Evidence-based Guidelines for Empirical Therapy of Neutropenic Fever in Korea
- Affiliations
-
- 1National Evidence-based Healthcare Collaborating Agency, Seoul, Korea. symonlee@catholic.ac.kr
- 2Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Infectious Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Family Medicine, Hallym University College of Medicine, Chuncheon, Korea.
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Laboratory Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 7Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 8Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 9Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1936068
- DOI: http://doi.org/10.3947/ic.2011.43.4.285
Abstract
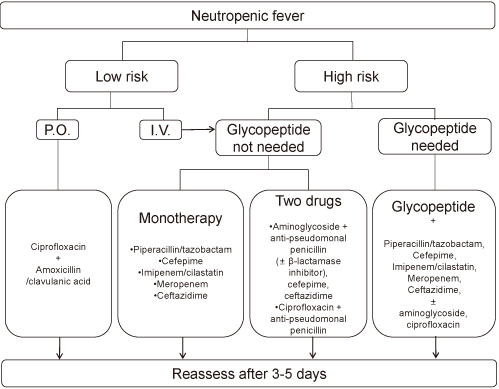
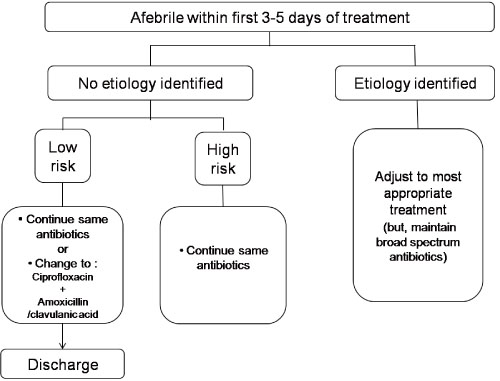
- Neutrophils play an important role in immunological function. Neutropenic patients are vulnerable to infection, and except fever is present, inflammatory reactions are scarce in many cases. Additionally, because infections can worsen rapidly, early evaluation and treatments are especially important in febrile neutropenic patients. In cases in which febrile neutropenia is anticipated due to anticancer chemotherapy, antibiotic prophylaxis can be used, based on the risk of infection. Antifungal prophylaxis may also be considered if long-term neutropenia or mucosal damage is expected. When fever is observed in patients suspected to have neutropenia, an adequate physical examination and blood and sputum cultures should be performed. Initial antibiotics should be chosen by considering the risk of complications following the infection; if the risk is low, oral antibiotics can be used. For initial intravenous antibiotics, monotherapy with a broad-spectrum antibiotic or combination therapy with two antibiotics is recommended. At 3 5 days after beginning the initial antibiotic therapy, the condition of the patient is assessed again to determine whether the fever has subsided or symptoms have worsened. If the patient's condition has improved, intravenous antibiotics can be replaced with oral antibiotics; if the condition has deteriorated, a change of antibiotics or addition of antifungal agents should be considered. If the causative microorganism is identified, initial antimicrobial or antifungal agents should be changed accordingly. When the cause is not detected, the initial agents should continue to be used until the neutrophil count recovers.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Fatal Breakthrough Mucormycosis in an Acute Myelogenous Leukemia Patient while on Posaconazole Prophylaxis
Seung Hun Kang, Hyun Seon Kim, Myoung Nam Bae, Jihye Kim, Ji Yeon Yoo, Kwan Yong Lee, Dong-Gun Lee, Hee-Je Kim
Infect Chemother. 2015;47(1):49-54. doi: 10.3947/ic.2015.47.1.49.Increase in Antibiotic-Resistant Gram-Negative Bacterial Infections in Febrile Neutropenic Children
Joon Hee Lee, Seul-Ki Kim, Seong Koo Kim, Seung Beom Han, Jae Wook Lee, Dong-Gun Lee, Nack-Gyun Chung, Bin Cho, Dae Chul Jeong, Jin Han Kang, Hack-Ki Kim
Infect Chemother. 2016;48(3):181-189. doi: 10.3947/ic.2016.48.3.181.Mycobacterium kansasii Pneumonia with Mediastinal Lymphadenitis in a Patient with Acute Myeloid Leukemia: Successful Treatment to Stem Cell Transplantation
Yeon-Geun Choi, Sung-Yeon Cho, Dong-Gun Lee, Eunjung Yim, Hyonsoo Joo, Seongyul Ryu, Jae-Ki Choi, Hee-Je Kim
Infect Chemother. 2017;49(1):78-83. doi: 10.3947/ic.2017.49.1.78.Principles of selecting appropriate antimicrobial agents
Su-Mi Choi, Dong-Gun Lee
J Korean Med Assoc. 2019;62(6):335-344. doi: 10.5124/jkma.2019.62.6.335.Advances in prophylaxis and treatment of invasive fungal infections: perspectives on hematologic diseases
Hyojin Ahn, Raeseok Lee, Sung-Yeon Cho, Dong-Gun Lee
Blood Res. 2022;57(S1):101-111. doi: 10.5045/br.2022.2022036.
Reference
-
1. The Korean Society of Infectious Diseases. Infectious Disease. 2007. Seoul: Koonja Publishing Inc.2. Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002. 34:730–751.
Article3. Segal BH, Baden LR, Casper C, Dubberke E, Freifeld AG, Gelfand M, Greene JN, Greer JP. NCCN Clinical Practice Guidelines in Oncology Prevention and Treatment of Cancer-Related Infections (v.2.2009). 2009. Fort Washington: National Comprehensive Cancer Network.4. Bertz H, Auner HW, Weissinger F, Salwender HJ, Einsele H, Egerer G, Sandherr M, Schuttrumpf S, Sudhoff T, Maschmeyer G. Antimicrobial therapy of febrile complications after high-dose chemo-/radiotherapy and autologous hematopoietic stem cell transplantation--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S167–S174.5. Bohme A, Ruhnke M, Buchheidt D, Cornely OA, Einsele H, Enzensberger R, Hebart H, Heinz W, Junghanss C, Karthaus M, Kruger W, Krug U, Kubin T, Penack O, Reichert D, Reuter S, Silling G, Sudhoff T, Ullmann AJ, Maschmeyer G. Treatment of invasive fungal infections in cancer patients--recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2009. 88:97–110.
Article6. Bohme A, Ruhnke M, Buchheidt D, Karthaus M, Einsele H, Guth S, Heussel G, Heussel CP, Junghanss C, Kern WK, Kubin T, Maschmeyer G, Sezer O, Silling G, Sudhoff T, Szelenyi Dagger H, Ullmann AJ. Treatment of fungal infections in hematology and oncology--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S133–S140.7. Buchheidt D, Bohme A, Cornely OA, Fatkenheuer G, Fuhr HG, Heussel G, Junghanss C, Karthaus M, Kellner O, Kern WV, Schiel X, Sezer O, Sudhoff T, Szelenyi H. Diagnosis and treatment of documented infections in neutropenic patients--recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S127–S132.8. Cornely OA, Bohme A, Buchheidt D, Glasmacher A, Kahl C, Karthaus M, Kern W, Kruger W, Maschmeyer G, Ritter J, Salwender HJ, Sandherr M, Schiel X, Schuttrumpf S, Sieniawski M, Silling G, Ullmann AJ, Wolf HH. Prophylaxis of invasive fungal infections in patients with hematological malignancies and solid tumors--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S186–S200.9. Einsele H, Bertz H, Beyer J, Kiehl MG, Runde V, Kolb HJ, Holler E, Beck R, Schwerdfeger R, Schumacher U, Hebart H, Martin H, Kienast J, Ullmann AJ, Maschmeyer G, Krüger W, Niederwieser D, Link H, Schmidt CA, Oettle H, Klingebiel T. Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Infectious complications after allogeneic stem cell transplantation:epidemiology and interventional therapy strategies--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S175–S185.10. Fatkenheuer G, Buchheidt D, Cornely OA, Fuhr HG, Karthaus M, Kisro J, Leithauser M, Salwender H, Sudhoff T, Szelenyi H, Weissinger F. Central venous catheter (CVC)-related infections in neutropenic patients--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S149–S157.11. Link H, Bohme A, Cornely OA, Hoffken K, Kellner O, Kern WV, Mahlberg R, Maschmeyer G, Nowrousian MR, Ostermann H, Ruhnke M, Sezer O, Schiel X, Wilhelm M, Auner HW. Antimicrobial therapy of unexplained fever in neutropenic patients--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO), Study Group Interventional Therapy of Unexplained Fever, Arbeitsgemeinschaft Supportivmassnahmen in der Onkologie (ASO) of the Deutsche Krebsgesellschaft (DKG-German Cancer Society). Ann Hematol. 2003. 82:Suppl 2. S105–S117.12. Ruhnke M, Bohme A, Buchheidt D, Donhuijsen K, Einsele H, Enzensberger R, Glasmacher A, Gumbel H, Heussel CP, Karthaus M, Lambrecht E, Sudhoff T, Szelenyi H. Diagnosis of invasive fungal infections in hematology and oncology--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003. 82:Suppl 2. S141–S148.13. Sandherr M, Einsele H, Hebart H, Kahl C, Kern W, Kiehl M, Massenkeil G, Penack O, Schiel X, Schuettrumpf S, Ullmann AJ, Cornely OA. Antiviral prophylaxis in patients with haematological malignancies and solid tumours: Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Oncology (DGHO). Ann Oncol. 2006. 17:1051–1059.
