Kosin Med J.
2014 Jun;29(1):1-10. 10.7180/kmj.2014.29.1.1.
Management of Low Bone Mass in Female Athletes
- Affiliations
-
- 1Department of Obstetrics and Gynecology, College of Medicine, Inje University, Sanggyepaik Hospital, Seoul, Korea. hchoi@paik.ac.kr
- KMID: 1882432
- DOI: http://doi.org/10.7180/kmj.2014.29.1.1
Abstract
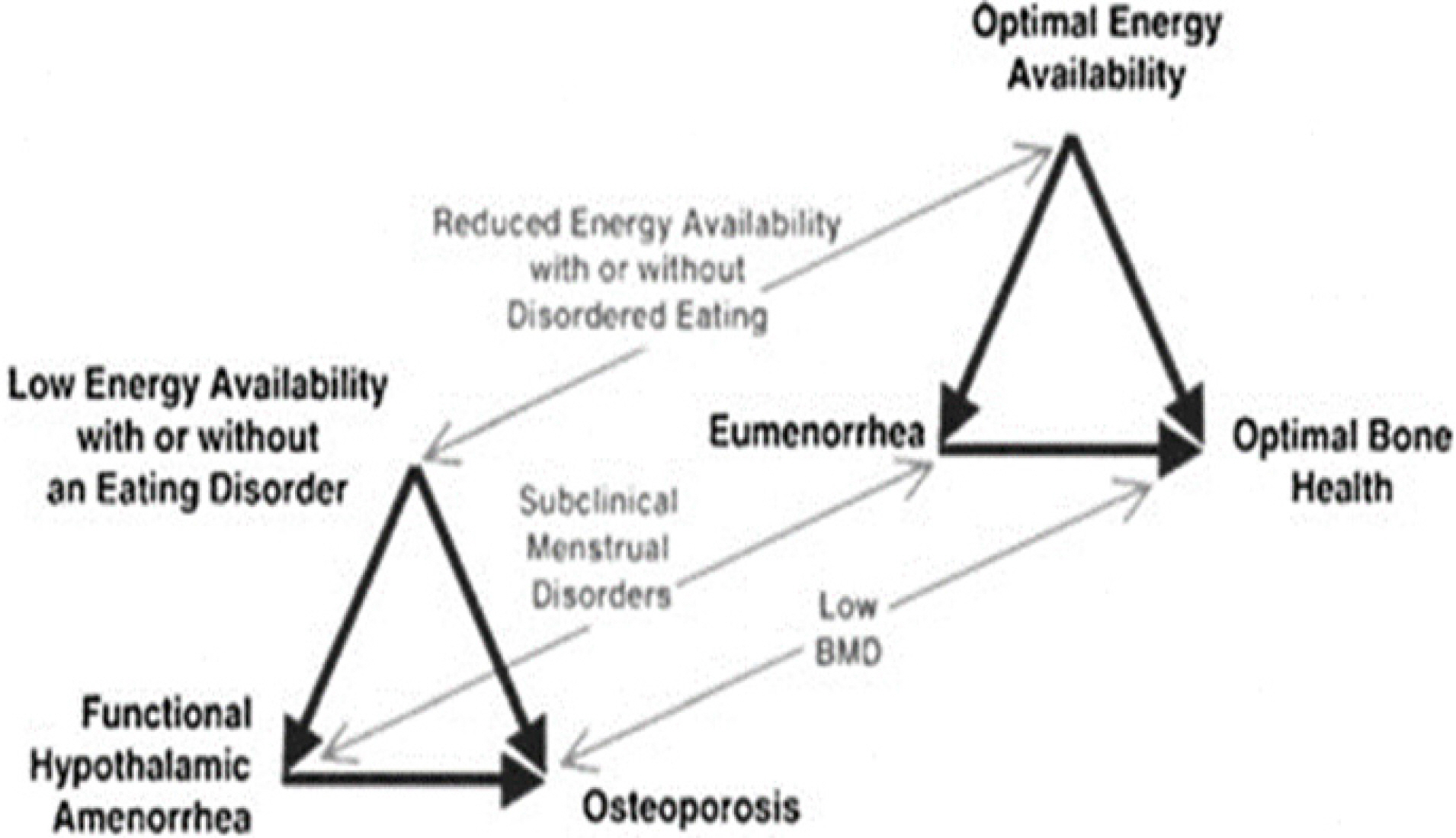
- As female athletic participation has increased, the positive effects of exercise on health have become evident. However, with this growth in sports activity, a set of health problems unique to the female athlete has emerged. The female athlete triad and its components can occur in females of all ages in every sport. The Female Athlete Triad poses serious health risks, both short and long term, to the overall well-being of affected individuals. Sustained low energy availability can impair health, causing many medical complications within the skeletal, endocrine, cardiovascular, reproductive, and central nervous systems. With the surge of females participating in athletics within the past 10 to 15 years, it is both conceivable and likely that the prevalence of this syndrome will continue to grow. Therefore, it is imperative that appropriate screening and diagnostic measures are enacted by a multidisciplinary team of health care providers, counselors, teachers, and dieticians in order to provide the proper care to affected athletes. Initial awareness should take place within the educational confines of elementary and high schools. Screening for female athletes exhibiting risk factors for the triad should also take place at the time of sports physicals. If one component of the triad is identified, the clinician should take the time to effectively workup the other. Treatment for each component of the triad includes both pharmacological and nonpharmacological measures, with emphasis placed upon increased energy availability and overall improved nutritional health. Using this all-encompassing type of approach, sports medicine practitioners should feel empowered to continue to promote the lifelong well-being of female athletes in the years to come.
