J Korean Soc Transplant.
2014 Dec;28(4):226-235. 10.4285/jkstn.2014.28.4.226.
Pre-transplant Predictors for 3-Month Mortality after Living Donor Liver Transplantation
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jw.joh@samsung.com
- 2Division of Gastroenterology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1941318
- DOI: http://doi.org/10.4285/jkstn.2014.28.4.226
Abstract
- BACKGROUND
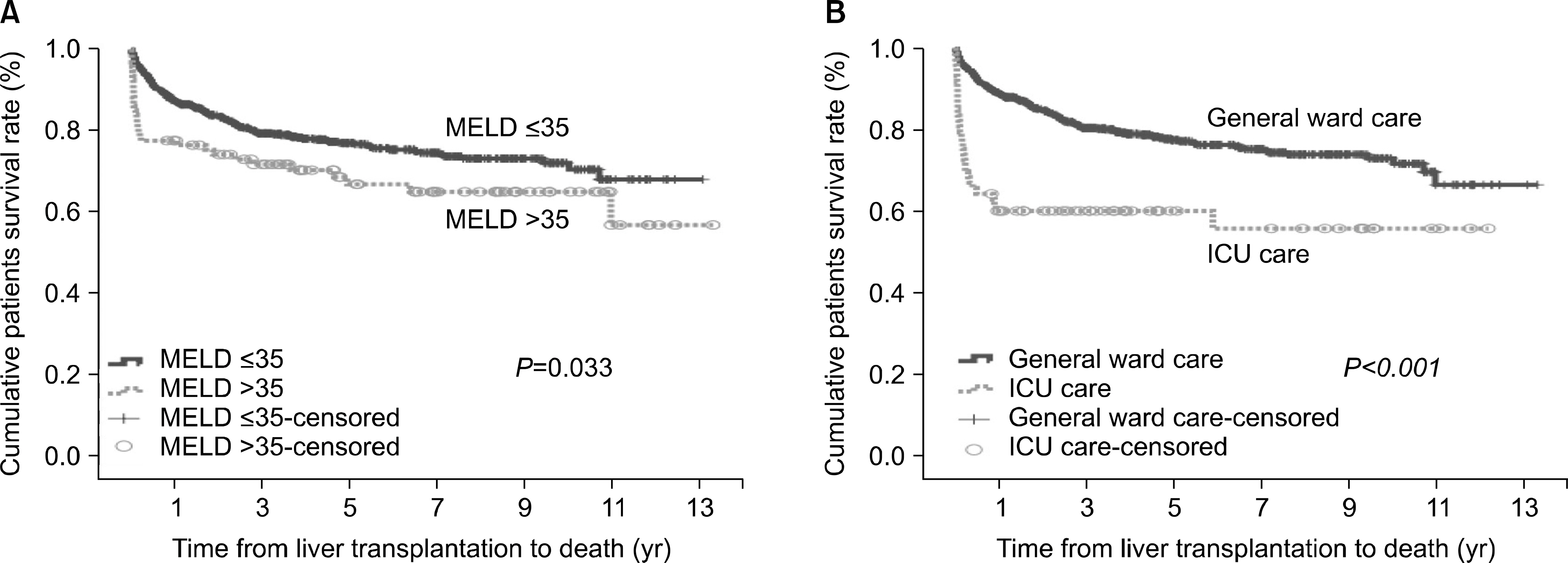
High model for end-stage liver disease (MELD) scores (> or =35) is closely associated with poor posttransplantation outcomes in patients who undergo living donor liver transplantation (LDLT). There is little information regarding factors that negatively impact the survival of patients with high MELD scores. The aim of this study was to identify factors associated with 3-month mortality of patients after LDLT.
METHODS
We retrospectively analyzed 774 patients who underwent adult LDLT with right lobe grafts between 1996 and 2012. Exclusion criteria were re-transplantation, left graft, auxiliary partial orthotopic liver transplantation, and inadequate medical recording. Preoperative variables were analyzed retrospectively.
RESULTS
The overall 3-month survival rate was 92%. In univariate analysis, acute progression of disease, severity of hepatic encephalopathy, Child-Pugh class C, hepatorenal syndrome, use of continuous renal replacement therapy, use of ventilator, intensive care unit (ICU) care before transplantation, and MELD scores > or =35 were identified as potential risk factors. However, only ICU care before transplantation and MELD scores > or =35 were independent risk factors for 3-month mortality after LDLT. Three-month and 1-year patient survival rates for those with no risk factors were 95.5% and 88.6%, respectively. In contrast, patients with at least one risk factor had 3-month and 1-year patient survival rates of 88.4% and 81.1%, respectively, while patients with two risk factors had 3-month and 1-year patient survival rates of 55.6% and 55.6%, respectively.
CONCLUSIONS
Patients with both risk factors (ICU care before LDLT and MELD scores > or =35) should be cautiously considered for treatment with LDLT.
Keyword
MeSH Terms
Figure
Reference
-
References
1). Korean Network for Organ Sharing (KONOS). Korean Network for Organ Sharing [Internet]. Seoul: KONOS;2014. [cited 2014 Jun 30]. Available from:. http://www.konos.go.kr/konosis/index.jsp.2). Ikegami T, Shirabe K, Yoshiya S, Yoshizumi T, Ninomiya M, Uchiyama H, et al. Bacterial sepsis after living donor liver transplantation: the impact of early enteral nutrition. J Am Coll Surg. 2012; 214:288–95.