Article14. Marchetti O, Cordonnier C, Calandra T. Empirical antifungal therapy in neutropaenic cancer patients with persistent fever. Eur J Cancer Suppl. 2007. 5:32–42.
Article15. Maertens JA, Frere P, Lass-Florl C, Heinz W, Cornely OA. Primary antifungal prophylaxis in leukaemia patients. Eur J Cancer Suppl. 2007. 5:43–48.
Article16. Drgona L, Paul M, Bucaneve G, Calandra T, Menichetti F. The need for aminoglycosides in combination with β-lactams for high-risk, febrile neutropaenic patients with leukaemia. Eur J Cancer Suppl. 2007. 5:13–22.
Article17. Cometta A, Marchetti O, Calandra T. Empirical use of anti-Gram-positive antibiotics in febrile neutropaenic cancer patients with acute leukaemia. Eur J Cancer Suppl. 2007. 5:23–31.
Article18. Bucaneve G, Castagnola E, Viscoli C, Leibovici L, Menichetti F. Quinolone prophylaxis for bacterial infections in afebrile high risk neutropenic patients. Eur J Cancer Suppl. 2007. 5:5–12.
Article19. Jun HX, Zhixiang S, Chun W, Reksodiputro AH, Ranuhardy D, Tamura K, Matsumoto T, Lee DG, Purushotaman SV, Lim V, Ahmed A, Hussain Y, Chua M, Ong A, Liu CY, Hsueh PR, Lin SF, Liu YC, Suwangool P, Jootar S, Picazo JJ. Clinical guidelines for the management of cancer patients with neutropenia and unexplained fever. Int J Antimicrob Agents. 2005. 26:Suppl 2. S128–S132. discussion S133-40.
Article20. Yoshida M, Ohno R. Current antimicrobial usage for the management of infections in leukemic patients in Japan: results of a survey. Clin Infect Dis. 2004. 39:Suppl 1. S11–S14.
Article21. Yoshida M, Ohno R. Antimicrobial prophylaxis in febrile neutropenia. Clin Infect Dis. 2004. 39:Suppl 1. S65–S67.
Article22. Urabe A. Clinical features of the neutropenic host: definitions and initial evaluation. Clin Infect Dis. 2004. 39:Suppl 1. S53–S55.
Article23. Tamura K, Imajo K, Akiyama N, Suzuki K, Urabe A, Ohyashiki K, Tanimoto M, Masaoka T. Randomized trial of cefepime monotherapy or cefepime in combination with amikacin as empirical therapy for febrile neutropenia. Clin Infect Dis. 2004. 39:Suppl 1. S15–S24.
Article24. Tamura K. Initial empirical antimicrobial therapy: duration and subsequent modifications. Clin Infect Dis. 2004. 39:Suppl 1. S59–S64.
Article25. Ohyashiki K. Monotherapy versus dual therapy based on risk categorization of febrile neutropenic patients. Clin Infect Dis. 2004. 39:Suppl 1. S56–S58.
Article26. Masaoka T. Evidence-based recommendations for antimicrobial use in febrile neutropenia in Japan: executive summary. Clin Infect Dis. 2004. 39:Suppl 1. S49–S52.
Article27. Kanamaru A, Tatsumi Y. Microbiological data for patients with febrile neutropenia. Clin Infect Dis. 2004. 39:Suppl 1. S7–S10.
Article28. Canadian Task Force on the Periodic Health Examination. The periodic health examination. Can Med Assoc J. 1979. 121:1193–1254.29. Choi SM, Park SH, Lee DG, Choi JH, Yoo JH, Shin WS. Current antimicrobial usage for the management of neutropenic fever in Korea: a nationwide survey. J Korean Med Sci. 2008. 23:941–947.
Article30. Kim HS, Song MG. Comparison of rectal temperature and tympanic membrane. Nurs Sci. 1998. 10:22–30.31. Fulbrook P. Core body temperature measurement: a comparison of axilla, tympanic membrane and pulmonary artery blood temperature. Intensive Crit Care Nurs. 1997. 13:266–272.
Article32. Dzarr AA, Kamal M, Baba AA. A comparison between infrared tympanic thermometry, oral and axilla with rectal thermometry in neutropenic adults. Eur J Oncol Nurs. 2009. 13:250–254.
Article33. Ciuraru NB, Braunstein R, Sulkes A, Stemmer SM. The influence of mucositis on oral thermometry: when fever may not reflect infection. Clin Infect Dis. 2008. 46:1859–1863.
Article34. Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966. 64:328–340.
Article35. Bodey GP, Rodriguez V, Chang HY, Narboni . Fever and infection in leukemic patients: a study of 494 consecutive patients. Cancer. 1978. 41:1610–1622.
Article36. Sickles EA, Greene WH, Wiernik PH. Clinical presentation of infection in granulocytopenic patients. Arch Intern Med. 1975. 135:715–719.
Article37. Heussel CP, Kauczor HU, Heussel GE, Fischer B, Begrich M, Mildenberger P, Thelen M. Pneumonia in febrile neutropenic patients and in bone marrow and blood stem-cell transplant recipients: use of high-resolution computed tomography. J Clin Oncol. 1999. 17:796–805.
Article38. Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J. The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol. 2000. 18:3038–3051.
Article39. Talcott JA, Finberg R, Mayer RJ, Goldman L. The medical course of cancer patients with fever and neutropenia. Clinical identification of a low-risk subgroup at presentation. Arch Intern Med. 1988. 148:2561–2568.
Article40. Talcott JA, Siegel RD, Finberg R, Goldman L. Risk assessment in cancer patients with fever and neutropenia: a prospective, two-center validation of a prediction rule. J Clin Oncol. 1992. 10:316–322.
Article41. Talcott JA, Whalen A, Clark J, Rieker PP, Finberg R. Home antibiotic therapy for low-risk cancer patients with fever and neutropenia: a pilot study of 30 patients based on a validated prediction rule. J Clin Oncol. 1994. 12:107–114.
Article42. Jung JS, Kwon KY, Kim KS, Lim YS, Rhee JE, Suh GJ, Youn YK. Risk prediction factors in febrile neutropenic patients. J Korean Soc Emerg Med. 2000. 11:305–315.43. Yoo JH, Choi SM, Lee DG, Choi JH, Shin WS, Min WS, Kim CC. Prognostic factors influencing infection-related mortality in patients with acute leukemia in Korea. J Korean Med Sci. 2005. 20:31–35.
Article44. Gafter-Gvili A, Fraser A, Paul M, Leibovici L. Meta-analysis: antibiotic prophylaxis reduces mortality in neutropenic patients. Ann Intern Med. 2005. 142:979–995.
Article45. Engels EA, Lau J, Barza M. Efficacy of quinolone prophylaxis in neutropenic cancer patients: a meta-analysis. J Clin Oncol. 1998. 16:1179–1187.
Article46. Ito JI, Tegtmeier BR, O'Donnell MR. Antibacterial prophylaxis in patients with cancer and neutropenia. N Engl J Med. 2006. 354:90–94. author reply 90-4.
