J Cerebrovasc Endovasc Neurosurg.
2014 Jun;16(2):71-77. 10.7461/jcen.2014.16.2.71.
Arachnoid Membrane Suturing for Prevention of Subdural Fluid Collection in Extracranial-intracranial Bypass Surgery
- Affiliations
-
- 1Department of Neurosurgery, Chonnam National University Hospital and Medical School, Gwangju, Korea. nsjsp@chonnam.ac.kr
- KMID: 1963173
- DOI: http://doi.org/10.7461/jcen.2014.16.2.71
Abstract
OBJECTIVE
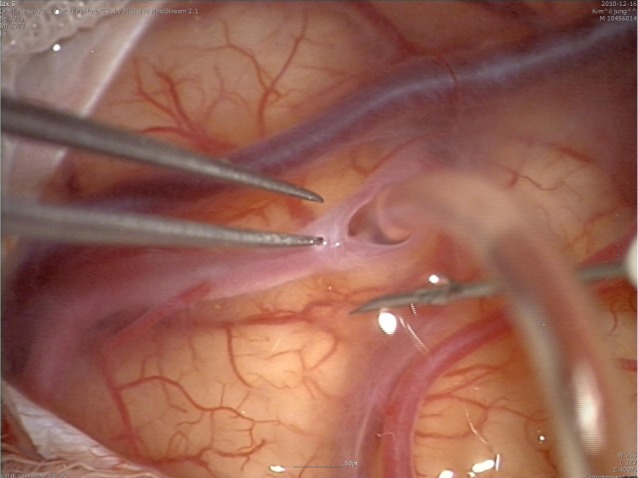
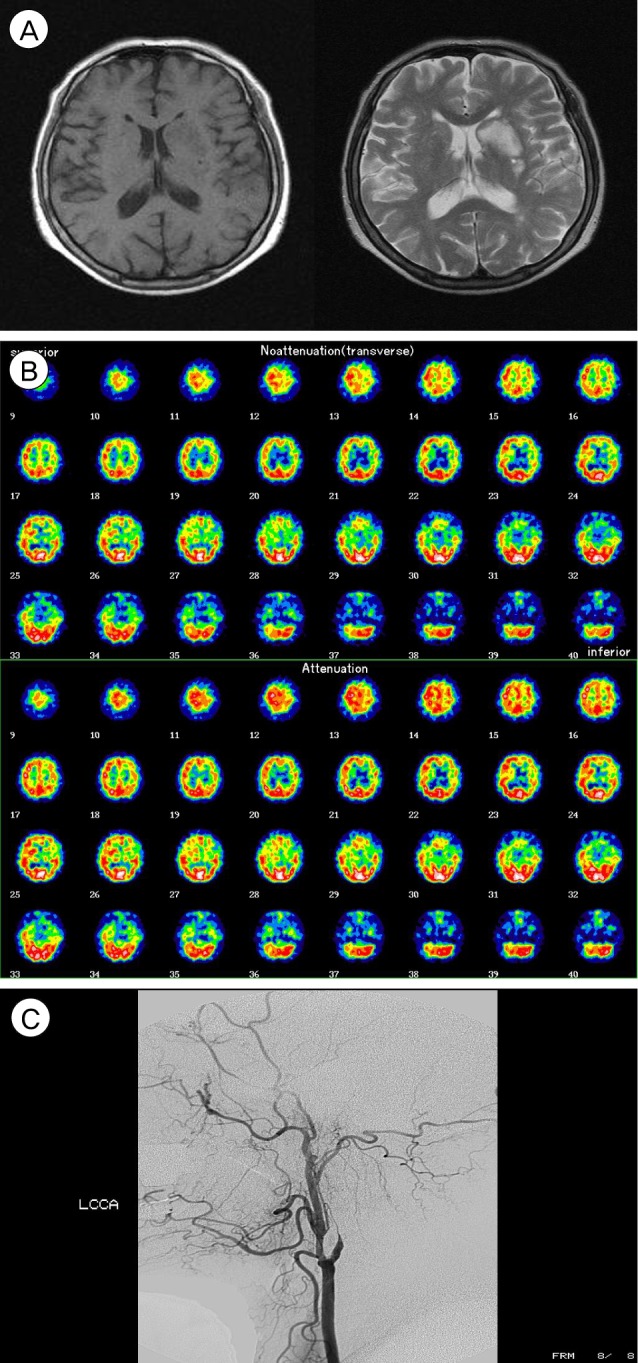
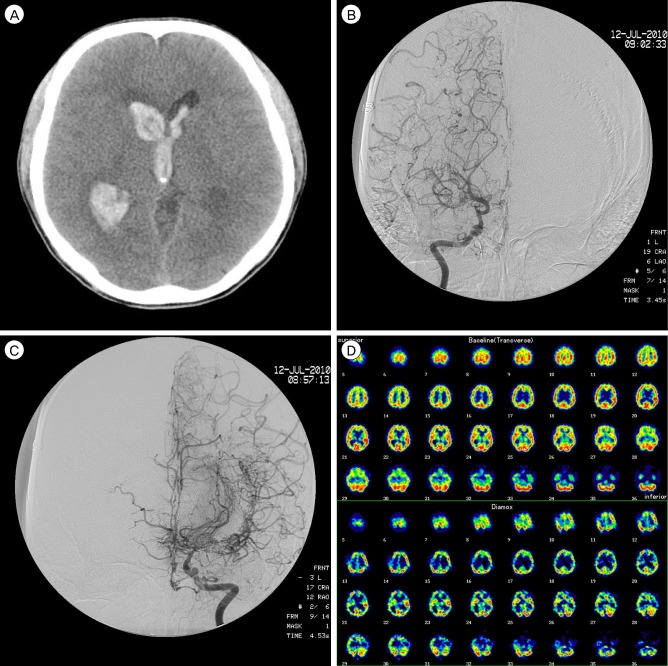
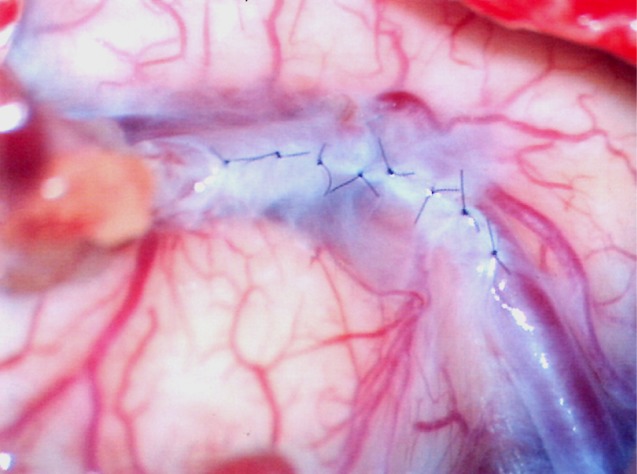
Water-tight closure of the dura in extracranial-intracranial (EC-IC) bypass is impossible because the superficial temporal artery (STA) must run through the dural defect. Consequently, subdural hygroma and subcutaneous cerebrospinal fluid (CSF) collection frequently occur postoperatively. To reduce these complications, we prospectively performed suturing of the arachnoid membrane after STA-middle cerebral artery (STA-MCA) and evaluated the clinical usefulness.
MATERIALS AND METHODS
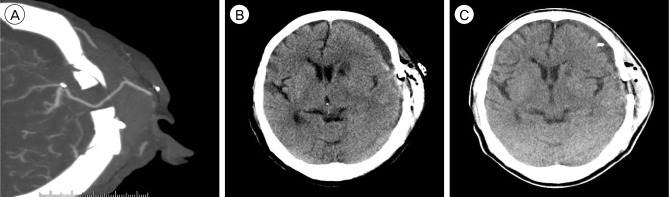
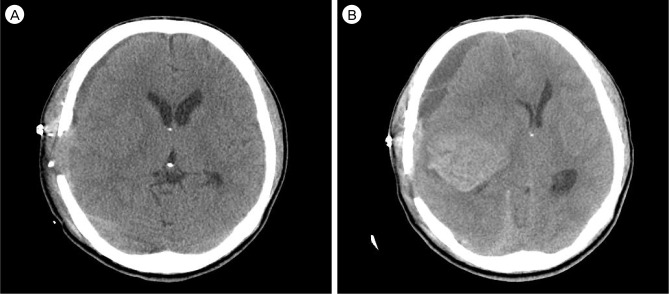
Between Mar. 2005 and Oct. 2010, extracranial-intracranial arterial bypass (EIAB) with/without encephalo-myo-synangiosis was performed in 88 cases (male : female = 53 : 35). As a control group, 51 patients (57 sides) underwent conventional bypass surgery without closure of the arachnoid membrane. Postoperative computed tomography (CT) scan was performed twice in three days and seven days later, respectively, for evaluation of the presence of subdural fluid collection and other mass lesions.
