J Korean Soc Spine Surg.
2014 Mar;21(1):1-7. 10.4184/jkss.2014.21.1.1.
Does Preoperative Cervical Sagittal Alignment And Range of Motion Affect Adjacent Segment Degeneration After Anterior Arthrodesis In Degenerative Cervical Spinal Disorders?: Midterm Follow up Study
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University Medical School, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Jeonju, Korea. osdr2815@naver.com
- KMID: 1840410
- DOI: http://doi.org/10.4184/jkss.2014.21.1.1
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
The purpose of this study was to investigate whether preoperative sagittal alignment and range of motion (ROM) affect adjacent segment degeneration (ASD) and disease after anterior arthrodesis in degenerative cervical spinal disorders. Summary of Literature Review:There is no study about the relationship between preoperative ROM and sagittal alignment and the development of ASD yet.
MATERIALS AND METHODS
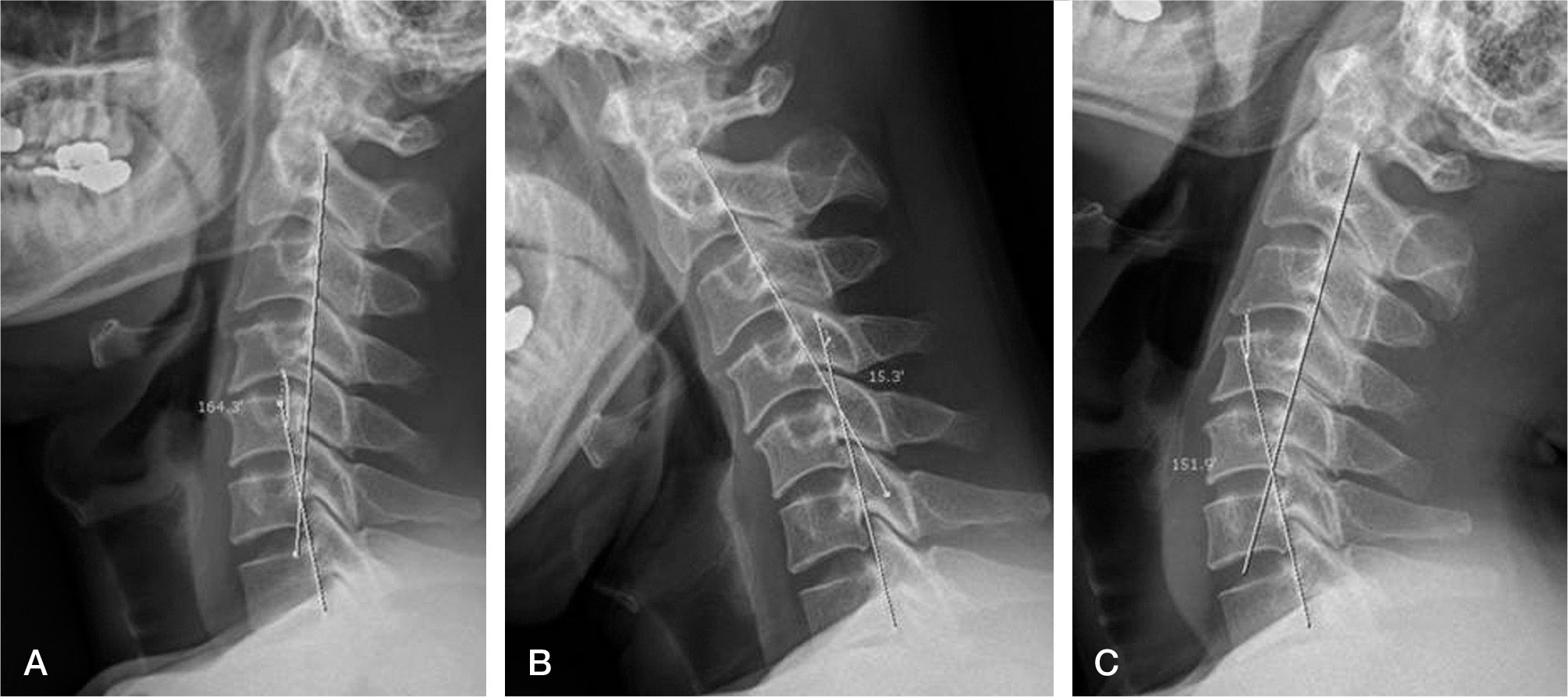
We took a retrospective approach to study 136 patients who underwent an anterior arthodesis for less than 2 segments with PEEK cage and plate construct method for degenerative cervical diseases and who have a minimum of 3 years of follow-up. We analyzed ASD and cervical ROM, such as less than 40degrees(group A) and more than 40degrees(group B) and sagittal alignment, such as lordosis or kyphosis with less than 10degrees(group a), 10degrees~30degrees(group b) and more than 30degrees(group c). Adjacent segment degeneration was graded according to Park's classification and Hillibrand method.