MeSH Terms
Figure
Reference
-
1. Gibbs JC, Williams NI, De Souza MJ. Prevalence of individual and combined components of the female athlete triad. Med Sci Sports Exerc. 2013; 45:985–96.
Article2. Otis CL, Drinkwater B, Johnson M, Loucks A, Wilmone J. American College of Sports Medicine position stand: the Female Athlete Triad. Med Sci Sports Exerc. 1997; 29:i–ix.3. Nichols DL, Sanborn CF, Essery EV. Bone density and young athletic women: an update. Sports Med. 2007; 37:1001–14.4. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine. American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007; 39:1867–82.5. Lebrun CM. The Female Athlete Triad: what's a doctor to do? Curr Sports Med Rep. 2007; 6:397–404.
Article6. Beals KA, Hill AK. The prevalence of disordered eating, menstrual dysfunction, and low bone mineral density among US collegiate athletes. Int J Sports Nutr Exerc Metab. 2006; 16:1–23.
Article7. Hoch AZ, Pajewski NM, Moraski L, Carrera GF, Wilson CR, Hoffmann RG, et al. Prevalence of the Female Athlete Triad in high school athletes and sedentary students. Clin J Sports Med. 2009; 19:421–8.
Article8. Nattiv A, Loucks AB, Manore MM, et al. Position Stand: the female athlete triad. Med Sci Sports Exerc. 2007; 39:1867–82.9. Manore MM. Nutritional needs of the female athlete. Clin J Sports Med. 1999; 18:549–63.
Article10. Witkop CT, Warren MP. Understanding the spectrum of the Female Athlete Triad. Am Coll Obstet Gynecol. 2010; 116:1444–8.
Article11. Sundgot-Borgen J. Risk and trigger factors for the development of eating disorders in female elite athletes. Med Sci Sports Exerc. 1994; 26:414–9.
Article12. Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000; 8:344–53.
Article13. Kadel NJ, Teitz CC, Kronmal RA. Stress fractures in ballet dancers. Am J Sports Med. 1992; 20:445–9.
Article14. Gibbs JC, Williams NI, Scheid JL, Toombs RJ, De Souza MJ. The association of a high drive for thinness with energy deficiency and severe menstrual disturbances: confirmation in a large population of exercising women. Int J Sport Nutr Exerc Metab. 2011; 21:280–90.
