Prog Med Phys.
2013 Dec;24(4):271-277. 10.14316/pmp.2013.24.4.271.
Convolution-Superposition Based IMRT Plan Study for the PTV Containing the Air Region: A Prostate Cancer Case
- Affiliations
-
- 1Department of Radiation Oncology, Hallym University College of Medicine, Seoul, Korea. seikang@hallym.or.kr
- KMID: 1910569
- DOI: http://doi.org/10.14316/pmp.2013.24.4.271
Abstract
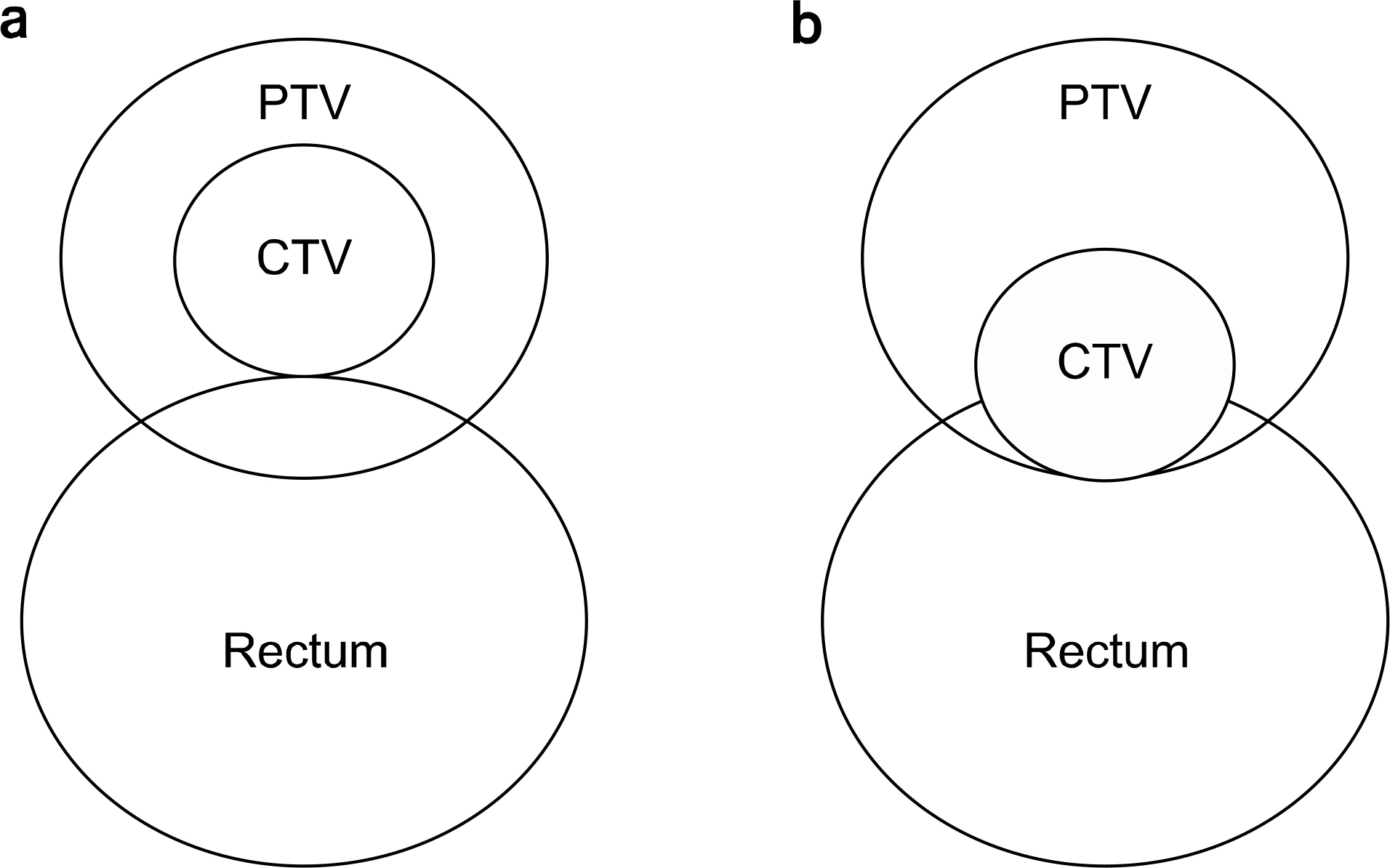
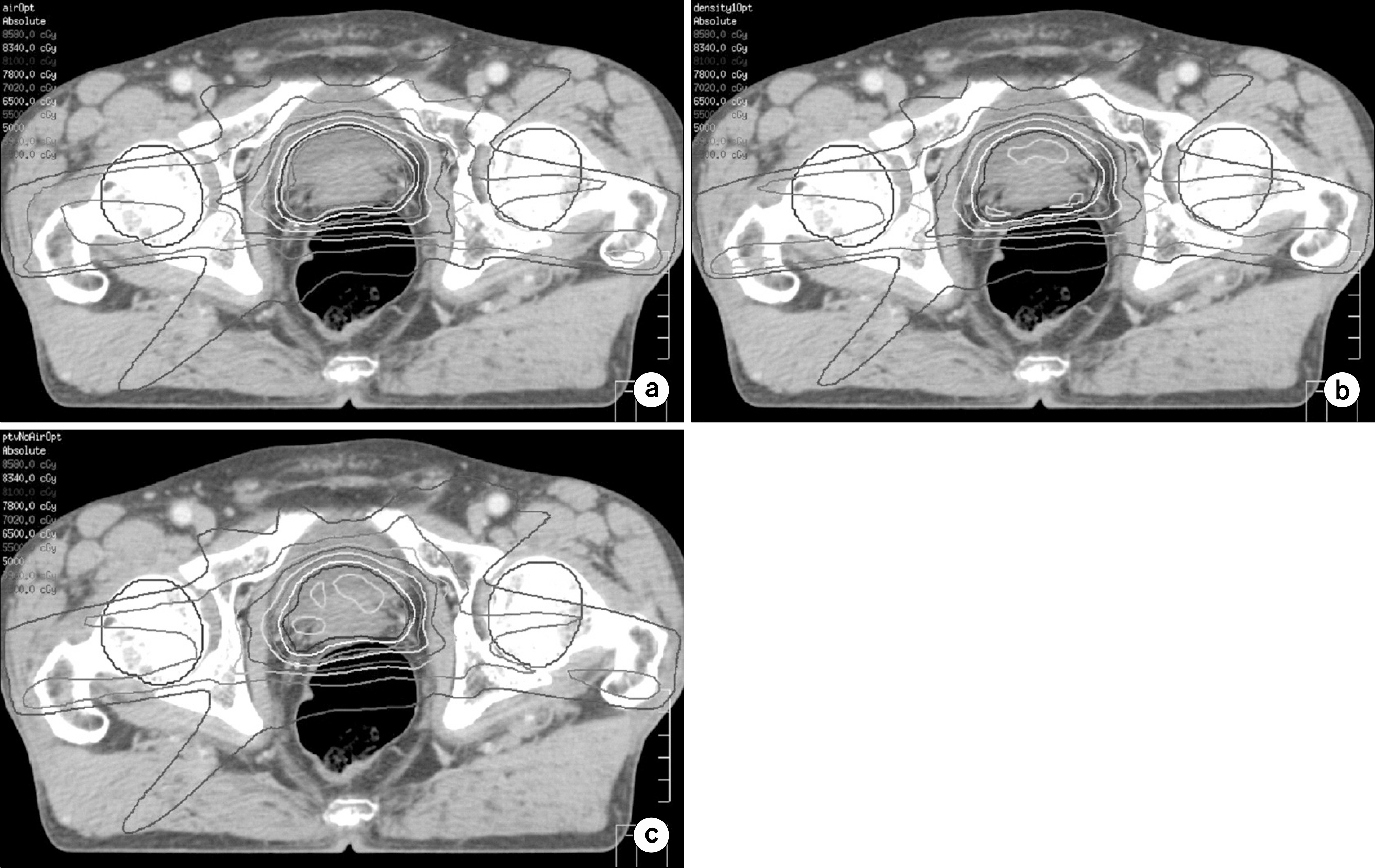
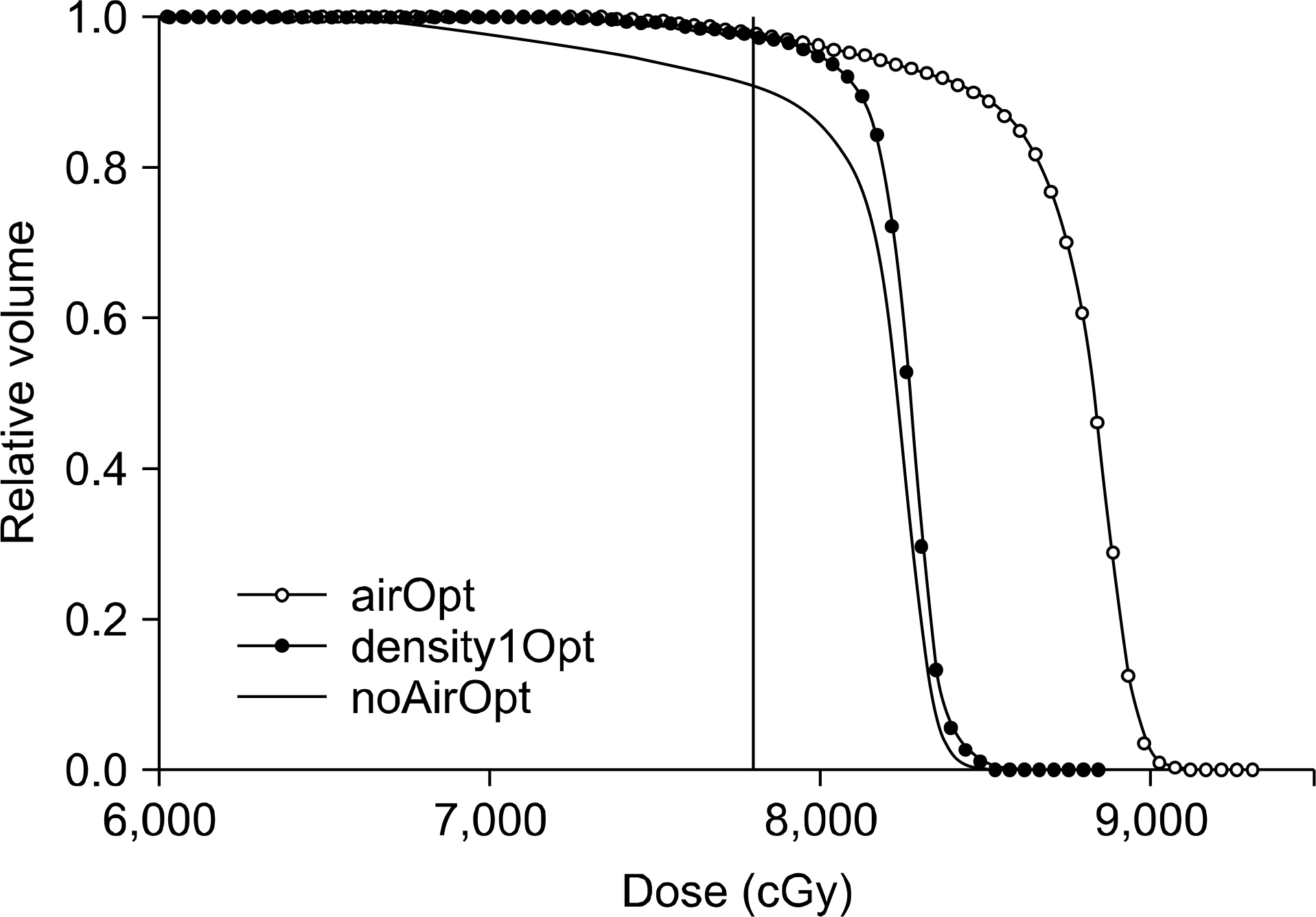
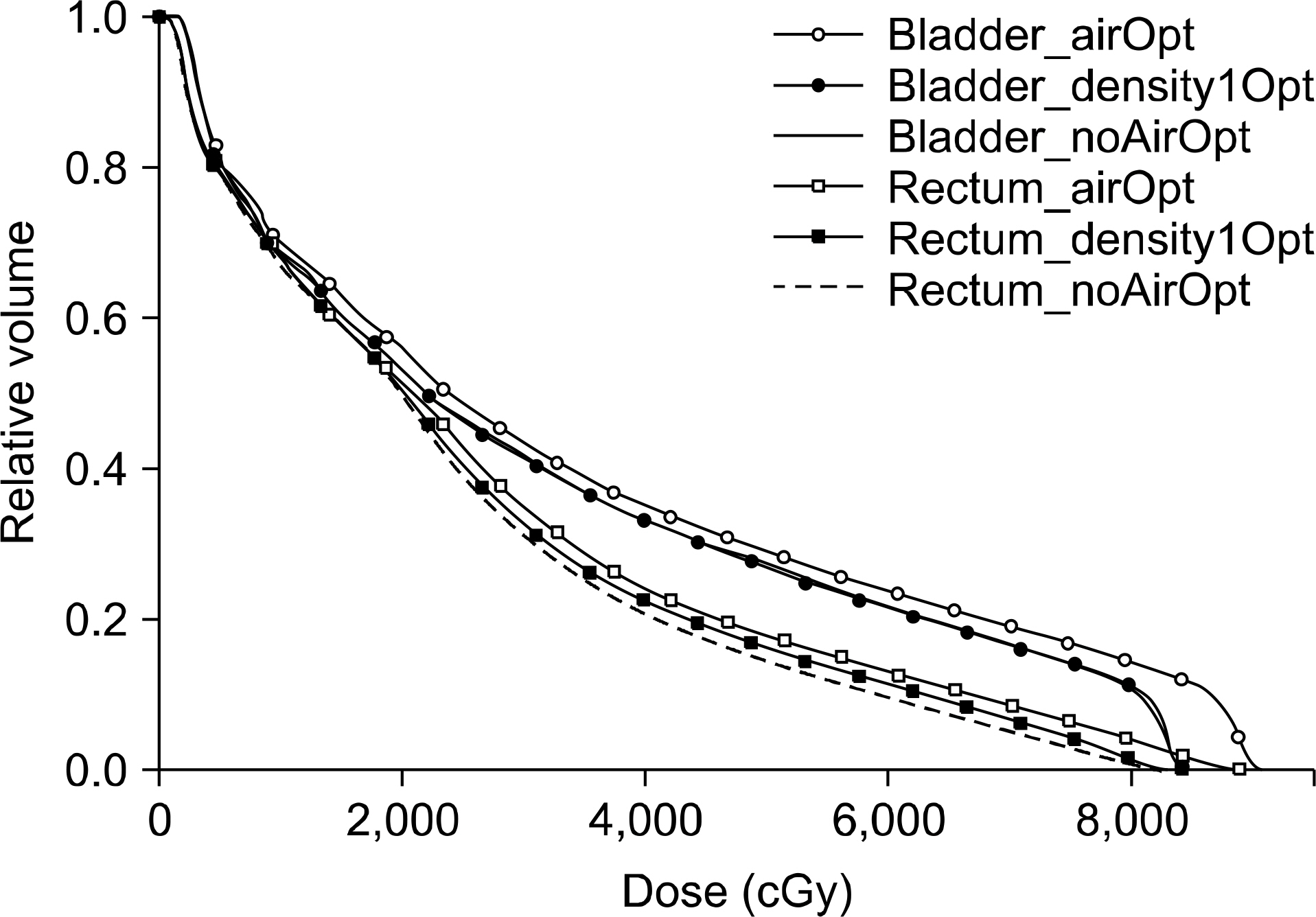
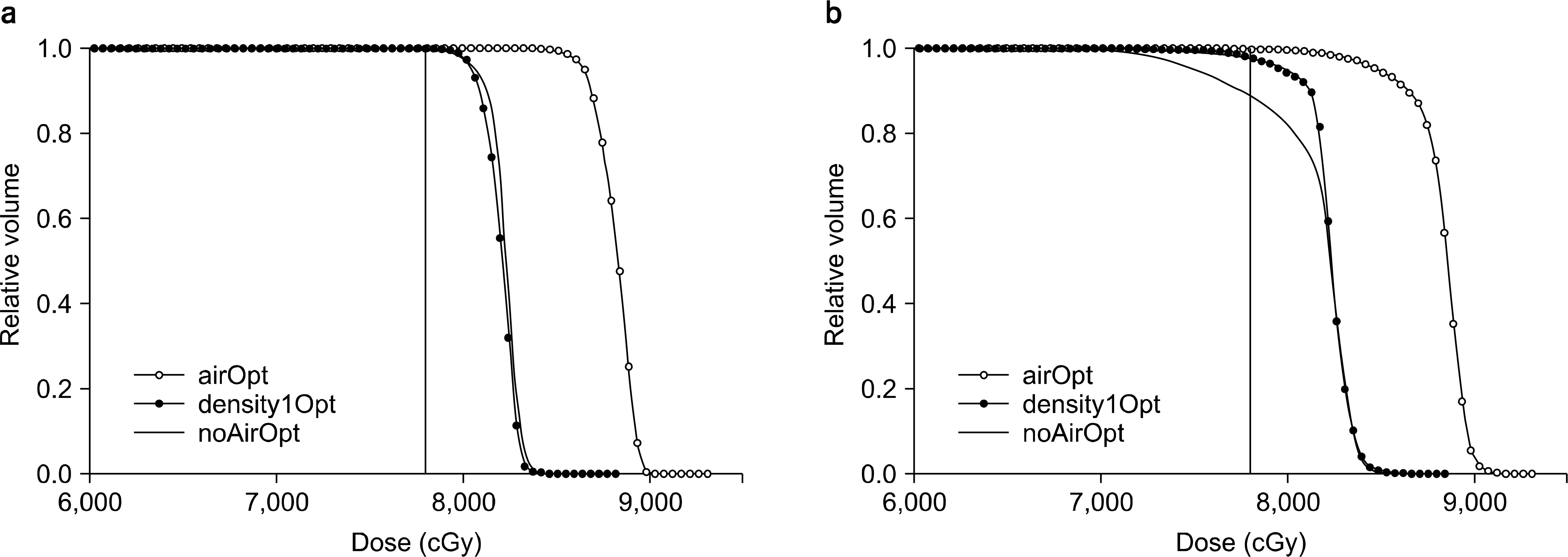
