Brain Tumor Res Treat.
2015 Apr;3(1):34-38. 10.14791/btrt.2015.3.1.34.
Primary Diffuse Leptomeningeal Gliosarcomatosis
- Affiliations
-
- 1Department of Neurosurgery, Yonsei University Health System, Seoul, Korea. changjh@yuhs.ac
- 2Brain Tumor Center, Yonsei University Health System, Seoul, Korea.
- 3Department of Pathology, Yonsei University Health System, Seoul, Korea.
- 4Brain Research Institute, Yonsei University Health System, Seoul, Korea.
- KMID: 1882008
- DOI: http://doi.org/10.14791/btrt.2015.3.1.34
Abstract
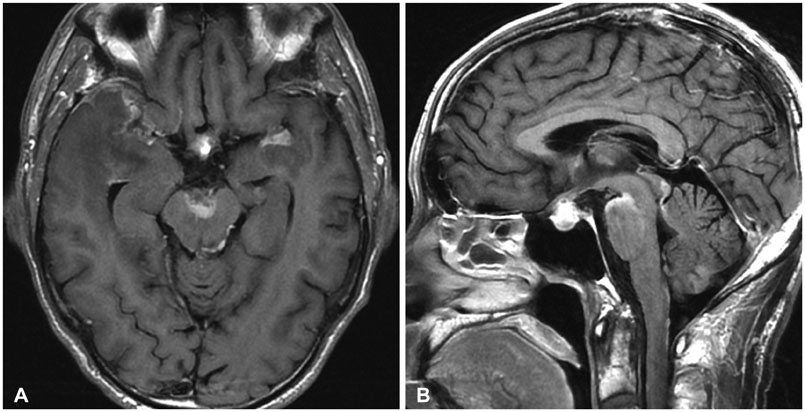
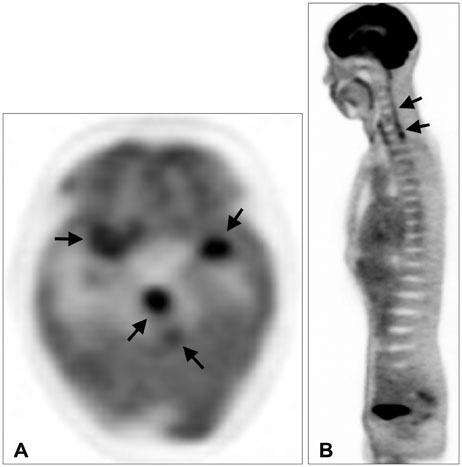
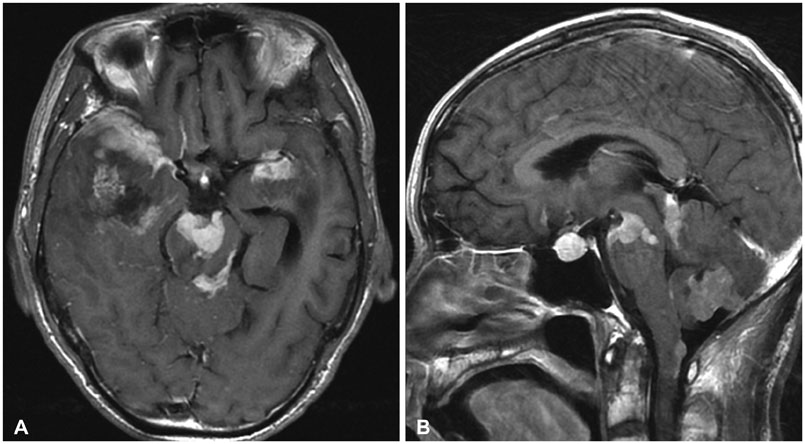
- Primary diffuse leptomeningeal gliomatosis (PDLG) is a rare condition with a fatal outcome, characterized by diffuse infiltration of the leptomeninges by neoplastic glial cells without evidence of primary tumor in the brain or spinal cord parenchyma. In particular, PDLG histologically diagnosed as gliosarcoma is extremely rare, with only 2 cases reported to date. We report a case of primary diffuse leptomeningeal gliosarcomatosis. A 68-year-old man presented with fever, chilling, headache, and a brief episode of mental deterioration. Initial T1-weighted post-contrast brain magnetic resonance imaging (MRI) showed diffuse leptomeningeal enhancement without a definite intraparenchymal lesion. Based on clinical and imaging findings, antiviral treatment was initiated. Despite the treatment, the patient's neurologic symptoms and mental status progressively deteriorated and follow-up MRI showed rapid progression of the disease. A meningeal biopsy revealed gliosarcoma and was conclusive for the diagnosis of primary diffuse leptomeningeal gliosarcomatosis. We suggest the inclusion of PDLG in the potential differential diagnosis of patients who present with nonspecific neurologic symptoms in the presence of leptomeningeal involvement on MRI.
MeSH Terms
Figure
Reference
-
1. Yamasaki K, Yokogami K, Ohta H, et al. A case of primary diffuse leptomeningeal gliomatosis. Brain Tumor Pathol. 2014; 31:177–181.
Article2. Debono B, Derrey S, Rabehenoina C, Proust F, Freger P, Laquerrière A. Primary diffuse multinodular leptomeningeal gliomatosis: case report and review of the literature. Surg Neurol. 2006; 65:273–282. discussion 282.3. Watanabe Y, Hotta T, Yoshioka H, Itou Y, Taniyama K, Sugiyama K. Primary diffuse leptomeningeal gliosarcomatosis. J Neurooncol. 2008; 86:207–210.
Article4. Dimou J, Tsui A, Maartens NF, King JA. Primary diffuse leptomeningeal gliosarcomatosis with a sphenoid/sellar mass: confirmation of the ectopic glial tissue theory? J Clin Neurosci. 2011; 18:702–704.
Article5. Miller CR, Perry A. Glioblastoma. Arch Pathol Lab Med. 2007; 131:397–406.
Article6. Kim YG, Kim EH, Kim SH, Chang JH. Solitary primary leptomeningeal glioma: case report. Brain Tumor Res Treat. 2013; 1:36–41.
Article7. Keith T, Llewellyn R, Harvie M, Roncaroli F, Weatherall MW. A report of the natural history of leptomeningeal gliomatosis. J Clin Neurosci. 2011; 18:582–585.
Article8. Cooper IS, Kernohan JW. Heterotopic glial nests in the subarachnoid space; histopathologic characteristics, mode of origin and relation to meningeal gliomas. J Neuropathol Exp Neurol. 1951; 10:16–29.
Article9. Ruiz-Ares G, Collantes-Bellido E, Rodriguez de Rivera F, et al. Primary diffuse leptomeningeal gliomatosis mimicking meningeal tuberculosis. Neurologist. 2011; 17:160–163.
Article10. Ko MW, Turkeltaub PE, Lee EB, et al. Primary diffuse leptomeningeal gliomatosis mimicking a chronic inflammatory meningitis. J Neurol Sci. 2009; 278:127–131.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Diffuse Leptomeningeal Gliomatosis: Report of a Case Presenting with Chronic Meningitis
- Breast Cancer with Leptomeningeal Metastasis
- Solitary Primary Leptomeningeal Glioma: Case Report
- Primary Leptomeningeal Malignant Melanoma
- Primary Leptomeningeal Glioblastomatosis Detected in Cerebrospinal Fluid Cytology: A Case Report