Article47. Cullen M, Steven N, Billingham L, Gaunt C, Hastings M, Simmonds P, Stuart N, Rea D, Bower M, Fernando I, Huddart R, Gollins S, Stanley A. Antibacterial prophylaxis after chemotherapy for solid tumors and lymphomas. N Engl J Med. 2005. 353:988–998.
Article48. Bucaneve G, Micozzi A, Menichetti F, Martino P, Dionisi MS, Martinelli G, Allione B, D'Antonio D, Buelli M, Nosari AM, Cilloni D, Zuffa E, Cantaffa R, Specchia G, Amadori S, Fabbiano F, Deliliers GL, Lauria F, Foa R, Del Favero A. Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. N Engl J Med. 2005. 353:977–987.
Article49. Lee DG, Choi SM, Choi JH, Yoo JH, Park YH, Kim YJ, Lee S, Min CK, Kim HJ, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Selective bowel decontamination for the prevention of infection in acute myelogenous leukemia: a prospective randomized trial. Korean J Intern Med. 2002. 17:38–44.
Article50. Thomas X, Troncy J, Belhabri A, Thiebaut A, Bouheddou N, Michallet M, Fleurette J, Pivot C, Fiere D, Archimbaud E. Effectiveness of combined vancomycin and pefloxacine in gastrointestinal decontamination for preventing infections after chemotherapy-induced bone marrow aplasia. A randomized double-blind study. Presse Med. 2000. 29:1745–1751.51. Talbot GH, Cassileth PA, Paradiso L, Correa-Coronas R, Bond L. The Enoxacin Prophylaxis Study Group. Oral enoxacin for infection prevention in adults with acute nonlymphocytic leukemia. Antimicrob Agents Chemother. 1993. 37:474–482.
Article52. Lew MA, Kehoe K, Ritz J, Antman KH, Nadler L, Takvorian T, Mayer R, Kalish L, Finberg R. Prophylaxis of bacterial infections with ciprofloxacin in patients undergoing bone marrow transplantation. Transplantation. 1991. 51:630–636.
Article53. Karp JE, Merz WG, Hendricksen C, Laughon B, Redden T, Bamberger BJ, Bartlett JG, Saral R, Burke PJ. Oral norfloxacin for prevention of gram-negative bacterial infections in patients with acute leukemia and granulocytopenia. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1987. 106:1–7.
Article54. Robenshtok E, Gafter-Gvili A, Goldberg E, Weinberger M, Yeshurun M, Leibovici L, Paul M. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2007. 25:5471–5489.
Article55. Goodman JL, Winston DJ, Greenfield RA, Chandrasekar PH, Fox B, Kaizer H, Shadduck RK, Shea TC, Stiff P, Friedman DJ, Powderly WG, Silber JL, Horowitz H, Lichtin A, Wolff SN, Mangan KF, Silver SM, Weisdorf D, Ho WG, Gilbert G, Buell D. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992. 326:845–851.
Article56. Slavin MA, Osborne B, Adams R, Levenstein MJ, Schoch HG, Feldman AR, Meyers JD, Bowden RA. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation--a prospective, randomized, double-blind study. J Infect Dis. 1995. 171:1545–1552.
Article57. Rotstein C, Bow EJ, Laverdiere M, Ioannou S, Carr D, Moghaddam N. The Canadian Fluconazole Prophylaxis Study Group. Randomized placebo-controlled trial of fluconazole prophylaxis for neutropenic cancer patients: benefit based on purpose and intensity of cytotoxic therapy. Clin Infect Dis. 1999. 28:331–340.
Article58. Winston DJ, Chandrasekar PH, Lazarus HM, Goodman JL, Silber JL, Horowitz H, Shadduck RK, Rosenfeld CS, Ho WG, Islam MZ, Buell DN. Fluconazole prophylaxis of fungal infections in patients with acute leukemia. Results of a randomized placebo-controlled, double-blind, multicenter trial. Ann Intern Med. 1993. 118:495–503.
Article59. Schaffner A, Schaffner M. Effect of prophylactic fluconazole on the frequency of fungal infections, amphotericin B use, and health care costs in patients undergoing intensive chemotherapy for hematologic neoplasias. J Infect Dis. 1995. 172:1035–1041.
Article60. Young GA, Bosly A, Gibbs DL, Durrant S. Antifungal Prophylaxis Study Group. A double-blind comparison of fluconazole and nystatin in the prevention of candidiasis in patients with leukaemia. Eur J Cancer. 1999. 35:1208–1213.
Article61. Philpott-Howard JN, Wade JJ, Mufti GJ, Brammer KW, Ehninger G. Multicentre Study Group. Randomized comparison of oral fluconazole versus oral polyenes for the prevention of fungal infection in patients at risk of neutropenia. J Antimicrob Chemother. 1993. 31:973–984.
Article62. Menichetti F, Del Favero A, Martino P, Bucaneve G, Micozzi A, D'Antonio D, Ricci P, Carotenuto M, Liso V, Nosari AM, Barbui T, Fasola G, Mandelli F. Preventing fungal infection in neutropenic patients with acute leukemia: fluconazole compared with oral amphotericin B. Ann Intern Med. 1994. 120:913–918.
Article63. Annaloro C, Oriana A, Tagliaferri E, Bertolli V, Della Volpe A, Soligo D, Ibatici A, Pozzoli E, Lambertenghi Deliliers GL. Efficacy of different prophylactic antifungal regimens in bone marrow transplantation. Haematologica. 1995. 80:512–517.64. Huijgens PC, Simoons-Smit AM, van Loenen AC, Prooy E, van Tinteren H, Ossenkoppele GJ, Jonkhoff AR. Fluconazole versus itraconazole for the prevention of fungal infections in haemato-oncology. J Clin Pathol. 1999. 52:376–380.
Article65. Glasmacher A, Cornely O, Ullmann AJ, Wedding U, Bodenstein H, Wandt H, Boewer C, Pasold R, Wolf HH, Hanel M, Dolken G, Junghanss C, Andreesen R, Bertz H. An open-label randomized trial comparing itraconazole oral solution with fluconazole oral solution for primary prophylaxis of fungal infections in patients with haematological malignancy and profound neutropenia. J Antimicrob Chemother. 2006. 57:317–325.
Article66. Marr KA, Crippa F, Leisenring W, Hoyle M, Boeckh M, Balajee SA, Nichols WG, Musher B, Corey L. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood. 2004. 103:1527–1533.
Article67. Morgenstern GR, Prentice AG, Prentice HG, Ropner JE, Schey SA, Warnock DW. U.K. Multicentre Antifungal Prophylaxis Study Group. A randomized controlled trial of itraconazole versus fluconazole for the prevention of fungal infections in patients with haematological malignancies. Br J Haematol. 1999. 105:901–911.
Article68. Oren I, Rowe JM, Sprecher H, Tamir A, Benyamini N, Akria L, Gorelik A, Dally N, Zuckerman T, Haddad N, Fineman R, Dann EJ. A prospective randomized trial of itraconazole vs fluconazole for the prevention of fungal infections in patients with acute leukemia and hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2006. 38:127–134.
Article69. Winston DJ, Maziarz RT, Chandrasekar PH, Lazarus HM, Goldman M, Blumer JL, Leitz GJ, Territo MC. Intravenous and oral itraconazole versus intravenous and oral fluconazole for long-term antifungal prophylaxis in allogeneic hematopoietic stem-cell transplant recipients. A multicenter, randomized trial. Ann Intern Med. 2003. 138:705–713.
Article70. Slordal L, Spigset O. Heart failure induced by non-cardiac drugs. Drug Saf. 2006. 29:567–586.
Article71. Nagappan V, Deresinski S. Reviews of anti-infective agents: posaconazole: a broad-spectrum triazole antifungal agent. Clin Infect Dis. 2007. 45:1610–1617.72. Schering-Plough announces FDA approval of NOXAFIL(R) (posaconazole) for treatment of oropharyngeal candidiasis (OPC). Schering-Plough. Accessed 15 May 2011. Available at: http://www2.prnewswire.com/cgi-bin/stories.pl?ACCT=104&STORY=/www/story/10-23-2006/0004456852&EDATE=.73. Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, Helfgott D, Holowiecki J, Stockelberg D, Goh YT, Petrini M, Hardalo C, Suresh R, Angulo-Gonzalez D. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007. 356:348–359.
