Anat Cell Biol.
2015 Jun;48(2):130-137. 10.5115/acb.2015.48.2.130.
Topography of human ankle joint: focused on posterior tibial artery and tibial nerve
- Affiliations
-
- 1Department of Nursing, College of Nursing, Keimyung University, Daegu, Korea.
- 2Department of Anatomy, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Anatomy, Chung-Ang University College of Medicine, Seoul, Korea. monami@cau.ac.kr
- KMID: 1845281
- DOI: http://doi.org/10.5115/acb.2015.48.2.130
Abstract
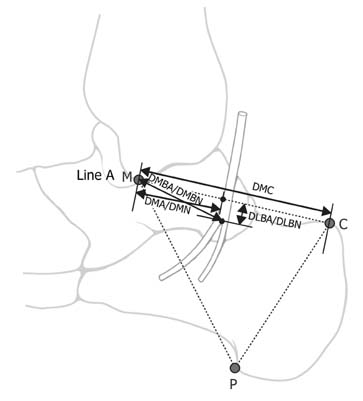
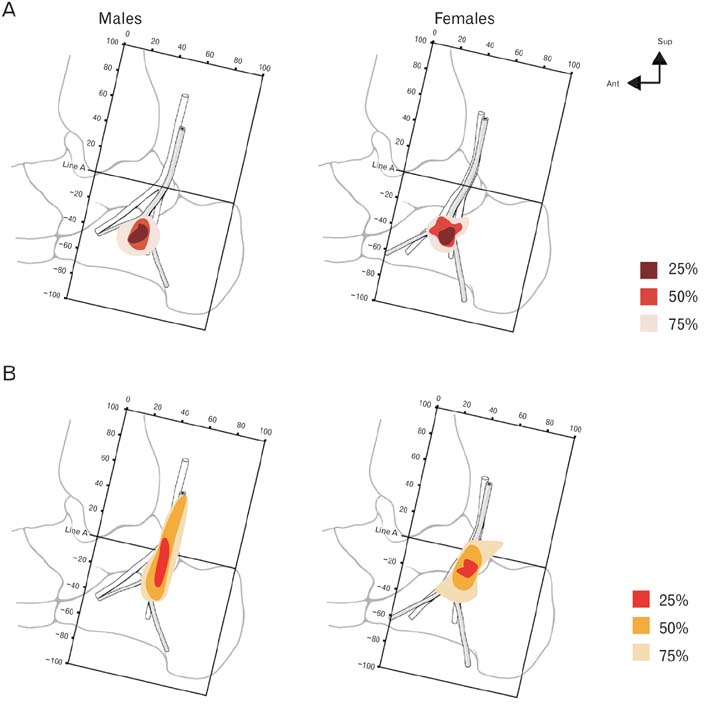
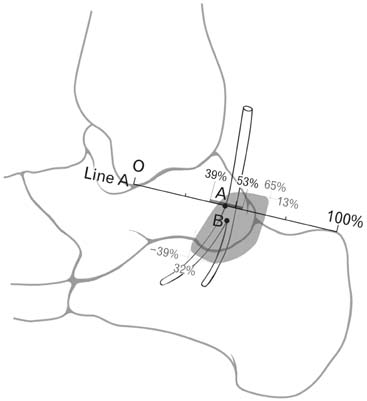
- Most of foot pain occurs by the entrapment of the tibial nerve and its branches. Some studies have reported the location of the tibial nerve; however, textbooks and researches have not described the posterior tibial artery and the relationship between the tibal nerve and the posterior tibial artery in detail. The purpose of this study was to analyze the location of neurovascular structures and bifurcations of the nerve and artery in the ankle region based on the anatomical landmarks. Ninety feet of embalmed human cadavers were examined. All measurements were evaluated based on a reference line. Neurovascular structures were classified based on the relationship between the tibial nerve and the posterior tibial artery. The bifurcation of arteries and nerves were expressed by X- and Y-coordinates. Based on the reference line, 9 measurements were examined. The most common type I (55.6%), was the posterior tibial artery located medial to the tibial nerve. Neurovascular structures were located less than 50% of the distance between M and C from M at the reference line. The bifurcation of the posterior tibial artery was 41% in X-coordinate, -38% in Y-coordinate, and that of the tibial nerve was 48%, and -10%, respectively. Thirteen measurements and classification showed statistically significant differences between both sexes (P<0.05). It is determined the average position of neurovascular structures in the human ankle region and recorded the differences between the sexes and amongst the populations. These results would be helpful for the diagnosis and treatment of foot pain.