Article15. Pritts SD, Susman J. Diagnosis of eating disorders in primary care. Am Fam Physician. 2003; 67:297–304.16. Sundgot-Borgen J. Risk and trigger factors for the development of eating disorders in female elite athletes. Med Sci Sports Exerc. 1994; 26:414–9.
Article17. Byrne S, McLean N. Elite athletes: effects of the pressure to be thin. J Sci Med Sport. 2002; 5:80–94.
Article18. Redman LM, Loucks AB. Menstrual disorders in athletes. Sports Med. 2005; 35:747–55.
Article19. Kelsey JL, Bachrach LK, Procter-Gray E, Nieves J, Greendale GA, Sowers M, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc. 2007; 39:1457–63.
Article20. Bolin D, Kemper A, Brolinson PG. Current concepts in the evaluation and management of stress fractures. Curr Sports Med Rep. 2005; 4:295–300.
Article21. Bonci CM, Bonci LJ, Granger LR, Johnson CL, Malina RM, Milne LW, et al. National Athletic Trainers' Association position statement: preventing, detecting, and managing disordered eating in athletes. J Athl Train. 2008; 43:80–108.
Article22. Loucks AB, Nattiv A. Essay: the female athlete triad. Lancet. 2005; 366:S49–50.
Article23. Martinsen M, Sundgot-Borgen J. Higher prevalence of eating disorders among adolescent elite athletes than controls. Med Sci Sports Exerc. 2013; 45:1188–97.
Article24. Smolak L, Murnen SK, Ruble AE. Female athletes and eating problems: a metaanalysis. Int J Eat Disord. 2000; 27:371–80.
Article25. Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. 2004; 14:25–32.
Article26. Beals KA, Meyer NL. Female Athlete Triad update. Clin Sports Med. 2007; 26:69–89.
Article27. Baxter-Jones AD, Helms P, Baines-Preece J, Preece M. Menarche in intensively trained gymnasts, swimmers and tennis players. Ann Hum Biol. 1994; 21:407–15.
Article28. De Souza MJ, Toombs RJ, Scheid JL O'Donnell E, Weat SL, Willams NI. High prevalence of subtle and severe menstrual disturbances in exercising women: confirmation using daily hormone measures. Hum Reprod. 2010; 25:491–503.
Article29. Practice Committee of the American Society for Reproductive Medicine. Current evaluation of amenorrhea. Fertil Steril. 2004; 82:S33–9.30. Carlberg KA, Buckman MT, Peake GT, Riedesel ML. A survey of menstrual function in athletes. Eur J Appl Physiol. 1983; 51:211–22.
Article31. Legro RS, Lin HM, Demers LM, Lloyd T. Rapid maturation of the reproductive axis during perimenarche independent of body composition. J Clin Endocrinol Metab. 2000; 85:1021–5.
Article32. Di Cagno A, Marchetti M, Battaglia C, Giombini A, Calcagno G, Fiorilli G, et al. Is menstrual delay a serious problem for elite rhythmic gymnasts? J Sports Med Phys Fitness. 2012; 52:647–53.33. Beals KA, Manore MM. Disorders of the female athlete triad among collegiate athletes. Int J Sport Nutr Exerc Metab. 2002; 12:281–93.
Article34. Chumlea WC, Schubert CM, Roche AF, Kulin HE, Lee PA, Himes JH, et al. Age at menarche and racial comparisons in US girls. Pediatrics. 2003; 111:110–3.
Article35. Nichols JF, Rauh MJ, Lawson MJ, Ji M, Barkai HS. Prevalence of the female athlete triad syndrome among high school athletes. Arch Pediatr Adolesc Med. 2006; 160:137–42.
Article36. Sanborn CF, Martin BJ, Wagner WW Jr. Is athletic amenorrhea specific to runners? Am J Obstet Gynecol. 1982; 143:859–61.