Article74. van Burik JA, Ratanatharathorn V, Stepan DE, Miller CB, Lipton JH, Vesole DH, Bunin N, Wall DA, Hiemenz JW, Satoi Y, Lee JM, Walsh TJ. Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis. 2004. 39:1407–1416.
Article75. Hiramatsu Y, Maeda Y, Fujii N, Saito T, Nawa Y, Hara M, Yano T, Asakura S, Sunami K, Tabayashi T, Miyata A, Matsuoka K, Shinagawa K, Ikeda K, Matsuo K, Tanimoto M. Use of micafungin versus fluconazole for antifungal prophylaxis in neutropenic patients receiving hematopoietic stem cell transplantation. Int J Hematol. 2008. 88:588–595.
Article76. Wolff SN, Fay J, Stevens D, Herzig RH, Pohlman B, Bolwell B, Lynch J, Ericson S, Freytes CO, LeMaistre F, Collins R, Pineiro L, Greer J, Stein R, Goodman SA, Dummer S. Fluconazole vs low-dose amphotericin B for the prevention of fungal infections in patients undergoing bone marrow transplantation: a study of the North American Marrow Transplant Group. Bone Marrow Transplant. 2000. 25:853–859.
Article77. Bodey GP, Anaissie EJ, Elting LS, Estey E, O'Brien S, Kantarjian H. Antifungal prophylaxis during remission induction therapy for acute leukemia fluconazole versus intravenous amphotericin B. Cancer. 1994. 73:2099–2106.
Article78. Tollemar J, Ringden O, Andersson S, Sundberg B, Ljungman P, Tyden G. Randomized double-blind study of liposomal amphotericin B (Ambisome) prophylaxis of invasive fungal infections in bone marrow transplant recipients. Bone Marrow Transplant. 1993. 12:577–582.79. Kelsey SM, Goldman JM, McCann S, Newland AC, Scarffe JH, Oppenheim BA, Mufti GJ. Liposomal amphotericin (AmBisome) in the prophylaxis of fungal infections in neutropenic patients: a randomised, double-blind, placebo-controlled study. Bone Marrow Transplant. 1999. 23:163–168.
Article80. Tollemar J, Hockerstedt K, Ericzon BG, Sundberg B, Ringden O. Fungal prophylaxis with AmBisome in liver and bone marrow transplant recipients: results of two randomized double-blind studies. Transplant Proc. 1994. 26:1833.81. Penack O, Schwartz S, Martus P, Reinwald M, Schmidt-Hieber M, Thiel E, Blau IW. Low-dose liposomal amphotericin B in the prevention of invasive fungal infections in patients with prolonged neutropenia: results from a randomized, single-center trial. Ann Oncol. 2006. 17:1306–1312.
Article82. Schwartz S, Behre G, Heinemann V, Wandt H, Schilling E, Arning M, Trittin A, Kern WV, Boenisch O, Bosse D, Lenz K, Ludwig WD, Hiddemann W, Siegert W, Beyer J. Aerosolized amphotericin B inhalations as prophylaxis of invasive aspergillus infections during prolonged neutropenia: results of a prospective randomized multicenter trial. Blood. 1999. 93:3654–3661.83. Alexander BD, Dodds Ashley ES, Addison RM, Alspaugh JA, Chao NJ, Perfect JR. Non-comparative evaluation of the safety of aerosolized amphotericin B lipid complex in patients undergoing allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2006. 8:13–20.
Article84. Rijnders BJ, Cornelissen JJ, Slobbe L, Becker MJ, Doorduijn JK, Hop WC, Ruijgrok EJ, Lowenberg B, Vulto A, Lugtenburg PJ, de Marie S. Aerosolized liposomal amphotericin B for the prevention of invasive pulmonary aspergillosis during prolonged neutropenia: a randomized, placebo-controlled trial. Clin Infect Dis. 2008. 46:1401–1408.
Article85. Choi SM, Lee DG, Choi JH, Park SH, Eom KS, Kim YJ, Kim HJ, Min CK, Yoo JH, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Itraconazole oral solution versus fluconazole syrup for prevention of invasive fungal infections in patients receiving hematopoietic stem cell transplantation: prospective, randomized, comparative clinical trial. Infect Chemother. 2005. 37:71–78.86. Menichetti F, Del Favero A, Martino P, Bucaneve G, Micozzi A, Girmenia C, Barbabietola G, Pagano L, Leoni P, Specchia G, Caiozzo A, Raimondi R, Mandelli F. Gruppo Italiano Malattie Ematologiche dell' Adulto. Itraconazole oral solution as prophylaxis for fungal infections in neutropenic patients with hematologic malignancies: a randomized, placebo-controlled, double-blind, multicenter trial. GIMEMA Infection Program. Clin Infect Dis. 1999. 28:250–255.
Article87. Nucci M, Biasoli I, Akiti T, Silveira F, Solza C, Barreiros G, Spector N, Derossi A, Pulcheri W. A double-blind, randomized, placebo-controlled trial of itraconazole capsules as antifungal prophylaxis for neutropenic patients. Clin Infect Dis. 2000. 30:300–305.
Article88. Akiyama H, Mori S, Tanikawa S, Sakamaki H, Onozawa Y. Fluconazole versus oral amphotericin B in preventing fungal infection in chemotherapy-induced neutropenic patients with haematological malignancies. Mycoses. 1993. 36:373–378.
Article89. Riley DK, Pavia AT, Beatty PG, Petersen FB, Spruance JL, Stokes R, Evans TG. The prophylactic use of low-dose amphotericin B in bone marrow transplant patients. Am J Med. 1994. 97:509–514.
Article90. Kaptan K, Ural AU, Cetin T, Avcu F, Beyan C, Yalcin A. Itraconazole is not effective for the prophylaxis of fungal infections in patients with neutropenia. J Infect Chemother. 2003. 9:40–45.
Article91. Kern W, Behre G, Rudolf T, Kerkhoff A, Grote-Metke A, Eimermacher H, Kubica U, Wormann B, Buchner T, Hiddemann W. German AML Cooperative Group. Failure of fluconazole prophylaxis to reduce mortality or the requirement of systemic amphotericin B therapy during treatment for refractory acute myeloid leukemia: results of a prospective randomized phase III study. Cancer. 1998. 83:291–301.
Article92. Lass-Florl C, Gunsilius E, Gastl G, Englisch M, Koch G, Ulmer H, Dierich MP, Petzer A. Fungal colonization in neutropenic patients: a randomized study comparing itraconazole solution and amphotericin B solution. Ann Hematol. 2003. 82:565–569.
Article93. Van Delden C, Lew DP, Chapuis B, Rohner P, Hirschel B. Antifungal Prophylaxis in Severely Neutropenic Patients: How Much Fluconazole is Necessary? Clin Microbiol Infect. 1995. 1:24–30.
Article94. Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, Greinix H, Morais de Azevedo W, Reddy V, Boparai N, Pedicone L, Patino H, Durrant S. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007. 356:335–347.
Article95. Hughes WT, Rivera GK, Schell MJ, Thornton D, Lott L. Successful intermittent chemoprophylaxis for Pneumocystis carinii pneumonitis. N Engl J Med. 1987. 316:1627–1632.
Article96. Green H, Paul M, Vidal L, Leibovici L. Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: systematic review and meta-analysis of randomized controlled trials. Mayo Clin Proc. 2007. 82:1052–1059.
Article97. Green H, Paul M, Vidal L, Leibovici L. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. Cochrane Database Syst Rev. 2007. CD005590.
Article98. Wadhwa PD, Morrison VA. Infectious complications of chronic lymphocytic leukemia. Semin Oncol. 2006. 33:240–249.
Article99. Martin SI, Marty FM, Fiumara K, Treon SP, Gribben JG, Baden LR. Infectious complications associated with alemtuzumab use for lymphoproliferative disorders. Clin Infect Dis. 2006. 43:16–24.
Article100. Sudhoff T, Arning M, Schneider W. Prophylactic strategies to meet infectious complications in fludarabine-treated CLL. Leukemia. 1997. 11:Suppl 2. S38–S41.101. El-Sadr WM, Luskin-Hawk R, Yurik TM, Walker J, Abrams D, John SL, Sherer R, Crane L, Labriola A, Caras S, Pulling C, Hafner R. A randomized trial of daily and thrice-weekly trimethoprim-sulfamethoxazole for the prevention of Pneumocystis carinii pneumonia in human immunodeficiency virus-infected persons. Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA). Clin Infect Dis. 1999. 29:775–783.