RESULTS
The surgical result was excellent, with no newly developing ischemic event until recent follow-up. The additional time needed for arachnoid suture was five to ten minutes, when three to eight sutures were required. Post-operative subdural fluid collection was not seen on follow-up computed tomography scans in all patients.
CONCLUSION
Arachnoid suturing is simple, safe, and effective for prevention of subdural fluid collection in EC-IC bypass surgery, especially the vulnerable ischemic hemisphere.
MeSH Terms
Figure
Reference
-
1. Andoh T, Sakai N, Yamada H, Yano H, Hirayama H, Imao Y, et al. Chronic subdural hematoma following bypass surgery-report of three cases. Neurol Med Chir (Tokyo). 1992; 8. 32(9):684–689. PMID: 1383857.2. Das K, Murali R, Lindstrom CJ, Couldwell WT. Symptomatic subdural hygroma and temporal lobe edema after translabyrinthine removal of acoustic neuroma. Skull Base. 2001; 5. 11(2):137–142. PMID: 17167613.
Article3. Fujimura M, Kaneta T, Shimizu H, Tominaga T. Cerebral ischemia owing to compression of the brain by swollen temporal muscle used for encephalo-myo-synangiosis in moyamoya disease. Neurosurg Rev. 2009; 4. 32(2):245–249. discussion 249. PMID: 19159959.
Article4. Furuya K, Kawahara N, Morita A, Momose T, Aoki S, Kirino T. Focal hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in a patient with moyamoya disease. Case report. J Neurosurg. 2004; 1. 100(1):128–132. PMID: 14743925.5. Kuroda S, Kamiyama H, Abe H, Asaoka K, Mitsumori K. Temporary neurological deterioration caused by hyperperfusion after extracranial-intracranial bypass-case report and study of cerebral hemodynamics. Neurol Med Chir (Tokyo). 1994; 1. 34(1):15–19. PMID: 7514747.6. Nakagawa Y, Shimoyama M, Kashiwaba T, Suzuki Y, Gotoh S, Miyasaka K, et al. [Reconstructive operation of Moyamoya disease and its problems]. No Shinkei Geka. 1981; 9(3):305–314. Japanese. PMID: 7242813.7. Ohue S, Kumon Y, Kohno K, Watanabe H, Iwata S, Ohnishi T. Postoperative temporary neurological deficits in adults with moyamoya disease. Surg Neurol. 2008; 3. 69(3):281–286. discussion 286-7. PMID: 17996267.
Article8. Sonobe M, Takahashi S, Kubota Y, Shirane R. [Chronic subdural hematoma developing after EMS for moyamoya disease]. No Shinkei Geka. 1982; 8. 10(8):857–859. Japanese. PMID: 7133306.9. Uno M, Nakajima N, Nishi K, Shinno K, Nagahiro S. Hyperperfusion syndrome after extracranial-intracranial bypass in a patient with moyamoya disease-case report. Neurol Med Chir (Tokyo). 1998; 7. 38(7):420–424. PMID: 9745249.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Intracranial Arachnoid Cyst
- Treatment of Chronic Subdural Hematoma with Arachnoid Cyst
- Two Cases of Arachnoid Cyst of the Middle Cranial Fossa with Chronic Subdural Hematoma
- A Clinical Analysis of 4 Cases of Arachnoid Cysts in Middle Cranial Fossa, Associated with Chronic Subdural Hematoma
- Clinical Observation of Intracrainal Arachnoid Cyst