Korean J Hepatobiliary Pancreat Surg.
2014 Feb;18(1):21-25. 10.14701/kjhbps.2014.18.1.21.
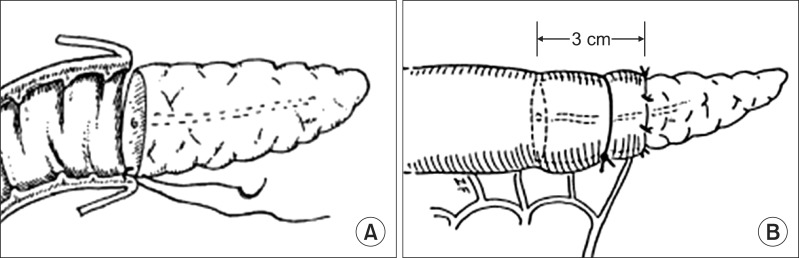
Preliminary results of binding pancreaticojejunostomy
- Affiliations
-
- 1Department of Surgery, Inha University Hospital, Incheon, Korea. siahn@inha.ac.kr
- KMID: 1890076
- DOI: http://doi.org/10.14701/kjhbps.2014.18.1.21
Abstract
- BACKGROUNDS/AIMS
The post-operative complications and clinical course of pancreaticoduodenectomy (PD) largely depend on the pancreaticojejunostomy (PJ). Several methods of PJ are in clinical use. We analyzed the early results of binding pancreaticojejunostomy (BPJ), a technique reported by SY Peng.
METHODS
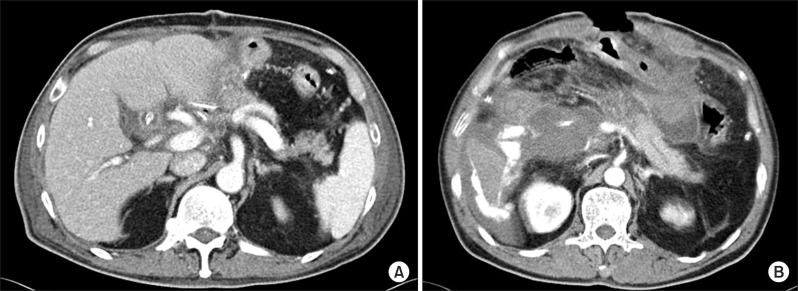
We retrospectively reviewed the clinical results of patients who received BPJ in Inha University Hospital from 2006 to 2011. 21 BPJs were performed with Peng's method. The definition of postoperative pancreatic fistula (PF) was a high amylase content (>3 times the upper normal serum value) of the drain fluid (of any measurable volume), at any time on or after the 3rd post-operative day. The pancreatic fistula was graded according to the International Study Group for Pancreatic Fistula (ISGPF) guidelines.
RESULTS
Of the 21 patients who received BPJ, 11 were male. The median age was 61.2 years. PD surgery included 4 cases of Whipple's procedures and 17 cases of pylorus-preserving PD. According to the post-operative course, 16 patients recovered well with no evidence of PF. A total of 5 patients (23.8%), including 3 grade A PFs and 2 grade C PFs, suffered from a pancreatic fistula. 3 patients with grade A PF recovered with conservative management.
CONCLUSIONS
The BPJ appears to be a relatively safe procedure based on this preliminary study, but further study is needed to validate its safety.
MeSH Terms
Figure
Reference
-
1. Shrikhande SV, Qureshi SS, Rajneesh N, et al. Pancreatic anastomoses after pancreaticoduodenectomy: do we need further studies? World J Surg. 2005; 29:1642–1649. PMID: 16311866.
Article2. Kakita A, Yoshida M, Takahashi T. History of pancreaticojejunostomy in pancreaticoduodenectomy: development of a more reliable anastomosis technique. J Hepatobiliary Pancreat Surg. 2001; 8:230–237. PMID: 11455485.
Article3. Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J Gastrointest Surg. 2006; 10:1199–1211. PMID: 17114007.
Article4. Büchler MW, Friess H, Wagner M, et al. Pancreatic fistula after pancreatic head resection. Br J Surg. 2000; 87:883–889. PMID: 10931023.
Article5. Mathur A, Pitt HA, Marine M, et al. Fatty pancreas: a factor in postoperative pancreatic fistula. Ann Surg. 2007; 246:1058–1064. PMID: 18043111.6. Peng S, Mou Y, Cai X, et al. Binding pancreaticojejunostomy is a new technique to minimize leakage. Am J Surg. 2002; 183:283–285. PMID: 11943127.
Article7. Peng SY, Wang JW, Li JT, et al. Binding pancreaticojejunostomy--a safe and reliable anastomosis procedure. HPB (Oxford). 2004; 6:154–160. PMID: 18333069.8. Peng SY, Wang JW, Lau WY, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007; 245:692–698. PMID: 17457161.9. Peng SY, Wang JW, Hong de F, et al. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011; 63:69–74. PMID: 21442343.
Article10. Buc E, Flamein R, Golffier C, et al. Peng's binding pancreaticojejunostomy after pancreaticoduodenectomy: a French prospective study. J Gastrointest Surg. 2010; 14:705–710. PMID: 20054660.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Binding Pancreaticojejunostomy Compared with Dunking Pancreaticojejunostomy
- Factors associated with pancreaticojejunostomy leak after pancreaticoduodenectomy
- Efficacy of Stented Pancreaticojejunostomy and Jejunojejunostomy after Pancreaticoduodenectomy
- Short-term Analysis of Pancreaticoduodenectomy with an Application of a Binding Pancreaticojejunostomy and an Endo GIA Stapler
- Studies on Factors Associated with Pancreaticojejunostomy Leak after Pancreaticoduodenectomy