Article102. Vasconcelles MJ, Bernardo MV, King C, Weller EA, Antin JH. Aerosolized pentamidine as pneumocystis prophylaxis after bone marrow transplantation is inferior to other regimens and is associated with decreased survival and an increased risk of other infections. Biol Blood Marrow Transplant. 2000. 6:35–43.
Article103. Souza JP, Boeckh M, Gooley TA, Flowers ME, Crawford SW. High rates of Pneumocystis carinii pneumonia in allogeneic blood and marrow transplant recipients receiving dapsone prophylaxis. Clin Infect Dis. 1999. 29:1467–1471.
Article104. Meyers JD, Flournoy N, Thomas ED. Infection with herpes simplex virus and cell-mediated immunity after marrow transplant. J Infect Dis. 1980. 142:338–346.
Article105. Schubert MM, Peterson DE, Flournoy N, Meyers JD, Truelove EL. Oral and pharyngeal herpes simplex virus infection after allogeneic bone marrow transplantation: analysis of factors associated with infection. Oral Surg Oral Med Oral Pathol. 1990. 70:286–293.
Article106. Barton T, Collis T, Stadtmauer E, Schuster M. Infectious complications the year after autologous bone marrow transplantation or peripheral stem cell transplantation for treatment of breast cancer. Clin Infect Dis. 2001. 32:391–395.
Article107. Herrmann RP, Trent M, Cooney J, Cannell PK. Infections in patients managed at home during autologous stem cell transplantation for lymphoma and multiple myeloma. Bone Marrow Transplant. 1999. 24:1213–1217.
Article108. Seropian S, Nadkarni R, Jillella AP, Salloum E, Burtness B, Hu GL, Zelterman D, Cooper DL. Neutropenic infections in 100 patients with non-Hodgkin's lymphoma or Hodgkin's disease treated with high-dose BEAM chemotherapy and peripheral blood progenitor cell transplant: out-patient treatment is a viable option. Bone Marrow Transplant. 1999. 23:599–605.
Article109. Lee JT, Kim YT. Prevalence of antibody to herpes simplex virus. Korean J Dermatol. 1993. 31:38–46.110. Glenny AM, Fernandez Mauleffinch LM, Pavitt S, Walsh T. Interventions for the prevention and treatment of herpes simplex virus in patients being treated for cancer. Cochrane Database Syst Rev. 2009. CD006706.
Article111. Yahav D, Gafter-Gvili A, Muchtar E, Skalsky K, Kariv G, Yeshurun M, Leibovici L, Paul M. Antiviral prophylaxis in haematological patients: systematic review and meta-analysis. Eur J Cancer. 2009. 45:3131–3148.
Article112. Liesveld JL, Abboud CN, Ifthikharuddin JJ, Lancet JE, Wedow LA, Oliva J, Stamm CG, Nichols D. Oral valacyclovir versus intravenous acyclovir in preventing herpes simplex virus infections in autologous stem cell transplant recipients. Biol Blood Marrow Transplant. 2002. 8:662–665.
Article113. Warkentin DI, Epstein JB, Campbell LM, Yip JG, Cox VC, Ransier A, Barnett MJ, Marra F. Valacyclovir versus acyclovir for HSV prophylaxisin neutropenic patients. Ann Pharmacother. 2002. 36:1525–1531.
Article114. Wade JC, Newton B, Flournoy N, Meyers JD. Oral acyclovir for prevention of herpes simplex virus reactivation after marrow transplantation. Ann Intern Med. 1984. 100:823–828.
Article115. Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, Wingard JR, Young JA, Boeckh MJ. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Preface. Bone Marrow Transplant. 2009. 44:453–455.
Article116. Choi SM, Lee DG, Park YH, Kim YJ, Kim HJ, Lee S, Choi JH, Yoo JH, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Infections in patients with acute leukemia : comparison of induction chemotherapy croup and reinduction chemotherapy group. Infect Chemother. 2003. 35:78–85.117. Kim HB, Park SW, Kim US, Kim JW, Shin DH, Oh M, Park S, Kim BK, Choe KW. Infections in patients with acute leukemia (1993-1996). Korean J Hematol. 1999. 34:359–365.118. Park SH, Choi SM, Lee DG, Choi JH, Yoo JH, Lee JW, Min WS, Shin WS, Kim CC. Current trends of infectious complications following hematopoietic stem cell transplantation in a single center. J Korean Med Sci. 2006. 21:199–207.
Article119. Rho YH, Lee YJ, Lee J, Eom JS, Sohn JW, Choi CW, Cheoung HJ, Kim WJ, Kim MJ, Kim JS, Park SC. Clinical aspects and prognostic factors of neutropenic fever in leukemic patients: 1996-2001. Korean J Infect Dis. 2002. 34:152–159.120. Rhee JY, Jang EH, Kim ST, Wi YM, Son KM, Cheong HS, Ki HK, Oh WS, Ki Hyun, Jung CW, Kim WS, Park K, Peck KR, Song JH. Profiles of infectious complications on the outcomes for the recipients of allogeneic hematopoietic stem cell transplantation. Korean J Med. 2007. 72:200–208.121. Kim JS, Oh JM. The patterns of infection and therapy in cancer patients receiving chemotherapy. J Korean Soc Health Syst Pharm. 2000. 17:481–500.122. Freifeld A, Marchigiani D, Walsh T, Chanock S, Lewis L, Hiemenz J, Hiemenz S, Hicks JE, Gill V, Steinberg SM, Pizzo PA. A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med. 1999. 341:305–311.
Article123. Hidalgo M, Hornedo J, Lumbreras C, Trigo JM, Colomer R, Perea S, Gomez C, Ruiz A, Garcia-Carbonero R, Cortes-Funes H. Outpatient therapy with oral ofloxacin for patients with low risk neutropenia and fever: a prospective, randomized clinical trial. Cancer. 1999. 85:213–219.
Article124. Kern WV, Cometta A, De Bock R, Langenaeken J, Paesmans M, Gaya H. International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. Oral versus intravenous empirical antimicrobial therapy for fever in patients with granulocytopenia who are receiving cancer chemotherapy. N Engl J Med. 1999. 341:312–318.
Article125. Malik IA, Khan WA, Karim M, Aziz Z, Khan MA. Feasibility of outpatient management of fever in cancer patients with low-risk neutropenia: results of a prospective randomized trial. Am J Med. 1995. 98:224–231.
Article126. Rolston KV, Rubenstein EB, Freifeld A. Early empiric antibiotic therapy for febrile neutropenia patients at low risk. Infect Dis Clin North Am. 1996. 10:223–237.
Article127. Rolston KV, Frisbee-Hume SE, Patel S, Manzullo EF, Benjamin RS. Oral moxifloxacin for outpatient treatment of low-risk, febrile neutropenic patients. Support Care Cancer. 2009.
Article128. Aquino VM, Herrera L, Sandler ES, Buchanan GR. Feasibility of oral ciprofloxacin for the outpatient management of febrile neutropenia in selected children with cancer. Cancer. 2000. 88:1710–1714.
Article129. Giamarellou H, Bassaris HP, Petrikkos G, Busch W, Voulgarelis M, Antoniadou A, Grouzi E, Zoumbos N. Monotherapy with intravenous followed by oral high-dose ciprofloxacin versus combination therapy with ceftazidime plus amikacin as initial empiric therapy for granulocytopenic patients with fever. Antimicrob Agents Chemother. 2000. 44:3264–3271.
Article130. Kerr KG, Armitage HT, McWhinney PH. Activity of quinolones against viridans group streptococci isolated from blood cultures of patients with haematological malignancy. Support Care Cancer. 1999. 7:28–30.
Article131. De Pauw BE, Deresinski SC, Feld R, Lane-Allman EF, Donnelly JP. The Intercontinental Antimicrobial Study Group. Ceftazidime compared with piperacillin and tobramycin for the empiric treatment of fever in neutropenic patients with cancer. A multicenter randomized trial. Ann Intern Med. 1994. 120:834–844.