Article37. Williams NI, Helmreich DL, Parfitt DB, Caston-Balderrama A, Cameron JL. Evidence for a causal role of low energy availability in the induction of menstrual cycle disturbances during strenuous exercise training. J Clin Endocrinol Metab. 2001; 86:5184–93.
Article38. Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. J Clin Endocrinol Metab. 2003; 88:297–311.
Article39. Misra M. Effects of hypogonadism on bone metabolism in female adolescents and young adults. Nat Rev Endocrinol. 2012; 8:395–404.
Article40. De Souza MJ, Williams NI. Beyond hypoestrogenism in amenorrheic athletes: energy deficiency as a contributing factor for bone loss. Curr Sports Med Rep. 2005; 4:38–44.41. Shapses SA, Heymsfield SB, Ricci TA, et al. Voluntary weight reduction increases bone turnover and loss. In Burckhardt P., Dawson-Hughes B, Heaney RB(eds) Nutritional Aspects of Osteoporosis. New York, NY: Springer-Verlag, 1998, pp.180–4.42. Grinspoon SK, Baum HB, Kim V, Coggins C, Klibanski A. Decreased bone formation and increased mineral dissolution during acute fasting in young women. J Clin Endocrinol Metab. 1995; 80:3628–33.
Article43. Ihle R, Loucks AB. Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res. 2004; 19:1231–40.
Article44. Andersen RE, Wadden TA, Herzog RJ. Changes in bone mineral content in obese dieting women. Metabolism. 1997; 46:857–61.
Article45. Compston JE, Laskey MA, Croucher PI, Coxon A, Kreitzman S. Effect of diet-induced weight loss on total body bone mass. Clin Sci (Lond). 1992; 82:429–32.46. Lloyd T., Myers C., Buchanan J.R., Demers LM. Collegiate women athletes with irregular menses during adolescence have decreased bone density. Obstet Gynecol. 1988; 72:639–42.47. Drinkwater BL, Bruemner B, Chesnut CH III. Menstrual history as a determinant of current bone density in young athletes. JAMA. 1990; 263:545–8.
Article48. Nattiv A, Puffer JC, Casper J, Dorey F, Kabo JM, Hame S, et al. Stress fracture risk factors, incidence and distribution: a 3-year prospective study in collegiate runners. Med Sci Sports Exerc. 2000; 32:S347.49. Ackerman KE, Nazem T, Chapko D, Russell M, Mendes N, Taylor AP, et al. Bone microarchitecture is impaired in adolescent amenorrheic athletes compared with eumenorrheic athletes and nonathletic controls. J Clin Endocrinol Metab. 2011; 96:3123–33.
Article50. Bennell KL, Malcolm SA, Thomas SA, Reid SJ, Brukner PD, Ebeling PR, et al. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996; 24:810–8.51. Bailey DA, Martin AD, McKay HA, Whiting S. Mirwald R. Calcium accretion in girls and boys during puberty: a longitudinal analysis. J Bone Miner Res. 2000; 15:2245–50.52. Yurth EF. Female athlete triad. West J Med. 1995; 162:149–50.53. Compston JE, McConachie C, Stott C, Hannon RA, Kaptoge S, Debiram I, et al. Changes in bone mineral density, body composition and biochemical markers of bone turnover during weight gain in adolescents with severe anorexia nervosa: a 1-year prospective study. Osteoporos Int. 2006; 17:77–84.
Article54. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007; 39:1867–82.55. Cobb KL, Bachrach LK, Greendale G, Marcus R, Neer RM, Nieves J, et al. Disordered eating, menstrual irregularity, and bone mineral density in female runners. Med Sci Sports Exerc. 2002; 35:711–9.
