Neurointervention.
2014 Sep;9(2):106-108. 10.5469/neuroint.2014.9.2.106.
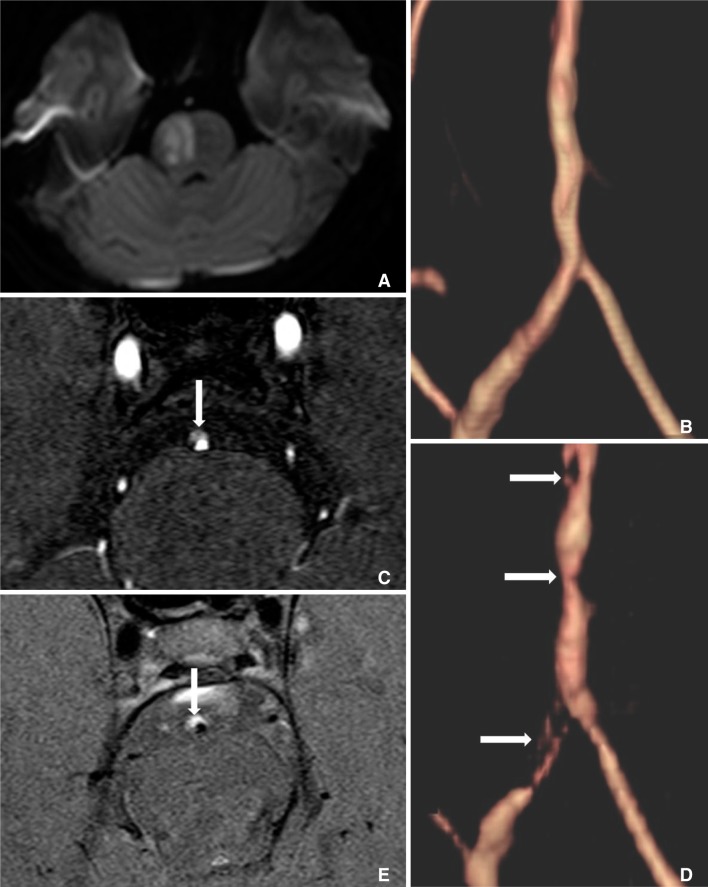
Rapid Progression of Symptomatic Vertebrobasilar Artery Dissection on Magnetic Resonance Imaging: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, IS Hallym Medical Center, Incheon, Korea. khs501@hanmail.net
- 2Department of Radiology, Chonbuk National University Medical School and Hospital, Jeonju, Korea.
- KMID: 1910767
- DOI: http://doi.org/10.5469/neuroint.2014.9.2.106
Abstract
- Spontaneous intracranial vertebrobasilar dissection can manifest with various clinical symptoms, including subarachnoid hemorrhage or ischemic symptoms from impaired posterior circulation. A 29-year-old woman came to our emergency department with a sudden onset of left sided mild motor weakness and headache. Initial magnetic resonance imaging (MRI) showed mild luminal irregularities in the vertebrobasilar arteries with an eccentric periluminal hematoma. Follow-up MRI obtained 3 days later showed a progression of vertebrobasilar dissection to multifocal stenoses with an increased intramural hematoma.
MeSH Terms
Figure
Reference
-
1. Hosoya T, Adachi M, Yamaguchi K, Haku T, Kayama T, Kato T. Clinical and neuroradiological features of intracranial vertebrobasilar artery dissection. Stroke. 1999; 30:1083–1090. PMID: 10229748.
Article2. Yamaura A, Ono J, Hirai S. Clinical picture of intracranial non-traumatic dissecting aneurysm. Neuropathology. 2000; 20:85–90. PMID: 10935444.
Article3. Tsukahara T, Minematsu K. Overview of spontaneous cervicocephalic arterial dissection in Japan. Acta Neurochir Suppl. 2010; 107:35–40. PMID: 19953368.
Article4. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001; 344:898–906. PMID: 11259724.
Article5. Arauz A, Marquez JM, Artigas C, Balderrama J, Orrego H. Recanalization of vertebral artery dissection. Stroke. 2010; 41:717–721. PMID: 20150549.
Article6. Kim BM, Kim SH, Kim DI, Shin YS, Suh SH, Kim DJ, et al. Outcomes and prognostic factors of intracranial unruptured vertebrobasilar artery dissection. Neurology. 2011; 76:1735–1741. PMID: 21576691.
Article7. Yoshimoto Y, Wakai S. Unruptured intracranial vertebral artery dissection. Clinical course and serial radiographic imagings. Stroke. 1997; 28:370–374. PMID: 9040692.8. Ahn SS, Kim BM, Suh SH, Kim DJ, Kim DI, Shin YS, et al. Spontaneous symptomatic intracranial vertebrobasilar dissection: initial and follow-up imaging findings. Radiology. 2012; 264:196–202. PMID: 22550310.
Article9. Arnold M, Bousser MG, Fahrni G, Fischer U, Georqiadis D, Gandjour J, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke. 2006; 37:2499–2503. PMID: 16960096.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experiences of Unruptured Vertebral Artery Dissection
- Vertebrobasilar Occlusion Presenting as Sudden Isolated Bilateral Sensorineural Hearing Loss: Case Report
- Diagnostic Usefulness of High Resolution Cross Sectional MRI in Symptomatic Middle Cerabral Arterial Dissection
- Differential Imaging Features of Pulmonary Artery Dissection from Other Intraluminal Diseases of Pulmonary Artery: Two Cases Report
- Spontaneous Intracranial Vertebral Artery Dissection in a 2-Year-Old Child Diagnosed with High-Resolution MRI: a Case Report