Article132. Cometta A, Calandra T, Gaya H, Zinner SH, de Bock R, Del Favero A, Bucaneve G, Crokaert F, Kern WV, Klastersky J, Langenaeken I, Micozzi A, Padmos A, Paesmans M, Viscoli C, Glauser MP. The International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer and the Gruppo Italiano Malattie Ematologiche Maligne dell'Adulto Infection Program. Monotherapy with meropenem versus combination therapy with ceftazidime plus amikacin as empiric therapy for fever in granulocytopenic patients with cancer. Antimicrob Agents Chemother. 1996. 40:1108–1115.
Article133. Rubinstein E, Lode H, Grassi C. Antibiotic Study Group. Ceftazidime monotherapy vs ceftriaxone/tobramycin for serious hospital-acquired gram-negative infections. Clin Infect Dis. 1995. 20:1217–1228.
Article134. Winston DJ, Ho WG, Bruckner DA, Champlin RE. Beta-lactam antibiotic therapy in febrile granulocytopenic patients. A randomized trial comparing cefoperazone plus piperacillin, ceftazidime plus piperacillin, and imipenem alone. Ann Intern Med. 1991. 115:849–859.
Article135. Pizzo PA, Hathorn JW, Hiemenz J, Browne M, Commers J, Cotton D, Gress J, Longo D, Marshall D, McKnight J, et al. A randomized trial comparing ceftazidime alone with combination antibiotic therapy in cancer patients with fever and neutropenia. N Engl J Med. 1986. 315:552–558.
Article136. Behre G, Link H, Maschmeyer G, Meyer P, Paaz U, Wilhelm M, Hiddemann W. Meropenem monotherapy versus combination therapy with ceftazidime and amikacin for empirical treatment of febrile neutropenic patients. Ann Hematol. 1998. 76:73–80.
Article137. Bohme A, Shah PM, Stille W, Hoelzer D. Piperacillin/tazobactam versus cefepime as initial empirical antimicrobial therapy in febrile neutropenic patients: a prospective randomized pilot study. Eur J Med Res. 1998. 3:324–330.138. Del Favero A, Menichetti F, Martino P, Bucaneve G, Micozzi A, Gentile G, Furno P, Russo D, D'Antonio D, Ricci P, Martino B, Mandelli F. A multicenter, double-blind, placebo-controlled trial comparing piperacillin-tazobactam with and without amikacin as empiric therapy for febrile neutropenia. Clin Infect Dis. 2001. 33:1295–1301.
Article139. Akova M, Akan H, Korten V, Biberoglu K, Hayran M, Unal S, Kars A, Kansu E. Meropenem Study Group of Turkey. Comparison of meropenem with amikacin plus ceftazidime in the empirical treatment of febrile neutropenia: a prospective randomised multicentre trial in patients without previous prophylactic antibiotics. Int J Antimicrob Agents. 1999. 13:15–19.
Article140. Yamamura D, Gucalp R, Carlisle P, Cimino M, Roberts J, Rotstein C. Open randomized study of cefepime versus piperacillin-gentamicin for treatment of febrile neutropenic cancer patients. Antimicrob Agents Chemother. 1997. 41:1704–1708.
Article141. Freifeld AG, Walsh T, Marshall D, Gress J, Steinberg SM, Hathorn J, Rubin M, Jarosinski P, Gill V, Young RC, et al. Monotherapy for fever and neutropenia in cancer patients: a randomized comparison of ceftazidime versus imipenem. J Clin Oncol. 1995. 13:165–176.
Article142. Bow EJ, Rotstein C, Noskin GA, Laverdiere M, Schwarer AP, Segal BH, Seymour JF, Szer J, Sanche S. A randomized, open-label, multicenter comparative study of the efficacy and safety of piperacillin-tazobactam and cefepime for the empirical treatment of febrile neutropenic episodes in patients with hematologic malignancies. Clin Infect Dis. 2006. 43:447–459.
Article143. Johnson MP, Ramphal R. Beta-lactam-resistant Enterobacter bacteremia in febrile neutropenic patients receiving monotherapy. J Infect Dis. 1990. 162:981–983.
Article144. Feld R, DePauw B, Berman S, Keating A, Ho W. Meropenem versus ceftazidime in the treatment of cancer patients with febrile neutropenia: a randomized, double-blind trial. J Clin Oncol. 2000. 18:3690–3698.
Article145. Vandercam B, Gerain J, Humblet Y, Ferrant A, Wauters G, Moreau M, Longueville J, Symann M, Straetmans N. Meropenem versus ceftazidime as empirical monotherapy for febrile neutropenic cancer patients. Ann Hematol. 2000. 79:152–157.
Article146. Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ. Cancer management: a multidisciplinary approach. 2009. 12th ed. New York: CMP Medica.147. Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007. 7:338–348.
Article148. Paul M, Yahav D, Fraser A, Leibovici L. Empirical antibiotic monotherapy for febrile neutropenia: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2006. 57:176–189.
Article149. Jung HW, Chae JW, Kang MR, Yang JC, Moon CS, Ki HK, Chang HH, Oh WS, Kim K, Peck KR, Lee NY, Song JH. Comparative efficacy and safety of cefepime alone versus ceftazidime plus tobramycin in cancer patients with febrile neutropenia. Infect Chemother. 2004. 36:341–349.150. Lee DH, Kim CK, Ko JY, Ma JR, Lee GY, Chon SY, Kim BS, Noh YH. A comparative study of cefepime versus ceftazidime monotherapy as empirical therapy for febrile episodes in neutropenic patients. J Korean Soc Chemother. 2002. 20:243–251.151. Flaherty JP, Waitley D, Edlin B, George D, Arnow P, O'Keefe P, Weinstein RA. Multicenter, randomized trial of ciprofloxacin plus azlocillin versus ceftazidime plus amikacin for empiric treatment of febrile neutropenic patients. Am J Med. 1989. 87:278S–282S.152. Cometta A, Zinner S, de Bock R, Calandra T, Gaya H, Klastersky J, Langenaeken J, Paesmans M, Viscoli C, Glauser MP. The International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. Piperacillin-tazobactam plus amikacin versus ceftazidime plus amikacin as empiric therapy for fever in granulocytopenic patients with cancer. Antimicrob Agents Chemother. 1995. 39:445–452.
Article153. Cordonnier C, Herbrecht R, Pico JL, Gardembas M, Delmer A, Delain M, Moreau P, Ladeb S, Nalet V, Rollin C, Gres JJ. The French Cefepime Study Group. Cefepime/amikacin versus ceftazidime/amikacin as empirical therapy for febrile episodes in neutropenic patients: a comparative study. Clin Infect Dis. 1997. 24:41–51.
Article154. Peacock JE, Herrington DA, Wade JC, Lazarus HM, Reed MD, Sinclair JW, Haverstock DC, Kowalsky SF, Hurd DD, Cushing DA, Harman CP, Donowitz GR. Ciprofloxacin plus piperacillin compared with tobramycin plus piperacillin as empirical therapy in febrile neutropenic patients. A randomized, double-blind trial. Ann Intern Med. 2002. 137:77–87.
Article155. Sanz MA, Lopez J, Lahuerta JJ, Rovira M, Batlle M, Perez C, Vazquez L, Julia A, Palau J, Gutierrez M, Capote FJ, Ramos F, Benlloch L, Larrea L, Jarque I. Cefepime plus amikacin versus piperacillin-tazobactam plus amikacin for initial antibiotic therapy in haematology patients with febrile neutropenia: results of an open, randomized, multicentre trial. J Antimicrob Chemother. 2002. 50:79–88.
Article156. Rybak MJ, Abate BJ, Kang SL, Ruffing MJ, Lerner SA, Drusano GL. Prospective evaluation of the effect of an aminoglycoside dosing regimen on rates of observed nephrotoxicity and ototoxicity. Antimicrob Agents Chemother. 1999. 43:1549–1555.
Article157. Torfoss D, Hoiby EA, Tangen JM, Holte H, Bo K, Meyer P, Grottum K, Weyde K, Lauritzsen GF, Sandstad B, Jacobsen AB, Olsen H, Kvaloy S. Tobramycin once versus three times daily, given with penicillin G, to febrile neutropenic cancer patients in Norway: a prospective, randomized, multicentre trial. J Antimicrob Chemother. 2007. 59:711–717.