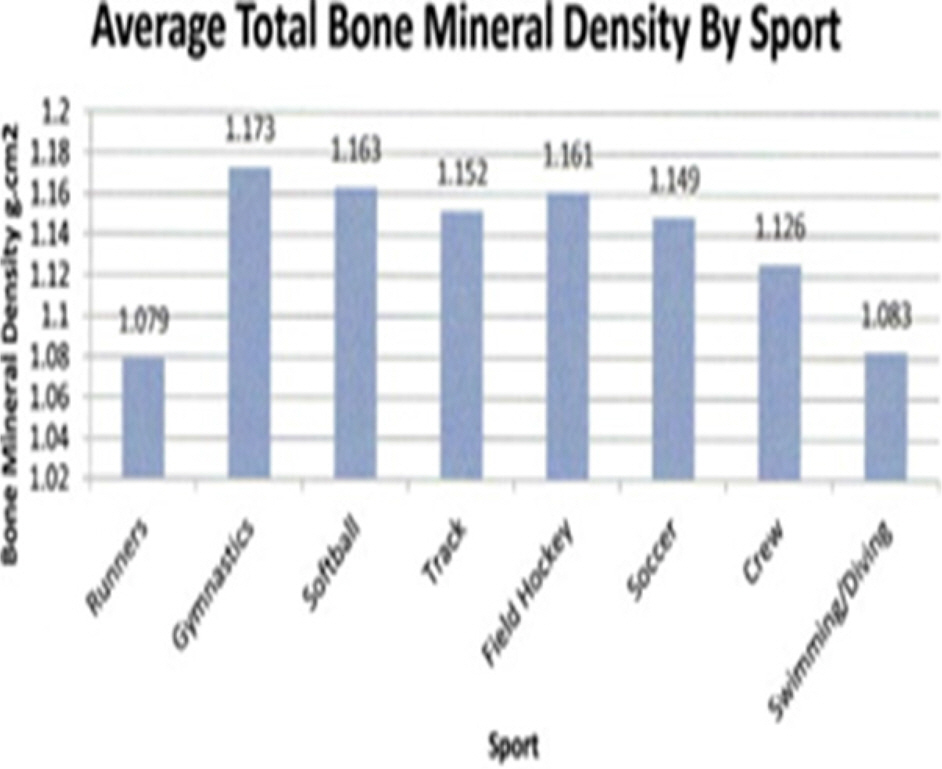
Article56. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine.Bone mineral density in collegiate female athletes: comparisons among sports. J Athletic Train. 2007; 42:403–8.57. Torstveit MK, Sundgot-Borgen J. The female athlete triad: are elite athletes at increased risk? Med Sci Sports Exerc. 2005; 37:184–93.
Article58. Mendelsohn FA, Warren MP. Anorexia, bulimia, and the female athlete triad: evaluation and management. J Clin Endocrinol Metab. 2010; 39:155–67.
Article59. Deimel JF, Dunlap BJ. The female athlete triad. Clin Sports Med. 2012; 31:247–54.
Article60. IOC Medical Commission Working Group Women in Sports. Position Stand on Female Athlete Triad. 2005. INTER REF. http://www.olympic.org/Documents/Reports/EN/en_report_917.pdf. Accessed July 29. 2013.61. American Dietetic Association; Dietitians of Canada; American College of Sports Medicine. Rodriguez NR, Di Marco NM, Langley S. American College of Sports Medicine position stand. Nutrition and athletic performance. Med Sci Sports Exerc. 2009; 41:709–31.62. National Research Council, Subcommittee on the Tenth Edition of the RDAs. Recommended Dietary Allowances. 10th ed.Washington, DC: National Academy Press;1989.63. Economos CD, Bortz SS, Nelson ME. Nutritional practices of elite athletes: practical recommendations. Sports Med. 1993; 16:381–99.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors and Assessment of Low Bone Mass in the Young Adult Female
- Low Back pain in Young Athletes: Epidemilogic Study of Risk Factors
- Bone Mineral Densities in Ballerinas, Korean Traditional Dancers and Athletes
- Management of Ulnar Collateral Ligament Injuries in Overhead Athletes
- A study on radiological evaluation of the lung volumes in Korean athletes