- In prostate IMRT planning, the planning target volume (PTV), extended from a clinical target volume (CTV), often contains an overlap air volume from the rectum, which poses a problem inoptimization and prescription. This study was aimed to establish a planning method for such a case. There can be three options in which volume should be considered the target during optimization process; PTV including the air volume of air density ('airOpt'), PTV including the air volume of density value one, mimicking the tissue material ('density1Opt'), and PTV excluding the air volume ('noAirOpt'). Using 10 MV photon beams, seven field IMRT plans for each target were created with the same parameter condition. For these three cases, DVHs for the PTV, bladder and the rectum were compared. Also, the dose coverage for the CTV and the shifted CTV were evaluated in which the shifted CTV was a copied and translated virtual CTV toward the rectum inside the PTV, thus occupying the initial position of the overlap air volume, simulating the worst condition for the dose coverage in the target. Among the three options, only density1Opt plan gave clinically acceptable result in terms of target coverage and maximum dose. The airOpt plan gave exceedingly higher dose and excessive dose coverage for the target volume whereas noAirOpt plan gave underdose for the shifted CTV. Therefore, for prostate IMRT plan, having an air region in the PTV, density modification of the included air to the value of one, is suggested, prior to optimization and prescription for the PTV. This idea can be equally applied to any cases including the head and neck cancer with the PTV having the overlapped air region. Further study is being under process.
Keyword
Figure
Reference
-
1. Solberg TD, Holly FE, De Salles AA, Wallace RE, Smathers JB. Implications of tissue heterogeneity for radiosurgery in head and neck tumors. Int J Radiat Oncol Biol Phys. 32(1):235–239. 1995.
Article2. Kan WK, Wu PM, Leung HT, et al. The effect of the nasopharyngeal air cavity on x-ray interface doses. Phys Med Biol. 43(3):529–537. 1998.
Article3. Waldron JN, O'Sullivan B, Warde P, et al. Ethmoid sinus cancer: twenty-nine cases managed with primary radiation therapy. Int J Radiat Oncol Biol Phys. 41(2):361–369. 1998.