RESULTS
There was no statistically significant difference between group A(1.35+/-0.48) and group B (1.44+/-0.50) in the correlation between the cervical ROM and the variation of disc height(p=0.07). Concerning the relationship between the ROM and osteophyte formation on adjacent segment, no statistically significant difference has been found between group A(1.64+/-0.88) and group B(1.43+/-0.67) (p=0.06). The disc height change at the final follow up after cervical sagittal alignment showed no statistically significant difference among the groups: Group A presented with 1.53+/-0.50, group B with 1.30+/-0.46 and group C with 1.40+/-0.50.(p=0.08) Regarding sagittal alignment and osteophyte change, there was no statistically significant difference among the groups as group A showed an average of 1.33+/-0.48, group Ban average of 1.56+/-0.88 and group Can average of 1.60+/-0.82(p=0.07).
CONCLUSION
Although the preoperative sagittal alignment and ROM did not significantly affect adjacent segment degeneration and diseases in a mid-term follow-up evaluation after anterior arthrodesis with PEEK cage and plate in degenerative cervical spinal disorders, we think a future study is required with a sufficient number of patients and a long term follow-up because there were borderline statistical significances shown in the present study.
Keyword
MeSH Terms
Figure
Reference
-
1. SMITH GW, ROBINSON RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40:607–24.
Article2. Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondyloticmyeloradiculopathy. Spine (Phila Pa 1976). 1993; 18:2167–73.3. Goffin J, van Loon J, Van Calenbergh F, Plets C. Longterm results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995; 8:500–8.
Article4. Kaplan EL, Meier P. Nonparametric estimation from in-complete observations. J Am Statist Assoc. 1958; 53:457–81.
Article5. McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A longterm followup study. J Bone Joint Surg Am. 1994; 76:1606–16.
Article6. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519–28.
Article7. Dö hler JR, Kahn MR, Hughes SP. Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Arch Orthop Trauma Surg. 1985; 104:247–50.8. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphoticma-lalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001; 10:320–4.9. Song KJ, Johnson JS, Choi BR, Wang JC, Lee KB. Anterior fusion alone compared with combined anterior and posterior fusion for the treatment of degenerative cervical kyphosis. J Bone Joint Surg Br. 2010; 92:1548–52.
Article10. Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005; 87:558–63.
Article11. Rhin JA, Lawrence J, Gates C, Harris E, Hilibrand AS. Adjacent segment disease after cervical spine fusion. Instr Course Lect. 2009; 58:747–56.12. Buckwalter JA. Aging and degeneration of the human inte-vertebral disc. Spine (Phila Pa 1976). 1995; 20:1307–14.13. Schwab JS, Diangelo DJ, Foley KT. Motion compension associated with single-level cervical fusion: where does the lost motion go? Spine (Phila Pa 1976). 2006; 31:2439–48.14. Ragab AA, Escarcega AJ, Zdeblick TA. A quantitative analysis of strain at adjacent segment after segmental im-mobilization of the cervical spine. J Spinal Disord Tech. 2006; 19:407–10.15. Maiman DJ, Kumaresan S, Yoganandan N, Pintar FA. Biomechanical effect of anterior cervical spine fusion on adjacent segment. Biomed Mater Eng. 1999; 9:27–38.16. Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007; 7:336–40.
Article17. Rao RD, Wang M, McGrady LM, Perlewitz TJ, David KS. Dose anterior plating of the cervical spine predis-pose to adjacent segment changes? Spine (Phila Pa 1976). 2005; 30:2788–92.18. Goffin J, Geusens E, Vantomme N, et al. Longterm followup after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004; 17:79–85.
Article19. Elsawaf A, Mastronardi L, Roperto R, Bozzao A, Caroli M, Ferrante L. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurg Rev. 2009; 32:215–24.
Article20. Yue WM, Brodner W, Highland TR. Longterm results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11- year radiologic and clinical followup study. Spine (Phila Pa 1976). 2005; 30:2138–44.21. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Longterm followup of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993; 75:1298–307.
Article22. Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine(Phila Pa 1976). 1984; 9:667–71.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Mal-alignment after Anterior Cervical Arthrodesis in Degenerative Cervical Spinal Disorders
- Changes of Adjacent Segment in Anterior Cervical Fusion
- Comparison of Adjacent Segment Degeneration, Cervical Alignment, and Clinical Outcomes after One- and Multilevel Anterior Cervical Discectomy and Fusion
- Radiologic Changes of Operated and Adjacent Segments after Anterior Cervical Microforaminotomy
- Radiologic Comparison of Cervical Athroplasty with Cervical Arthrodesis