
-
1. Corpa-Rodriguez ME, Mayoralas-Alises S, Garcia-Sanchez J, Gil-Alonso JL, Diaz-Agero P, Casillas-Pajuelo M. Postoperative course in 7 cases of primary sarcoma of the lung. Arch Bronconeumol. 2005. 41:634–637.2. Odashiro AN, Miiji LO, Nguyen GK. Primary lung leiomyosarcoma detected by bronchoscopy cytology. Diagn Cytopathol. 2005. 33:220–222.3. Fitoz S, Atasoy C, Kizilkaya E, Basekim C, Karsli F. Radiologic findings in primary pulmonary leiomyosarcoma. J Thorac Imaging. 2000. 15:151–152.4. Etienne-Mastroianni B, Falchero L, Chalabreysse L, Loire R, Ranchere D, Souquet PJ, et al. Primary sarcomas of the lung: a clinicopathologic study of 12 cases. Lung Cancer. 2002. 38:283–289.5. Regnard JF, Icard P, Guibert L, de Montpreville VT, Magdeleinat P, Levasseur P. Prognostic factors and results after surgical treatment of primary sarcoma of the lung. Ann Thorac Surg. 1999. 68:227–231.6. Gladish GW, Sabloff BM, Munden RF, Truong MT, Erasmus JJ, Chasen MH. Primary thoracic sarcomas. Radiographics. 2002. 22:621–637.7. Conner WC, Fink GW, McGinnis KM, Alfieris GM. Surgical management of leiomyosarcoma of the mediastinum. Ann Thorac Surg. 2004. 77:334–336.8. Magne N, Porsin B, Pivot X, Tchiknavorian X, Marcy PY, Foa C, et al. Primary lung sarcoma: long survivors obtained with iterative complete surgery. Lung Cancer. 2001. 31:241–245.9. Porte HL, Metois DG, Leroy X, Conti M, Gosselin B, Wurtz A. Surgical treatment of primary sarcoma of the lung. Eur J Cardiothorac Surg. 2000. 18:136–142.10. Janssen JP, Mulder JJ, Wagenaar SS, Elbers HR, van den Bosch JM. Primary sarcoma of the lung: a clinical study with long-term follow-up. Ann Thorac Surg. 1994. 58:1151–1155.11. Takeda F, Yamagiwa I, Ohizumi H, Shiono S. Leiomyosarcoma of the main bronchus in a girl: a long-time survivor with multiple lung metastases. Pediatr Pulmonol. 2004. 37:368–374.12. Suster S. Primary sarcomas of the lung. Semin Diagn Pathol. 1995. 12:140–157.13. Moran CA, Suster S, Abbondanzo SL, Koss MN. Primary leiomyosarcomas of the lung: a clinicopathologic and immunohistochemical study of 18 cases. Mod Pathol. 1997. 10:121–128.14. Crum CP. Kumar V, Abbas AK, Fausto N, editors. Chapter 22. The female genital tract. Pathologic basis of disease. 2005. 7th ed. Philadelphia: W.B. Saunders;1059–1118.15. Rosai J. Rosai J, Ackerman LV, editors. Chapter 1. Introduction. Surgical pathology. 2004. 9th ed. New York: Mosby;9–12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adjuvant Treatment of Proper Endobronchial Management in Leiomyosarcoma
- Primary Endobronchial Leiomyosarcoma: One case report
- A Case of Primary Leiomyosarcoma of the Lung
- A Case of Radiation Bronchitis Induced Massive Hemoptysis after High-Dose-Rate Endobronchial Brachytherapy
- A Case of Complication of Expandible Metallic Stent with Endobronchial Stenosis