Prog Med Phys.
2014 Sep;25(3):176-184. 10.14316/pmp.2014.25.3.176.
Comparison of Dose Distribution in Spine Radiosurgery Plans: Simultaneously Integrated Boost and RTOG 0631 Protocol
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dongryul.oh@samsung.com
- KMID: 1910550
- DOI: http://doi.org/10.14316/pmp.2014.25.3.176
Abstract
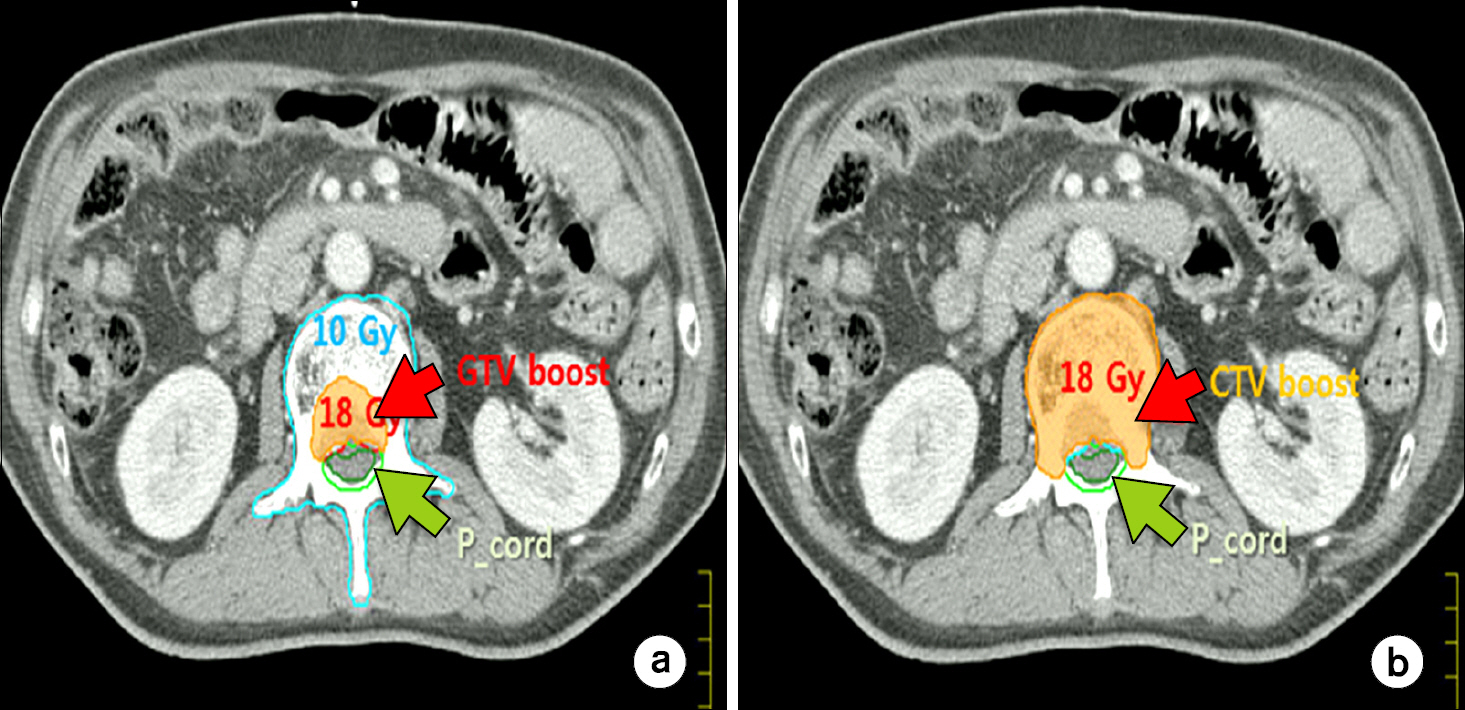
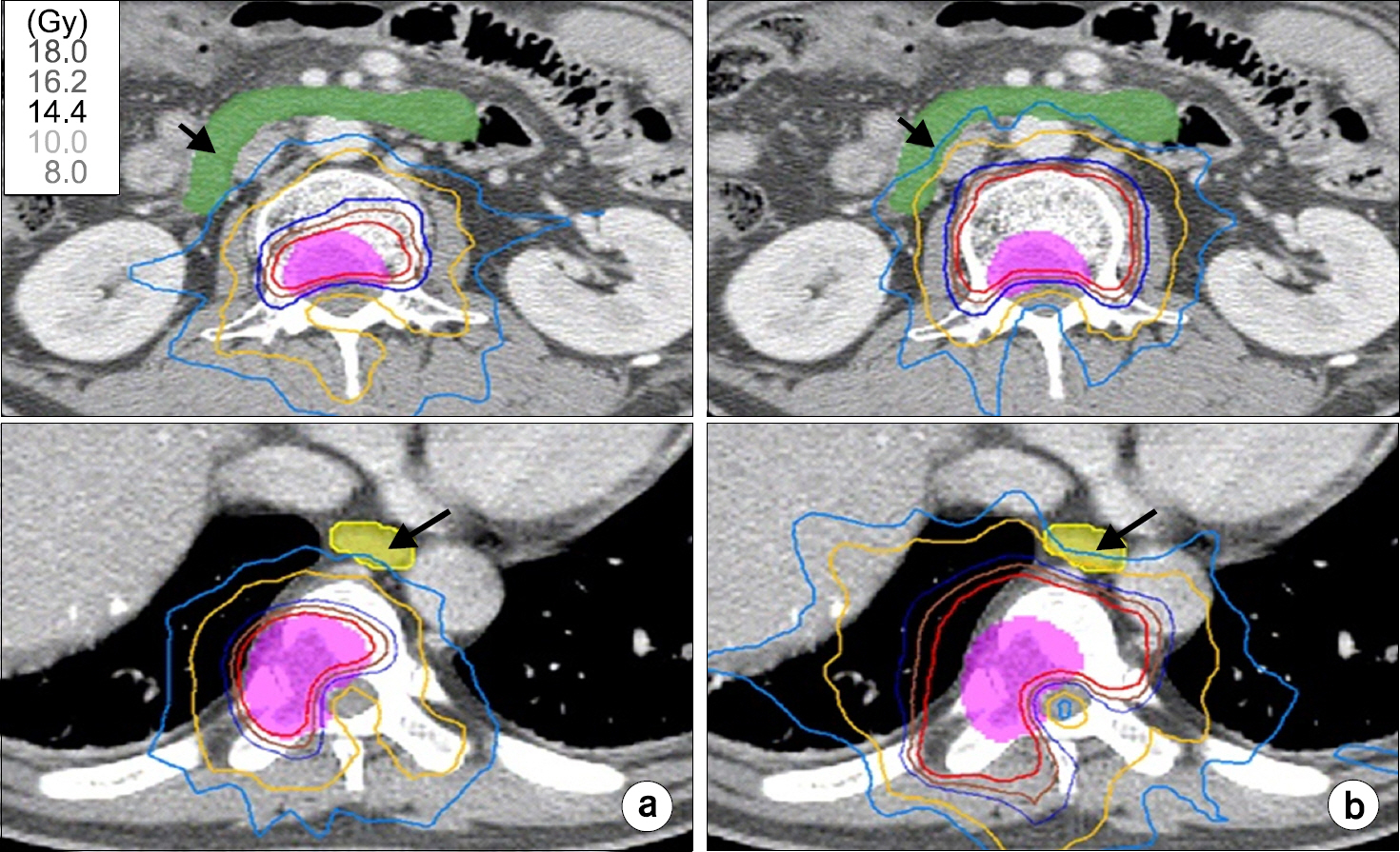
- In this study, we compareddose distributions from simultaneously integrated boost (SIB) method versus the RTOG 0631 protocol for spine radiosurgery. Spine radiosurgery plans wereperformed in five patients with localized spinal metastases from hepatocellular carcinoma. The computed tomography (CT) and T1- and T2-weighted magnetic resonance imaging (MRI) were fused for delineating of GTV and spinal cord. In SIB plan, the clinical target volume (CTV1) was included the whole compartments of the involved spine, while RTOG 0631 protocol defines the CTV2 as the involved vertebral body and both left and right pedicles. The CTV2 includes transverse process and posterior element according to the extent of GTV. The doses were prescribed 18 Gy to GTV and 10 Gy to CTV1 in SIB plan, while the prescription of RTOG 0631 protocol was applied 18 Gy to CTV2. The results of dose-volume histogram (DVH) showed that there were competitive in target coverage, while the doses of spinal cord andother normal organs were lower in SIB method than in RTOG 0631 protocol. The 85% irradiated volume of VB in RTOG 0631 protocol was similar to that in the SIB plan. However, the dose to normal organs in RTOG 0631 had a tendency to higher than that in SIB plan. The SIB plan might be an alternative method in case of predictive serious complications of surrounded normal organs. In conclusion, although both approaches of SIB or RTOG 0631 showed competitive planning results, tumor control probability (TCP) and normal tissue complication probability (NTCP) through diverse clinical researches should be analyzed in the future.