Article158. Choi SM, Lee DG, Kim MJ, Kim DY, Park YH, Kim YJ, Kim HJ, Lee S, Choi JH, Yoo JH, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Clinical features and risk factors of the septic shock in patients with neutropenic fever. Infect Chemother. 2003. 35:370–376.159. Elting LS, Rubenstein EB, Rolston K, Cantor SB, Martin CG, Kurtin D, Rodriguez S, Lam T, Kanesan K, Bodey G. Time to clinical response: an outcome of antibiotic therapy of febrile neutropenia with implications for quality and cost of care. J Clin Oncol. 2000. 18:3699–3706.
Article160. Kim WS, Lee H, Ki HK, Kim CK, Kim SW, Kim S, Peck KR, Kim WS, Youn SS, Lee HK, Kang WK, Park CH, Park KC, Song JH. The efficacy and safety of oral ciprofloxacin therapy for low-risk febrite patients with neutropenia during cancer chemotherapy. J Korean Soc Chemother. 2000. 18:29–38.161. European Organization for Research and Treatment of Cancer (EORTC) International Antimicrobial Therapy Cooperative Group and the National Cancer Institute of Canada-Clinical Trials Group. Vancomycin added to empirical combination antibiotic therapy for fever in granulocytopenic cancer patients. J Infect Dis. 1991. 163:951–958.162. Micozzi A, Venditti M, Amadori S, Pulsoni A, Tirindelli C, Martino P. Teicoplanin in the treatment of gram-positive bacteraemia in neutropenic patients. Br J Haematol. 1990. 76:Suppl 2. 19–23.
Article163. Vardakas KZ, Samonis G, Chrysanthopoulou SA, Bliziotis IA, Falagas ME. Role of glycopeptides as part of initial empirical treatment of febrile neutropenic patients: a meta-analysis of randomised controlled trials. Lancet Infect Dis. 2005. 5:431–439.
Article164. Paul M, Borok S, Fraser A, Vidal L, Leibovici L. Empirical antibiotics against Gram-positive infections for febrile neutropenia: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2005. 55:436–444.
Article165. Elting LS, Rubenstein EB, Rolston KV, Bodey GP. Outcomes of bacteremia in patients with cancer and neutropenia: observations from two decades of epidemiological and clinical trials. Clin Infect Dis. 1997. 25:247–259.
Article166. Glasmacher A, von Lilienfeld-Toal M, Schulte S, Hahn C, Schmidt-Wolf IG, Prentice A. An evidence-based evaluation of important aspects of empirical antibiotic therapy in febrile neutropenic patients. Clin Microbiol Infect. 2005. 11:Suppl 5. 17–23.
Article167. Kim SH, Park WB, Lee KD, Kang CI, Bang JW, Kim HB, Kim EC, Oh MD, Choe KW. Outcome of inappropriate initial antimicrobial treatment in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2004. 54:489–497.
Article168. Uh Y, Hwang GY, Jang IH, Kwon O, Kim HY, Yoon KJ. Antimicrobial susceptibility patterns and macrolide resistance genes of beta-hemolytic viridans group streptococci in a tertiary Korean hospital. J Korean Med Sci. 2007. 22:791–794.
Article169. Uh Y, Hwang GY, Jang IH, Yoon KJ, Kim HY. Antimicrobial susceptibilities of viridans streptococci isolated from blood cultures during recent period. J Lab Med Qual Assur. 2002. 24:225–230.170. Cometta A, Kern WV, De Bock R, Paesmans M, Vandenbergh M, Crokaert F, Engelhard D, Marchetti O, Akan H, Skoutelis A, Korten V, Vandercam M, Gaya H, Padmos A, Klastersky J, Zinner S, Glauser MP, Calandra T, Viscoli C. Vancomycin versus placebo for treating persistent fever in patients with neutropenic cancer receiving piperacillin-tazobactam monotherapy. Clin Infect Dis. 2003. 37:382–389.
Article171. Erjavec Z, de Vries-Hospers HG, Laseur M, Halie RM, Daenen S. A prospective, randomized, double-blinded, placebo-controlled trial of empirical teicoplanin in febrile neutropenia with persistent fever after imipenem monotherapy. J Antimicrob Chemother. 2000. 45:843–849.
Article172. Svetitsky S, Leibovici L, Paul M. Comparative efficacy and safety of vancomycin versus teicoplanin: systematic review and meta-analysis. Antimicrob Agents Chemother. 2009. 53:4069–4079.
Article173. Soriano A, Marco F, Martinez JA, Pisos E, Almela M, Dimova VP, Alamo D, Ortega M, Lopez J, Mensa J. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008. 46:193–200.
Article174. Brink AJ, Richards GA, Cummins RR, Lambson J. Recommendations to achieve rapid therapeutic teicoplanin plasma concentrations in adult hospitalised patients treated for sepsis. Int J Antimicrob Agents. 2008. 32:455–458.
Article175. Press OW, Ramsey PG, Larson EB, Fefer A, Hickman RO. Hickman catheter infections in patients with malignancies. Medicine (Baltimore). 1984. 63:189–200.
Article176. Cercenado E, Ena J, Rodriguez-Creixems M, Romero I, Bouza E. A conservative procedure for the diagnosis of catheter-related infections. Arch Intern Med. 1990. 150:1417–1420.
Article177. Blot F, Nitenberg G, Chachaty E, Raynard B, Germann N, Antoun S, Laplanche A, Brun-Buisson C, Tancrede C. Diagnosis of catheter-related bacteraemia: a prospective comparison of the time to positivity of hub-blood versus peripheral-blood cultures. Lancet. 1999. 354:1071–1077.
Article178. Raad I, Hanna HA, Alakech B, Chatzinikolaou I, Johnson MM, Tarrand J. Differential time to positivity: a useful method for diagnosing catheter-related bloodstream infections. Ann Intern Med. 2004. 140:18–25.
Article179. Krause R, Auner HW, Gorkiewicz G, Wolfler A, Daxboeck F, Linkesch W, Krejs GJ, Wenisch C, Reisinger EC. Detection of catheter-related bloodstream infections by the differential-time-to-positivity method and gram stain-acridine orange leukocyte cytospin test in neutropenic patients after hematopoietic stem cell transplantation. J Clin Microbiol. 2004. 42:4835–4837.
Article180. Abdelkefi A, Achour W, Ben Othman T, Torjman L, Ladeb S, Lakhal A, Hsairi M, Kammoun L, Ben Hassen A, Ben Abdeladhim A. Difference in time to positivity is useful for the diagnosis of catheter-related bloodstream infection in hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2005. 35:397–401.
Article181. Blot F, Schmidt E, Nitenberg G, Tancrede C, Leclercq B, Laplanche A, Andremont A. Earlier positivity of central-venous-versus peripheral-blood cultures is highly predictive of catheter-related sepsis. J Clin Microbiol. 1998. 36:105–109.
Article182. Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009. 49:1–45.
Article183. Wilcox MH, Tack KJ, Bouza E, Herr DL, Ruf BR, Ijzerman MM, Croos-Dabrera RV, Kunkel MJ, Knirsch C. Complicated skin and skin-structure infections and catheter-related bloodstream infections: noninferiority of linezolid in a phase 3 study. Clin Infect Dis. 2009. 48:203–212.
Article184. Kim SH, Kang CI, Kim HB, Youn SS, Oh MD, Kim EC, Park SY, Kim BK, Choe KW. Outcomes of Hickman catheter salvage in febrile neutropenic cancer patients with Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2003. 24:897–904.
Article185. Dugdale DC, Ramsey PG. Staphylococcus aureus bacteremia in patients with Hickman catheters. Am J Med. 1990. 89:137–141.
Article186. Pizzo PA, Robichaud KJ, Gill FA, Witebsky FG. Empiric antibiotic and antifungal therapy for cancer patients with prolonged fever and granulocytopenia. Am J Med. 1982. 72:101–111.
Article187. EORTC International Antimicrobial Therapy Cooperative Group. Empiric antifungal therapy in febrile granulocytopenic patients. Am J Med. 1989. 86:668–672.188. Klastersky J. Empirical antifungal therapy. Int J Antimicrob Agents. 2004. 23:105–112.
Article189. Wingard JR. Empirical antifungal therapy in treating febrile neutropenic patients. Clin Infect Dis. 2004. 39:Suppl 1. S38–S43.
Article190. Goldberg E, Gafter-Gvili A, Robenshtok E, Leibovici L, Paul M. Empirical antifungal therapy for patients with neutropenia and persistent fever: Systematic review and meta-analysis. Eur J Cancer. 2008. 44:2192–2203.
