J Korean Soc Radiol.
2015 Apr;72(4):271-281. 10.3348/jksr.2015.72.4.271.
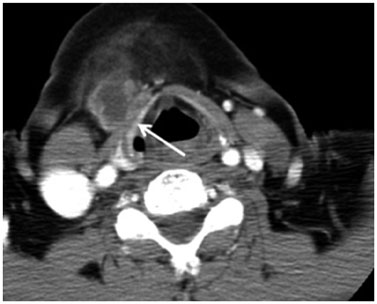
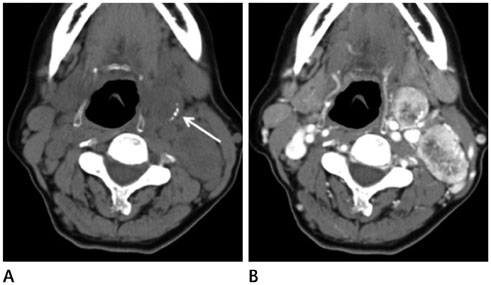
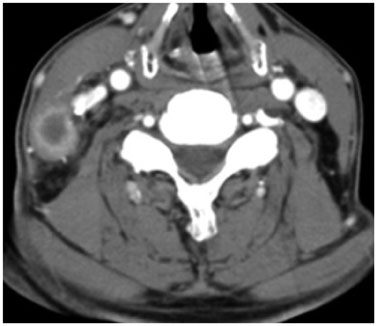
Comparative Study of Lymph Node Metastasis from Squamous Cell Carcinoma and Non-Squamous Cell Carcinoma on Neck CT
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. mdhjk@schmc.ac.kr
- KMID: 1941758
- DOI: http://doi.org/10.3348/jksr.2015.72.4.271
Abstract
- PURPOSE
To assess the differential imaging findings of metastatic lymph nodes in squamous cell carcinoma (SCC) and non-squamous cell carcinoma (non-SCC) on neck CT and to facilitate the identification of primary focus before performing a biopsy.
MATERIALS AND METHODS
We retrospectively analyzed 46 patients with SCC and 50 patients with non-SCC who underwent neck CT from January 2006 to January 2011. Patients were divided into two groups; SCC and non-SCC. The total number of lymph nodes was 204 in the SCC group and 530 in the non-SCC group. Two observers were asked to assess the characteristics of abnormal lymph nodes (number, margin types, enhancement patterns, size, bilaterality, calcification, fat infiltration, conglomeration, invasion of adjacent tissue, and nodal distribution). Nodal distribution was evaluated by imaging-based nodal classification on neck CT.
RESULTS
Between the SCC group and the non-SCC group except for cases of thyroid cancer, the number of lymph nodes and the number of lymph nodes smaller than 3 cm in the non-SCC group except for cases of thyroid cancer were significantly greater than those in the SCC group (p < 0.05).
CONCLUSION
The number of lymph nodes, the number of lymph nodes smaller than 3 cm, and nodal distribution are helpful in differential diagnosis between SCC and non-SCC before performing a biopsy.
MeSH Terms
Figure
Cited by 1 articles
-
Radiotherapy versus Surgery in Early-Stage HPV-Positive Oropharyngeal Cancer
Dong-Yun Kim, Hong-Gyun Wu, Jin Ho Kim, Joo Ho Lee, Soon-Hyun Ahn, Eun-Jae Chung, Keun-Yong Eom, Young Ho Jung, Woo-Jin Jeong, Tack-Kyun Kwon, Suzy Kim, Chan Woo Wee
Cancer Res Treat. 2022;54(2):406-416. doi: 10.4143/crt.2021.441.