Article3). Freise CE, Gillespie BW, Koffron AJ, Lok AS, Pruett TL, Emond JC, et al. Recipient morbidity after living and deceased donor liver transplantation: findings from the A2ALL Retrospective Cohort Study. Am J Transplant. 2008; 8:2569–79.
Article4). Li C, Mi K, Wen T, Yan L, Li B, Yang J, et al. Outcomes of patients with benign liver diseases undergoing living donor versus deceased donor liver transplantation. PLoS One. 2011; 6:e27366.
Article5). Bernardi M, Gitto S, Biselli M. The MELD score in patients awaiting liver transplant: strengths and weaknesses. J Hepatol. 2011; 54:1297–306.
Article6). Trotter JF, Osgood MJ. MELD scores of liver transplant recipients according to size of waiting list: impact of organ allocation and patient outcomes. JAMA. 2004; 291:1871–4.7). Onaca NN, Levy MF, Sanchez EQ, Chinnakotla S, Fasola CG, Thomas MJ, et al. A correlation between the pretransplantation MELD score and mortality in the first two years after liver transplantation. Liver Transpl. 2003; 9:117–23.
Article8). Selzner M, Kashfi A, Cattral MS, Selzner N, McGilvray ID, Greig PD, et al. Live donor liver transplantation in high MELD score recipients. Ann Surg. 2010; 251:153–7.
Article9). Li C, Wen T, Yan L, Li B, Wang W, Xu M, et al. Does model for end-stage liver disease score predict the short-term outcome of living donor liver transplantation? Transplant Proc. 2010; 42:3620–3.
Article10). Shin M, Song S, Kim JM, Kwon CH, Kim SJ, Lee SK, et al. Donor morbidity including biliary complications in living-donor liver transplantation: singlecenter analysis of 827 cases. Transplantation. 2012; 93:942–8.11). Moon JI, Kwon CH, Joh JW, Jung GO, Choi GS, Park JB, et al. Safety of small-for-size grafts in adult-to-adult living donor liver transplantation using the right lobe. Liver Transpl. 2010; 16:864–9.
Article12). Kim JM, Kim SJ, Joh JW, Kwon CH, Song S, Shin M, et al. Is cytomegalovirus infection dangerous in cytomegalovirus-seropositive recipients after liver transplantation? Liver Transpl. 2011; 17:446–55.
Article13). Foxton MR, Al-Freah MA, Portal AJ, Sizer E, Bernal W, Auzinger G, et al. Increased model for end-stage liver disease score at the time of liver transplant results in prolonged hospitalization and overall intensive care unit costs. Liver Transpl. 2010; 16:668–77.
Article14). New York State Department of Health. Information for a Healthy New York [Internet]. New York: New York State Department of Health;2014. [cited 2014 Jul 3]. Available from:. http://www.health.ny.gov.15). Hayashi PH, Trotter JF, Forman L, Kugelmas M, Steinberg T, Russ P, et al. Impact of pretransplant diagnosis of hepatocellular carcinoma on cadveric liver allocation in the era of MELD. Liver Transpl. 2004; 10:42–8.
Article16). Chok KS, Chan SC, Fung JY, Cheung TT, Chan AC, Fan ST, et al. Survival outcomes of right-lobe living donor liver transplantation for patients with high model for end-stage liver disease scores. Hepatobiliary Pancreat Dis Int. 2013; 12:256–62.
Article17). Ikegami T, Imai D, Wang H, Yoshizumi T, Yamashita Y, Ninomiya M, et al. D-MELD as a predictor of early graft mortality in adult-to-adult living-donor liver transplantation. Transplantation. 2014; 97:457–62.
Article18). Nadalin S, Schaffer R, Fruehauf N. Split-liver transplantation in the high-MELD adult patient: are we being too cautious? Transpl Int. 2009; 22:702–6.
Article19). Earl TM, Chari RS. Which types of graft to use in patients with acute liver failure? (A) Auxiliary liver transplant (B) Living donor liver transplantation (C) The whole liver. (C) I take the whole liver only. J Hepatol. 2007; 46:578–82.20). Barr ML, Belghiti J, Villamil FG, Pomfret EA, Sutherland DS, Gruessner RW, et al. A report of the Vancouver Forum on the care of the live organ donor: lung, liver, pancreas, and intestine data and medical guidelines. Transplantation. 2006; 81:1373–85.
Article21). Park I, Moon E, Hwang JA, Yu S, Kim BW, Wang HJ, et al. Does hepatorenal syndrome affect the result of liver transplantation? Clinical observations. Transplant Proc. 2010; 42:2563–6.
Article22). Nair S, Verma S, Thuluvath PJ. Pretransplant renal function predicts survival in patients undergoing orthotopic liver transplantation. Hepatology. 2002; 35:1179–85.
Article23). Emiroglu R, Yilmaz U, Coskun M, Karakayali H, Haberal M. Higher graft-to-host ratio may decrease posttransplant mortality in patients with a high MELD score. Transplant Proc. 2007; 39:1164–5. .S.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overcoming high pre-transplant isoagglutinin titers using high-dose intravenous immunoglobulin, salvage plasmapheresis, and booster rituximab without splenectomy in ABO-incompatible living donor liver transplantation: a case report
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Sluggish decline in a post-transplant model for end-stage liver disease score is a predictor of mortality in living donor liver transplantation
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making