Article191. Nivoix Y, Velten M, Letscher-Bru V, Moghaddam A, Natarajan-Ame S, Fohrer C, Lioure B, Bilger K, Lutun P, Marcellin L, Launoy A, Freys G, Bergerat JP, Herbrecht R. Factors associated with overall and attributable mortality in invasive aspergillosis. Clin Infect Dis. 2008. 47:1176–1184.
Article192. Yoo JH, Choi JH, Lee DG, Choi S, Shin WS, Kim CC. Analysis of invasive fungal infection after hematopoietic stem cell transplantation or chemotherapy in patients with hematologic diseases. Infect Chemother. 2004. 36:40–45.193. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008. 46:327–360.
Article194. Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, Filler SG, Fisher JF, Kullberg BJ, Ostrosky-Zeichner L, Reboli AC, Rex JH, Walsh TJ, Sobel JD. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009. 48:503–535.
Article195. Michallet M, Ito JI. Approaches to the management of invasive fungal infections in hematologic malignancy and hematopoietic cell transplantation. J Clin Oncol. 2009. 27:3398–3409.
Article196. Lee JS, Shin JH, Lee K, Kim MN, Shin BM, Uh Y, Lee WG, Lee HS, Chang CL, Kim SH, Shin MG, Suh SP, Ryang DW. Species distribution and susceptibility to azole antifungals of Candida bloodstream isolates from eight university hospitals in Korea. Yonsei Med J. 2007. 48:779–786.
Article197. Bal AM, Gould IM. Empirical antimicrobial treatment for chemotherapy-induced febrile neutropenia. Int J Antimicrob Agents. 2007. 29:501–509.
Article198. Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz C, Bodensteiner D, Pappas P, Seibel N, Greenberg RN, Dummer S, Schuster M, Holcenberg JS. National Institute of Allergy and Infectious Diseases Mycoses Study Group. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. N Engl J Med. 1999. 340:764–771.
Article199. Walsh TJ, Pappas P, Winston DJ, Lazarus HM, Petersen F, Raffalli J, Yanovich S, Stiff P, Greenberg R, Donowitz G, Schuster M, Reboli A, Wingard J, Arndt C, Reinhardt J, Hadley S, Finberg R, Laverdiere M, Perfect J, Garber G, Fioritoni G, Anaissie E, Lee J. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med. 2002. 346:225–234.
Article200. Walsh TJ, Teppler H, Donowitz GR, Maertens JA, Baden LR, Dmoszynska A, Cornely OA, Bourque MR, Lupinacci RJ, Sable CA, dePauw BE. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med. 2004. 351:1391–1402.
Article201. Girmenia C, Barosi G, Aversa F, Bacigalupo A, Barbui T, Baronciani D, Bosi A, Candoni A, Locasciulli A, Locatelli F, Menichetti F, Musso M, Viscoli C, Rambaldi A. Prophylaxis and treatment of invasive fungal diseases in allogeneic stem cell transplantation: results of a consensus process by Gruppo Italiano Trapianto di Midollo Osseo (GITMO). Clin Infect Dis. 2009. 49:1226–1236.
Article202. Prentice HG, Hann IM, Herbrecht R, Aoun M, Kvaloy S, Catovsky D, Pinkerton CR, Schey SA, Jacobs F, Oakhill A, Stevens RF, Darbyshire PJ, Gibson BE. A randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyrexia of unknown origin in neutropenic patients. Br J Haematol. 1997. 98:711–718.
Article203. Boogaerts M, Winston DJ, Bow EJ, Garber G, Reboli AC, Schwarer AP, Novitzky N, Boehme A, Chwetzoff E, De Beule K. Intravenous and oral itraconazole versus intravenous amphotericin B deoxycholate as empirical antifungal therapy for persistent fever in neutropenic patients with cancer who are receiving broad-spectrum antibacterial therapy. A randomized, controlled trial. Ann Intern Med. 2001. 135:412–422.
Article204. Park SH, Choi SM, Lee DG, Choi JH, Yoo JH, Min WS, Shin WS. Intravenous itraconazole vs. amphotericin B deoxycholate for empirical antifungal therapy in patients with persistent neutropenic fever. Korean J Intern Med. 2006. 21:165–172.
Article205. Schuler U, Bammer S, Aulitzky WE, Binder C, Bohme A, Egerer G, Sandherr M, Schwerdtfeger R, Silling G, Wandt H, Glasmacher A, Ehninger G. Safety and efficacy of itraconazole compared to amphotericin B as empirical antifungal therapy for neutropenic fever in patients with haematological malignancy. Onkologie. 2007. 30:185–191.
Article206. Segal BH. Aspergillosis. N Engl J Med. 2009. 360:1870–1884.
Article207. Winston DJ, Hathorn JW, Schuster MG, Schiller GJ, Territo MC. A multicenter, randomized trial of fluconazole versus amphotericin B for empiric antifungal therapy of febrile neutropenic patients with cancer. Am J Med. 2000. 108:282–289.
Article208. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Munoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008. 46:1813–1821.
Article209. Ben-Ami R, Lewis RE, Kontoyiannis DP. Invasive mould infections in the setting of hematopoietic cell transplantation: current trends and new challenges. Curr Opin Infect Dis. 2009. 22:376–384.
Article210. Maertens J, Theunissen K, Verhoef G, Verschakelen J, Lagrou K, Verbeken E, Wilmer A, Verhaegen J, Boogaerts M, Van Eldere J. Galactomannan and computed tomography-based preemptive antifungal therapy in neutropenic patients at high risk for invasive fungal infection: a prospective feasibility study. Clin Infect Dis. 2005. 41:1242–1250.
Article211. Cordonnier C, Pautas C, Maury S, Vekhoff A, Farhat H, Suarez F, Dhedin N, Isnard F, Ades L, Kuhnowski F, Foulet F, Kuentz M, Maison P, Bretagne S, Schwarzinger M. Empirical versus preemptive antifungal therapy for high-risk, febrile, neutropenic patients: a randomized, controlled trial. Clin Infect Dis. 2009. 48:1042–1051.
Article212. Yoo JH, Choi JH, Choi SM, Lee DG, Shin WS, Min WS, Kim CC. Application of nucleic acid sequence-based amplification for diagnosis of and monitoring the clinical course of invasive aspergillosis in patients with hematologic diseases. Clin Infect Dis. 2005. 40:392–398.
Article213. Mennink-Kersten MA, Verweij PE. Non-culture-based diagnostics for opportunistic fungi. Infect Dis Clin North Am. 2006. 20:711–727. viii
Article214. Song KH, Lee S, Jang HC, Jeon JH, Park WB, Park KU, Park SW, Oh MD, Choe KW. Diagnostic usefulness of galactomannan assay for invasive aspergillosis. Infect Chemother. 2009. 41:82–89.
Article215. O'Shaughnessy EM, Shea YM, Witebsky FG. Laboratory diagnosis of invasive mycoses. Infect Dis Clin North Am. 2003. 17:135–158.216. Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006. 42:1417–1427.
Article217. Hachem RY, Kontoyiannis DP, Chemaly RF, Jiang Y, Reitzel R, Raad I. Utility of galactomannan enzyme immunoassay and (1,3) beta-D-glucan in diagnosis of invasive fungal infections: low sensitivity for Aspergillus fumigatus infection in hematologic malignancy patients. J Clin Microbiol. 2009. 47:129–133.
Article218. Yoo JH, Choi SM, Lee DG, Park SH, Choi JH, Kwon EY, Shin WS. Comparison of the real-time nucleic acid sequence-based amplification (RTi-NASBA) with conventional NASBA, and galactomannan assay for the diagnosis of invasive aspergillosis. J Korean Med Sci. 2007. 22:672–676.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evidence-Based Guidelines for Empirical Therapy of Neutropenic Fever in Korea
- Intravenous Itraconazole vs. Amphotericin B Deoxycholate for Empirical Antifungal Therapy in Patients with Persistent Neutropenic Fever
- The Effect of Empirical Antibiotics in Febrile Neutropenia
- Optimizing Helicobacter pylori Treatment: An Updated Review of Empirical and Susceptibility Test-Based Treatments
- Childhood Fever Management: Current Practice vs Evidence