Reference
-
1. Seethala RR. Current state of neck dissection in the United States. Head Neck Pathol. 2009; 3:238–245.2. van den Brekel MW, Stel HV, Castelijns JA, Nauta JJ, van der Waal I, Valk J, et al. Cervical lymph node metastasis: assessment of radiologic criteria. Radiology. 1990; 177:379–384.3. Sumi M, Ohki M, Nakamura T. Comparison of sonography and CT for differentiating benign from malignant cervical lymph nodes in patients with squamous cell carcinoma of the head and neck. AJR Am J Roentgenol. 2001; 176:1019–1024.4. de Bondt RB, Nelemans PJ, Bakers F, Casselman JW, Peutz-Kootstra C, Kremer B, et al. Morphological MRI criteria improve the detection of lymph node metastases in head and neck squamous cell carcinoma: multivariate logistic regression analysis of MRI features of cervical lymph nodes. Eur Radiol. 2009; 19:626–633.5. Dammann F, Horger M, Mueller-Berg M, Schlemmer H, Claussen CD, Hoffman J, et al. Rational diagnosis of squamous cell carcinoma of the head and neck region: comparative evaluation of CT, MRI, and 18FDG PET. AJR Am J Roentgenol. 2005; 184:1326–1331.6. Curtin HD, Ishwaran H, Mancuso AA, Dalley RW, Caudry DJ, McNeil BJ. Comparison of CT and MR imaging in staging of neck metastases. Radiology. 1998; 207:123–130.7. Yuasa K, Kawazu T, Nagata T, Kanda S, Ohishi M, Shirasuna K. Computed tomography and ultrasonography of metastatic cervical lymph nodes in oral squamous cell carcinoma. Dentomaxillofac Radiol. 2000; 29:238–244.8. Anzai Y, Brunberg JA, Lufkin RB. Imaging of nodal metastases in the head and neck. J Magn Reson Imaging. 1997; 7:774–783.9. Burgess KL, Hartwick RW, Bedard YC. Metastatic squamous carcinoma presenting as a neck cyst. Differential diagnosis from inflamed branchial cleft cyst in fine needle aspirates. Acta Cytol. 1993; 37:494–449.10. Verma K, Mandal S, Kapila K. Cystic change in lymph nodes with metastatic squamous cell carcinoma. Acta Cytol. 1995; 39:478–480.11. Flanagan PM, Roland NJ, Jones AS. Cervical node metastases presenting with features of branchial cysts. J Laryngol Otol. 1994; 108:1068–1071.12. Gourin CG, Johnson JT. Incidence of unsuspected metastases in lateral cervical cysts. Laryngoscope. 2000; 110(10 Pt 1):1637–1641.13. Unal M, Pata YS, AkbasXMLLink_XYZ Y, Aydin O. Cervical cystic metastasis of squamous cell carcinoma: a case report with an unusual presentation. Eur Arch Otorhinolaryngol. 2005; 262:387–389.14. Goldenberg D, Sciubba J, Koch WM. Cystic metastasis from head and neck squamous cell cancer: a distinct disease variant? Head Neck. 2006; 28:633–638.15. Goldenberg D, Begum S, Westra WH, Khan Z, Sciubba J, Pai SI, et al. Cystic lymph node metastasis in patients with head and neck cancer: an HPV-associated phenomenon. Head Neck. 2008; 30:898–903.16. Regauer S, Mannweiler S, Anderhuber W, Gotschuli A, Berghold A, Schachenreiter J, et al. Cystic lymph node metastases of squamous cell carcinoma of Waldeyer's ring origin. Br J Cancer. 1999; 79:1437–1442.17. Choi YJ, Yun JS, Kook SH, Jung EC, Park YL. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010; 34:1494–1499.18. Sohn YM, Kwak JY, Kim EK, Moon HJ, Kim SJ, Kim MJ. Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am J Roentgenol. 2010; 194:38–43.19. Rosário PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005; 24:1385–1389.20. Eisenkraft BL, Som PM. The spectrum of benign and malignant etiologies of cervical node calcification. AJR Am J Roentgenol. 