Infect Chemother.
2011 Aug;43(4):355-358. 10.3947/ic.2011.43.4.355.
Clostridium tertium Bacteremia in a Non-neutropenic Patient with Small Bowel Obstruction
- Affiliations
-
- 1Department of Internal Medicine and AIDS Research Institute, Yonsei University College of Medicine, Seoul, Korea. shhan74@yuhs.ac
- 2Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1936073
- DOI: http://doi.org/10.3947/ic.2011.43.4.355
Abstract
- Clostridium tertium-induced bacteremia is a rare condition seen predominantly in neutropenic patients and/or patients with gastrointestinal disease. In this report, we describe a non-neutropenic, 72-year-old patient with a small bowel obstruction who presented with C. tertium bacteremia. Clostridium tertium is aerotolerant and resistant to broad-spectrum cephalosporins. The aerotolerant nature of C. tertium is resulted in delayed identification and reporting since it is not initially considered a candidate for infection.
MeSH Terms
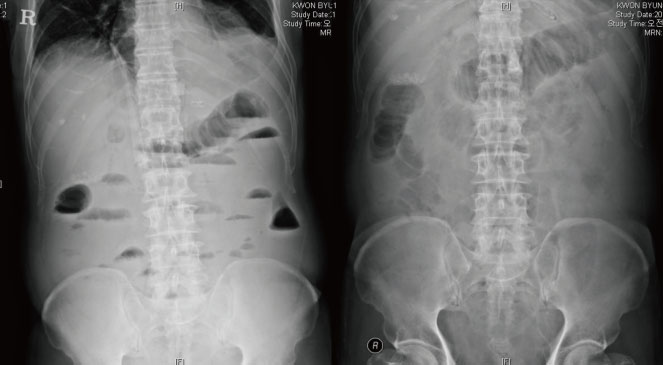
Figure
Reference
-
1. Allen SD, Emery CL, Lyerly DM. Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, editors. Clostridium. Manual of clinical microbiology. 2003. 8th ed. Washington, DC: ASM Press;835–856.2. King BM, Ranck BA, Daugherty FD, Rau CA. Clostridium tertium septicemia. N Engl J Med. 1963. 269:467–469.3. Miller DL, Brazer S, Murdoch D, Reller LB, Corey GR. Significance of Clostridium tertium bacteremia in neutropenic and nonneutropenic patients: review of 32 cases. Clin Infect Dis. 2001. 32:975–978.
Article4. Lew JF, Wiedermann BL, Sneed J, Campos J, McCullough D. Aerotolerant Clostridium tertium brain abscess following a lawn dart injury. J Clin Microbiol. 1990. 28:2127–2129.
Article5. Leegaard TM, Sandven P, Gaustad P. Clostridium tertium: 3 case reports. Scand J Infect Dis. 2005. 37:230–232.
Article6. Gosbell IB, Johnson CG, Newton PJ, Jelfs J. Clostridium tertium bacteremia: 2 cases and review. Pathology. 1996. 28:70–73.7. Steyaert S, Peleman R, Vaneechoutte M, De Baere T, Claeys G, Verschraegen G. Septicemia in neutropenic patients infected with Clostridium tertium resistant to cefepime and other expanded-spectrum cephalosporins. J Clin Microbiol. 1999. 37:3778–3779.
Article8. Thaler M, Gill V, Pizzo PA. Emergence of Clostridium tertium as a pathogen in neutropenic patients. Am J Med. 1986. 81:596–600.9. Coleman N, Speirs G, Khan J, Broadbent V, Wight DG, Warren RE. Neutropenic enterocolitis associated with Clostridium tertium. J Clin Pathol. 1993. 46:180–183.10. Valtonen M, Sivonen A, Elonen E. A cluster of seven cases of Clostridium tertium septicemia in neutropenic patients. Eur J Clin Microbiol Infect Dis. 1990. 9:40–42.
Article11. Speirs G, Warren RE, Rampling A. Clostridium tertium septicemia in patients with neutropenia. J Infect Dis. 1988. 158:1336–1340.12. Brown EA, Talbot GH, Provencher M, Cassileth P. Anaerobic bacteremia in patients with acute leukemia. Infect Control Hosp Epidemiol. 1989. 10:65–69.
Article13. Tappe D, Dirks J, Müller R, Brederlau J, Abele-Horn M, Suerbaum S, Kurzai O. Fatal Clostridium tertium septicemia in a nonneutropenic patient. J Infect. 2005. 50:76–80.14. Vanderhofstadt M, André M, Lonchay C, Levecque P, Holemans X, Canon JL, D'Hondt L. Clostridium tertium bactermia: contamination or true pathogen? A report two cases and a review of the literature. Int J Infect Dis. 2010. 14:Suppl 3. e335–e337.15. Goldstein EJ, Citron DM, Merriam CV, Warren YA, Tyrrell KL, Fernandez HT. Comparative in vitro susceptibilities of 396 unusual anaerobic strains to tigecycline and eight other antimicrobial agents. Antimicrob Agents Chemother. 2006. 50:3507–3513.
Article16. Fomin P, Koalov S, Cooper A, Babinchak T, Dartois N, De Vane N, Castaing N, Tellado J. 301 And 306 Study Groups. The efficacy and safety of tigecycline for the treatment of complicated intra-abdominal infections - the European experience. J Chemother. 2008. 20:Suppl 1. 12–19.
Article17. Babinchak T, Ellis-Grosse E, Dartois N, Rose GM, Loh E. Tigecycline 301 Study Group. Tigecycline 306 Study Group. The efficacy and safety of tigecycline for the treatment of complicated intra-abdominal infections: analysis of pooled clinical trial data. Clin Infect Dis. 2005. 41:Suppl 5. S354–S367.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Clostridium tertium Infection and Successful Identification of the Organism by Matrix-Assisted Laser Desorption-Ionization Time-of-Flight Mass Spectrometry Analysis
- Two Cases of Clostridium citroniae Bacteremia in Cancer Patients
- Two Cases of Bacteremias Caused by Clostridium ramosum
- Small bowel intubation using guide wire: use in decompression of small bowel obstruction
- A Case of Clostridium bifermentans Bacteremia in a Patient with Myelodysplastic Syndrome