Article4. Davidson SE, Ibbott GS, Prado KL, Dong L, Liao Z, Followill DS. Accuracy of two heterogeneity dose calculation algorithms for IMRT in treatment plans designed using an anthropomorphic thorax phantom. Med Phys. 34(5):1850–1857. 2007.
Article5. Tillikainen L, Helminen H, Torsti T, et al. A 3D pencil- beam-based superposition algorithm for photon dose calculation in heterogeneous media. Phys Med Biol. 53(14):3821–3839. 2008.6. Han T, Mikell JK, Salehpour M, Mourtada F. Dosimetric comparison of Acuros XB deterministic radiation transport method with Monte Carlo and model-based convolution methods in heterogeneous media. Med Phys. 38(5):2651–2664. 2011.
Article7. Takahashi W, Yamashita H, Saotome N, et al. Evaluation of heterogeneity dose distributions for Stereotactic Radiotherapy (SRT): comparison of commercially available Monte Carlo dose calculation with other algorithms. Radiat Oncol. 7:20. 2012.
Article8. Teh BS, Mai WY, Uhl BM, et al. Intensity-modulated radiation therapy (IMRT) for prostate cancer with the use of a rectal balloon for prostate immobilization: acute toxicity and dose-volume analysis. Int J Radiat Oncol Biol Phys. 49(3):705–712. 2001.
Article9. McGary JE, Teh BS, Butler EB, Grant W 3rd. Prostate immobilization using a rectal balloon. J Appl Clin Med Phys. 3(1):6–11. 2002.
Article10. Wachter S, Gerstner N, Dorner D, et al. The influence of a rectal balloon tube as internal immobilization device on variations of volumes and dose-volume histograms during treatment course of conformal radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 52(1):91–100. 2002.
Article11. Miralbell R, Molla M, Arnalte R, et al. Target repositioning optimization in prostate cancer: is intensity-modulated radiotherapy under stereotactic conditions feasible? Int J Radiat Oncol Biol Phys. 59(2):366–371. 2004.
Article12. Teh BS, Dong L, McGary JE, Mai WY, Grant W 3rd, Butler EB. Rectal wall sparing by dosimetric effect of rectal balloon used during intensity-modulated radiation therapy (IMRT) for prostate cancer. Med Dosim. 30(1):25–30. 2005.
Article13. Song JS, Court LE, Cormack RA. Monte Carlo calculation of rectal dose when using an intrarectal balloon during prostate radiation therapy. Med Dosim. 32(3):151–156. 2007.
Article14. Hardcastle N, Metcalfe PE, Rosenfeld AB, Tome WA. Endorectal balloon cavity dosimetry in a phantom: performance under IMRT and helical tomotherapy beams. Radiother Oncol. 92(1):48–56. 2009.
Article15. Smeenk RJ, Teh BS, Butler EB, van Lin EN, Kaanders JH. Is there a role for endorectal balloons in prostate radiotherapy? A systematic review. Radiother Oncol. 95(3):277–282. 2010.
Article16. Srivastava SP, Das IJ, Kumar A, Johnstone PA, Cheng CW. Impact of rectal balloon-filling materials on the dosimetry of prostate and organs at risk in photon beam therapy. J Appl Clin Med Phys. 14(1):81–91. 2013.
Article17. ICRU Report 62. International Commission on Radiation Units and Measurements. Prescribing, Recording, and Reporting Photon Beam Therapy (supplement to ICRU Report 50), Bethesda, MD. 1999.18. de Crevoisier R, Tucker SL, Dong L, et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys. 62(4):965–973. (2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dose Distribution of Intensity Modulated Radiation Therapy in Prostate Cancer
- Dosimetric and Radiobiological Evaluation of Dose Volume Optimizer (DVO) and Progressive Resolution Optimizer (PRO) Algorithm against Photon Optimizer on IMRT and VMAT Plan for Prostate Cancer
- Application of Intensity Modulated Radiation Therapy (IMRT) in Prostate Cancer
- Evaluation of Dose Distributions Recalculated with Per-field Measurement Data under the Condition of Respiratory Motion during IMRT for Liver Cancer
- Impact of Respiratory Motion on Breast Cancer Intensity-modulated Radiation Therapy