1999; 172:1433–1437.21. Moon WK, Han MH, Chang KH, Im JG, Kim HJ, Sung KJ, et al. CT and MR imaging of head and neck tuberculosis. Radiographics. 1997; 17:391–402.22. Choi EC, Moon WJ, Lim YC. Case report. Tuberculous cervical lymphadenitis mimicking metastatic lymph nodes from papillary thyroid carcinoma. Br J Radiol. 2009; 82:e208–e211.23. Iqbal M, Subhan A, Aslam A. Papillary thyroid carcinoma with tuberculous cervical lymphadenopathy mimicking metastasis. J Coll Physicians Surg Pak. 2011; 21:207–209.24. Mancuso AA, Harnsberger HR, Muraki AS, Stevens MH. Computed tomography of cervical and retropharyngeal lymph nodes: normal anatomy, variants of normal, and applications in staging head and neck cancer. Part II: pathology. Radiology. 1983; 148:715–772.25. Yousem DM, Som PM, Hackney DB, Schwaibold F, Hendrix RA. Central nodal necrosis and extracapsular neoplastic spread in cervical lymph nodes: MR imaging versus CT. Radiology. 1992; 182:753–759.26. King AD, Tse GM, Ahuja AT, Yuen EH, Vlantis AC, To EW, et al. Necrosis in metastatic neck nodes: diagnostic accuracy of CT, MR imaging, and US. Radiology. 2004; 230:720–726.27. Trotta BM, Pease CS, Rasamny JJ, Raghavan P, Mukherjee S. Oral cavity and oropharyngeal squamous cell cancer: key imaging findings for staging and treatment planning. Radiographics. 2011; 31:339–354.28. Som PM. Detection of metastasis in cervical lymph nodes: CT and MR criteria and differential diagnosis. AJR Am J Roentgenol. 1992; 158:961–969.29. Mancuso AA, Maceri D, Rice D, Hanafee W. CT of cervical lymph node cancer. AJR Am J Roentgenol. 1981; 136:381–385.30. Vandecaveye V, De Keyzer F, Vander Poorten V, Dirix P, Verbeken E, Nuyts S, et al. Head and neck squamous cell carcinoma: value of diffusion-weighted MR imaging for nodal staging. Radiology. 2009; 251:134–146.31. Wunderbaldinger P, Harisinghani MG, Hahn PF, Daniels GH, Turetschek K, Simeone J, et al. Cystic lymph node metastases in papillary thyroid carcinoma. AJR Am J Roentgenol. 2002; 178:693–697.32. Yamashita H, Noguchi S, Murakami N, Kawamoto H, Watanabe S. Extracapsular invasion of lymph node metastasis is an indicator of distant metastasis and poor prognosis in patients with thyroid papillary carcinoma. Cancer. 1997; 80:2268–2272.33. Yamashita H, Noguchi S, Murakami N, Toda M, Uchino S, Watanabe S, et al. Extracapsular invasion of lymph node metastasis. A good indicator of disease recurrence and poor prognosis in patients with thyroid microcarcinoma. Cancer. 1999; 86:842–884.34. Parkin DM, Muir CS. Cancer Incidence in Five Continents. Comparability and quality of data. IARC Sci Publ. 1992; (120):45–173.35. Voutilainen PE, Multanen MM, Leppäniemi AK, Haglund CH, Haapiainen RK, Franssila KO. Prognosis after lymph node recurrence in papillary thyroid carcinoma depends on age. Thyroid. 2001; 11:953–957.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Squamous Cell Carcinoma of Sigmoid Colon
- A Case of Squamous Cell Carcinoma with Metastasis Developed in Acne Conglobata
- A Case of Squamous Cell Carcinoma of the Nail Bed with Lymph Node Metastasis
- CT findings of mediastinal lymph node metastasis in bronchogenic carcinoma of the lung: A comparative study of small cell carcinoma vs non-small cell carcinoma
- A Case of Squamous Cell Carcinoma of the Scrotum