J Korean Soc Radiol.
2015 Apr;72(4):291-294. 10.3348/jksr.2015.72.4.291.
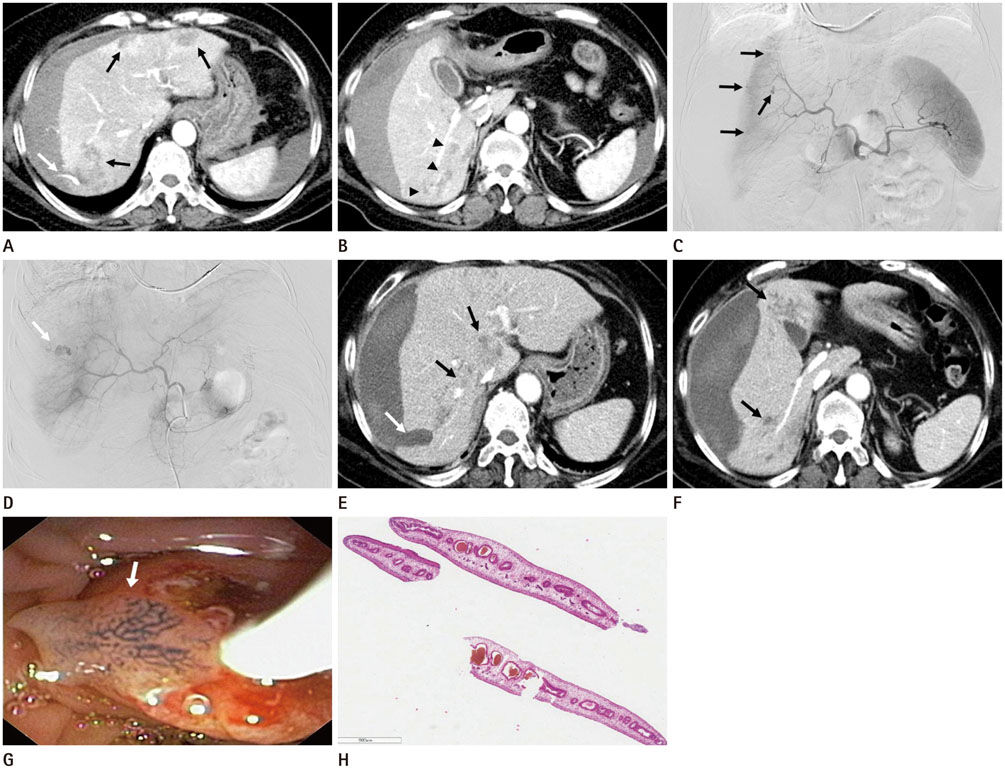
Hepatobiliary Fascioliasis with Multiple Aneurysms and Active Bleeding: A Case Report
- Affiliations
-
- 1Department of Radiology, College of Medicine, Yeungnam University, Daegu, Korea. sungho1999@ynu.ac.kr
- KMID: 1941761
- DOI: http://doi.org/10.3348/jksr.2015.72.4.291
Abstract
- A 52-year-old woman visited our institution with upper abdominal pain which had lasted for the past two days. Laboratory tests revealed mild leukocytosis, decreased serum hemoglobin, and peripheral blood eosinophilia. CT scans showed multiple ill-defined, hypodense lesions in the peripheral areas of both hepatic lobes and active bleeding with a subcapsular hematoma in the right hepatic lobe. Angiography also showed active bleeding in the right hepatic lobe with multiple aneurysms, so a transarterial coil embolization was performed to stop the bleeding. The endoscopic retrograde cholangiopancreatography revealed several moving flat flukes in the common bile duct, which were pathologically confirmed as Fasciola hepatica.
MeSH Terms
Figure
Reference
-
1. Mas-Coma S. Epidemiology of fascioliasis in human endemic areas. J Helminthol. 2005; 79:207–216.2. Song KD, Lim JH, Kim MJ, Jang YJ, Kim JW, Cho SH, et al. Peritoneal manifestations of fascioliasis on CT images: a new observation. Abdom Imaging. 2013; 38:839–843.3. Aksoy DY, Kerimoğlu U, Oto A, Ergüven S, Arslan S, Unal S, et al. Fasciola hepatica infection: clinical and computerized tomographic findings of ten patients. Turk J Gastroenterol. 2006; 17:40–45.4. Lim JH, Mairiang E, Ahn GH. Biliary parasitic diseases including clonorchiasis, opisthorchiasis and fascioliasis. Abdom Imaging. 2008; 33:157–165.5. Koç Z, Ulusan S, Tokmak N. Hepatobiliary fascioliasis: imaging characteristics with a new finding. Diagn Interv Radiol. 2009; 15:247–251.6. Catalano OA, Sahani DV, Forcione DG, Czermak B, Liu CH, Soricelli A, et al. Biliary infections: spectrum of imaging findings and management. Radiographics. 2009; 29:2059–2080.7. Kabaalioglu A, Ceken K, Alimoglu E, Saba R, Cubuk M, Arslan G, et al. Hepatobiliary fascioliasis: sonographic and CT findings in 87 patients during the initial phase and long-term follow-up. AJR Am J Roentgenol. 2007; 189:824–828.8. Marcos LA, Terashima A, Gotuzzo E. Update on hepatobiliary flukes: fascioliasis, opisthorchiasis and clonorchiasis. Curr Opin Infect Dis. 2008; 21:523–530.9. Lee WK, Mossop PJ, Little AF, Fitt GJ, Vrazas JI, Hoang JK, et al. Infected (mycotic) aneurysms: spectrum of imaging appearances and management. Radiographics. 2008; 28:1853–1868.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Hepatobiliary Fascioliasis with Multiple Aneurysms and Active Bleeding: A Case Report
- A Case of Fascioliasis Diagnosed by ERCP
- Multiple Aneurysms of the Distal Anterior Cerebral Artery: Case Report
- A Case of Liver Abscess Associated with Fascioliasis Diagnosed by MRI
- Endovascular Treatment of Multiple Pancreaticoduodenal Artery Aneurysms Associated with Celiac Artery Stenosis: A Case Report