MeSH Terms
Figure
Cited by 2 articles
-
Anatomical study and branching point of neurovascular structures at the medial side of the ankle
Chanatporn Inthasan, Tanawat Vaseenon, Pasuk Mahakkanukrauh
Anat Cell Biol. 2020;53(4):422-434. doi: 10.5115/acb.20.087.Anatomical variations of the tibial nerve and their clinical correlation
Anita Soraya Soetoko, Dina Fatmawati
Anat Cell Biol. 2023;56(4):415-420. doi: 10.5115/acb.23.065.
Reference
-
1. National Health Insurance Service. To difficult walk 'Plantar fasciitis', female patients increased three times over the past five years [Internet]. Seoul: National Health Insurance Service;2013. cited 2015 Feb 1. Available from: http://www.nhis.or.kr/bbs7/boards/B0039/3003.2. Aldridge T. Diagnosing heel pain in adults. Am Fam Physician. 2004; 70:332–338.3. Antoniadis G, Scheglmann K. Posterior tarsal tunnel syndrome: diagnosis and treatment. Dtsch Arztebl Int. 2008; 105:776–781.4. Mahadevon V. Pelvic girdle and lower limb. In : Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. Madrid: Elsevier;2008. p. 1425–1427.5. Erickson SJ, Quinn SF, Kneeland JB, Smith JW, Johnson JE, Carrera GF, Shereff MJ, Hyde JS, Jesmanowicz A. MR imaging of the tarsal tunnel and related spaces: normal and abnormal findings with anatomic correlation. AJR Am J Roentgenol. 1990; 155:323–328.6. Franson J, Baravarian B. Tarsal tunnel syndrome: a compression neuropathy involving four distinct tunnels. Clin Podiatr Med Surg. 2006; 23:597–609.7. Lau JT, Daniels TR. Tarsal tunnel syndrome: a review of the literature. Foot Ankle Int. 1999; 20:201–209.8. Radin EL. Tarsal tunnel syndrome. Clin Orthop Relat Res. 1983; (181):167–170.9. Havel PE, Ebraheim NA, Clark SE, Jackson WT, DiDio L. Tibial nerve branching in the tarsal tunnel. Foot Ankle. 1988; 9:117–119.10. Heimkes B, Posel P, Stotz S, Wolf K. The proximal and distal tarsal tunnel syndromes. An anatomical study. Int Orthop. 1987; 11:193–196.11. Lam SJ. Tarsal tunnel syndrome. J Bone Joint Surg Br. 1967; 49:87–92.12. Lamm BM, Paley D, Testani M, Herzenberg JE. Tarsal tunnel decompression in leg lengthening and deformity correction of the foot and ankle. J Foot Ankle Surg. 2007; 46:201–206.13. Bareither DJ, Genau JM, Massaro JC. Variation in the division of the tibial nerve: application to nerve blocks. J Foot Surg. 1990; 29:581–583.14. Dellon AL, Mackinnon SE. Tibial nerve branching in the tarsal tunnel. Arch Neurol. 1984; 41:645–646.15. Williams EH, Williams CG, Rosson GD, Dellon LA. Anatomic site for proximal tibial nerve compression: a cadaver study. Ann Plast Surg. 2009; 62:322–325.16. Gamie Z, Donnelly L, Tsiridis E. The "safe zone" in medial percutaneous calcaneal pin placement. Clin Anat. 2009; 22:523–529.17. Govsa F, Bilge O, Ozer MA. Variations in the origin of the medial and inferior calcaneal nerves. Arch Orthop Trauma Surg. 2006; 126:6–14.18. Andreasen Struijk LN, Birn H, Teglbjaerg PS, Haase J, Struijk JJ. Size and separability of the calcaneal and the medial and lateral plantar nerves in the distal tibial nerve. Anat Sci Int. 2010; 85:13–22.19. Davis TJ, Schon LC. Branches of the tibial nerve: anatomic variations. Foot Ankle Int. 1995; 16:21–29.20. Rondhuis JJ, Huson A. The first branch of the lateral plantar nerve and heel pain. Acta Morphol Neerl Scand. 1986; 24:269–279.21. Gould JS. Recurrent tarsal tunnel syndrome. Foot Ankle Clin. 2014; 19:451–467.22. Kim K, Isu T, Morimoto D, Sasamori T, Sugawara A, Chiba Y, Isobe M, Kobayashi S, Morita A. Neurovascular bundle decompression without excessive dissection for tarsal tunnel syndrome. Neurol Med Chir (Tokyo). 2014; 54:901–906.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tarsal Tunnel Syndrome secondary to the Varicosis of Posterior Tibial Vein (Two Cases Report)
- Low Tibial Osteotomy
- Checkrein Deformity by Incarcerated Posterior Tibial Tendon and Displaced Flexor Hallucis Longus Tendon following Ankle Dislocation: A Case Report
- The Intraneural Ganglion of the Posterior Tibial Nerve and Medial Plantar Nerve
- Anatomical variations of the tibial nerve and their clinical correlation