MeSH Terms
Figure
Reference
-
References
1. Sahgal A, Larson DA, Chang EL, et al. Stereotactic body radiosurgery for spine metastases: a critical review. Int J RadiatOncolBiolPhys. 71:652–665. 2008.2. Orit G, Annette E, Rojano K, et al. Influence of rotiations on dose distributions in spinal stereoractic body radiationtherapy (SBRT). Int J RadiatOncolBiolPhys. 73:1596–1601. 2009.3. Yamada Y, Bilskv MH, Lovaelock DM, et al. High-dose single-fraction, imageguided intensitymodulated radiotherapy formetastatic spinal lesion. Int J RadiatOncolBiol Phys. 71:484–490. 2008.4. Stefano S, Winston W, Jain-Yue J, et al. Spine Radiosurgery: A dosimetric analysis in 124 patients who recived 18 Gy Int J RadiatOncolBiolPhys. 84:571–576. 2012.5. Ryu S, Rock J, Jain R, et al. Radiosurgical decompression of metastatic epidural compression. Cancer. 116:2250–2257. 2010.
Article6. Sunyoung L, Mison C, Mijo L. Stereotactic body radiotherapy for solitary spine metastasis. Radiat Oncol J. 31(4):260–266. 2013.7. Gerszten PC, Germanwala A, Burton SA, et al. Combination kyphoplasty and spinal radiosurgery: a new treatment paradigm for pathological fracture. J. Neurosurg. Spine. 3(4):296–301. 2005.8. Jin JY, Chen Q, Jin R, et al. Technical and clinical experience with spine radiosurgery: a new technology for management of localized spine metastases. Technology Cancer Res Treat. 6:127–133. 2007.
Article9. Gerszten PC, Burton SA, Ozhasoglu C, et al. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine. 32:193–199. 2007.10. Ryu S, Gerszten PC, Timmerman R, et al. RTOG 0631 study protocol: Phase II/III study of imageguided radiosurgery/SBRT for localized spine metastasis. Availableat:. http://www.rtog. org/members/protocols/0631.pdf. Accessed.11. Cox B, Spratt D, Lovelock M, et al. International Spine Radiosurgery Consortium consensus guidelines for target volume definitions for target volume definition in spinal stereotatic surgery. Int J RadiatOncolBiolPhys. 83(5):e597–605. 2012.12. Stefano SP, Winston W, Jain-Yue J, et al. Spine radiosurgery: A dosimetric analysis in 124 patients who received 18Gy. Int J RadiatOncolBiolPhys. 5:571–576. 2012.13. Soo-Min C, Gi Woong L, Seok Hyun S. The effect of multileaf collimator leaf width on the radiosurgery planning for spine lesion treatment in terms of the modulated techniques and target complexity Radiation Oncology. 9:72. 2014.14. Timmerman R. An overview of hypofractional and introduction to this issue of seminars in radiation Oncology. Semin Radiat Oncol. 18(4):215–222. 2008.15. Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. ClinOncol(R CollRadiol). 24(2):112–24. 2012.
Article16. Kristopher D, Leila M, Liang Z, et al. Single fraction conventional external beam radiation therapy for bone metastases: A systemic review of randomized controlled trials. Radiother and Oncol. 106:5–14. 2013.17. Max D, Jaap D, Esther S, et al. Imaging for stereotatic spine radiotherapy: Clinical consideration. Int. J RadiatOncolBiolPhys. 81(2):321–330. 2011.18. David C, Matthew B, Khoi N, et al. Genealizable Class Solution for Treatment Plannig of Spinal Sterotactic Body Radiation Therapy. Int. J RadiatOncolBiolPhys. 84(3):847–853. 2012.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Volumetric-Modulated Arc Radiotherapy Using Knowledge-Based Planning: Application to Spine Stereotactic Body Radiotherapy
- Rapid Optimization of Multiple Isocenters Using Computer Search for Linear Accelerator-based Stereotactic Radiosurgery
- Impact of Intensity Modulated Radiation Therapy as aBoost Treatment on the Lung Dose Distributions for Non-Small-Cell Lung Cancer
- Dosimetric Plan Comparison of Accelerated Partial Breast Irradiation (APBI) Using CyberKnife
- An Integrated Logistic Formula for Dose Prescription in Radiosurgery