Tuberc Respir Dis.
2009 May;66(5):349-357. 10.4046/trd.2009.66.5.349.
A Public-Private Collaboration Model for Treatment Intervention to Improve Outcomes in Patients with Tuberculosis in the Private Sector
- Affiliations
-
- 1Korean Institute of Tuberculosis, Korean National Tuberculosis Association, Seoul, Korea. wjlew@hanmail.net
- 2International Union Against Tuberculosis and Lung Disease, Paris, France.
- 3Health Promotion Bureau, Ministry of Health and Welfare, Seoul, Korea.
- 4School of Public Health, Seoul National University, Seoul, Korea.
- KMID: 1846397
- DOI: http://doi.org/10.4046/trd.2009.66.5.349
Abstract
-
BACKGROUND: The treatment success rates in patients with tuberculosis are known to be lower in the private sector compared to the public sector. To improve treatment outcomes in the private sector we developed a public-private collaboration model for strengthening health education and case holding activities with public health nursing in the private sector.
METHODS
We performed a prospective cohort study in new smear positive pulmonary tuberculosis patients treated at private hospitals, selected by non-randomization, with an intervention consisting of health education and case holding activities by specially trained public health nurses (intervention group) results were compared with cases treated without the intervention (conventional group). Physicians were asked to treat both groups routinely. The treatment outcomes of patients under treatment by the National Tuberculosis Programme were also analyzed for comparison.
RESULTS
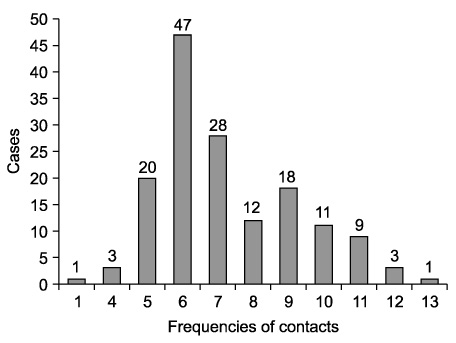
There were 172 cases each in the intervention and conventional groups. The mean age was 48.9+/-19.0 and 48.2+/-19.7 in the respective groups (p=0.66). The PHN interacted with the cases in the intervention group by initial face to face interview and telephone calls an average of 7.1+/-9.2 times during the initial six months. The intervention group showed a significantly higher treatment success rate, 91.6%, (Rate Ratio [RR]; 1.23, 95% Confidence Interval [CI]; 1.12~1.36), lower default, 3.6%, (RR; 0.31, 95% CI; 0.13~0.75) and transfer-out rate, 3.0%, (RR; 0.32, 95% CI; 0.12~0.86) than the conventional group where they were: 75.0%, 11.6%, 9.3%, respectively. The success rate was even higher than the rate (80.5%) of 1,027 cases treated in health centers (RR; 1.11, 95% CI; 1.05~1.17). Of the completed cases in the intervention group, 82.2% regarded the role of the public health nurse as very helpful.
CONCLUSION
The treatment success rate, of tuberculosis patients in the private sector, was significantly improved by an intervention using a public-private collaboration model.
MeSH Terms
Figure
Cited by 1 articles
-
Social and Clinical Characteristics of Immigrants with Tuberculosis in South Korea
Gee Ho Min, Young Kim, Jong Seok Lee, Jee Youn Oh, Gyu Young Hur, Young Seok Lee, Kyung Hoon Min, Sung Yong Lee, Je Hyeong Kim, Chol Shin, Seung Heon Lee
Yonsei Med J. 2017;58(3):592-597. doi: 10.3349/ymj.2017.58.3.592.
Reference
-
1. Hong YP, Kim SJ, Lew WJ, Lee SH, Lee EK. Cohort analyses of the treatment of smear-positive pulmonary tuberculosis patients under programme conditions in Korea, 1983-1994. Int J Tuberc Lung Dis. 1998. 2:365–371.2. Jin BW, Jang DJ. An analysis of tuberculosis patient management in private sector (in Korean). Tuberc Respir Dis. 1990. 37:399–406.3. Hong YP, Kim SJ, Lee EG, Lew WJ, Bai JY. Treatment of bacillary pulmonary tuberculosis at the chest clinics in the private sector in Korea, 1993. Int J Tuberc Lung Dis. 1999. 3:695–702.4. Ministry of Health and Welfare. Korean National Tuberculosis Association. Report on the 7th tuberculosis prevalence survey in Korea. 1996. Seoul: Korean National Tuberculosis Association.5. Korean National Institute of Health. Korean Institute of Tuberculosis. Annual report on the notified tuberculosis patients in Korea: based on Korean Tuberculosis Surveillance System. 2002. Seoul: Korean Institute of Tuberculosis.6. Korean National Institute of Health. Korean Institute of Tuberculosis. Annual report on the notified tuberculosis patients in Korea: based on Korean Tuberculosis Surveillance System. 2003. Seoul: Korean Institute of Tuberculosis.7. World Health Organization. Treatment of tuberculosis: guidelines for national tuberculosis, WHO/CDS/TB 2003.313. 2003. Geneva: WHO.8. Fox W. General considerations in the choice and management of regimens of chemotherapy for pulmonary tuberculosis. Bull Int Union Tuberc. 1972. 47:49–67.9. Horne NW, Ross JD. Modern drug treatment of tuberculosis. 1990. 7th ed. London: The Chest, Heart and Stroke Association;43–45.10. Leff DR, Leff AR. Tuberculosis control policies in major metropolitan health departments in the United States: VI. standard practice in 1996. Am J Respir Crit Care Med. 1997. 156:1487–1494.11. Ormerod LP, Bentley C. The management of pulmonary tuberculosis notified in England and Wales in 1993. J R Coll Physicians Lond. 1997. 31:662–665.12. Simpson AJ, Watt B, Heald SH, Sudlow MF, Leitch AG. The management of pulmonary tuberculosis in adults notified in Scotland in 1993. Respir Med. 1998. 92:1289–1294.13. Rothe TB, Karrer W. Short-course therapy of pulmonary tuberculosis: doctor's compliance. Tuber Lung Dis. 1996. 77:93–97.14. Sumartojo EM, Geiter LJ, Miller B, Hale BE. Can physicians treat tuberculosis?: report on a national survey of physician practices. Am J Public Health. 1997. 87:2008–2011.15. Ollé-Goig JE, Cullity JE, Vargas R. A survey of prescribing patterns for tuberculosis treatment amongst doctors in a Bolivian city. Int J Tuberc Lung Dis. 1999. 3:74–78.16. Singla N, Sharma PP, Singla R, Jain RC. Survey of knowledge, attitudes and practices for tuberculosis among general practitioners in Delhi, India. Int J Tuberc Lung Dis. 1998. 2:384–389.17. Bloch AB, Cauthen GM, Simone PM, Kelly GD, Dansbury KG, Castro KG. Completion of tuberculosis therapy for patients reported in the United States in 1993. Int J Tuberc Lung Dis. 1999. 3:273–280.18. Hong YP, Kwon DW, Kim SJ, Chang SC, Kang MK, Lee EP, et al. Survey of knowledge, attitudes and practices for tuberculosis among general practitioners. Tuber Lung Dis. 1995. 76:431–435.19. Vyas RM, Small PM, DeRiemer K. The private-public divide: impact of conflicting perceptions between the private and public health care sectors in India. Int J Tuberc Lung Dis. 2003. 7:543–549.20. Uplekar M, Pathania V, Raviglione M. Private practitioners and public health: weak links in tuberculosis control. Lancet. 2001. 358:912–916.21. Weil DE. Advancing tuberculosis control within reforming health systems. Int J Tuberc Lung Dis. 2000. 4:597–605.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Tuberculosis in Korea
- Treatment of Tuberculosis Patients in the Private Sector in Korea
- Increasing the Treatment Success Rate of Tuberculosis in a Private Hospital through Public-Private Mix (PPM) Project
- Clinical Characteristics and Treatment Outcomes of Patients with Pulmonary Tuberculosis at a Private General Hospital
- The Clinical Characteristics, Diagnosis, Treatment, and Outcomes of Patients with Tuberculosis at a Private University Hospital in Korea