Korean J Obstet Gynecol.
2011 Oct;54(10):618-622. 10.5468/KJOG.2011.54.10.618.
Clinical outcomes of 1,041 total laparoscopic hysterectomies: Six years of experience in a single center
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 2Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea. ybkimlh@snubh.org
- KMID: 1836748
- DOI: http://doi.org/10.5468/KJOG.2011.54.10.618
Abstract
OBJECTIVE
To evaluate the association between outcomes of total laparoscopic hysterectomy (TLH) and patient demographic and clinical factors.
METHODS
The present study was performed on a total of 1,041 women who underwent TLH, with or without bilateral/unilateral salpingo-oophorectomy, from May 2003 to December 2008, excluding patients who also underwent other procedures simultaneously, including ovarian cystectomy, colporrhaphy, incontinence surgery, pelvic/para-aortic lymph node dissection, and/or omentectomy. The medical records were reviewed and clinical outcomes were analyzed.
RESULTS
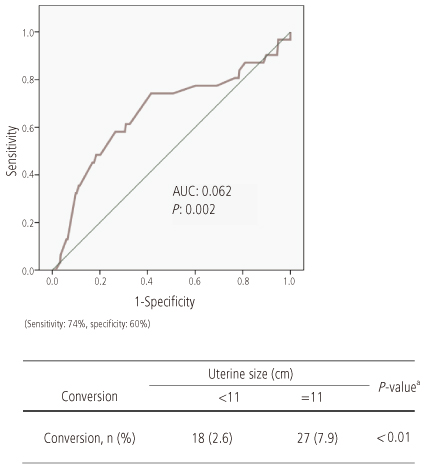
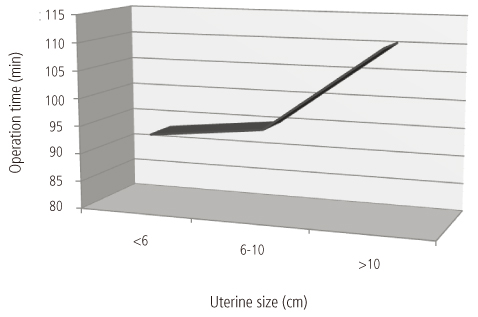
Mean patient age was 46.6 +/- 13.4 years, mean operation time was 103.4 +/- 42.3 minutes, and mean duration of total hospital stay was 5.4 +/- 2.9 days. The mean decrease in hemoglobin concentration from before operation to 1 day after surgery was 1.4 +/- 0.9 g/dL, and one patient required an intraoperative transfusion. The main diagnosis was leiomyoma including concomitant adenomyosis (62.2%), followed by adenomyosis (16.0%) and 32 early stage gynecologic malignancies including 20 patients with microinvasive cervical cancer, 10 with endometrial cancer, 1 with borderline ovarian cancer, and 1 with uterine sarcoma. Laparotomy conversion was occurred in 45 patients (4.2%), because of severe pelvic/abdominal adhesion or huge uterine size. Large uterine size was associated with a significantly higher rate of conversion (7.9% vs. 2.6%, P < 0.01), and a significantly longer operation time (110.5 minutes vs. 93.1 minutes vs. 95.3 minutes, P < 0.01). Overall, 6 patients (0.6%) experienced major complications, including two bowel perforations, two ureteral injuries requiring surgical repair, one vaginal evisceration, and one incisional hernia.
CONCLUSION
TLH is a safe and acceptable alternative to standard hysterectomy for various indications, including malignancy.
Keyword
MeSH Terms
Figure
Reference
-
1. Marana R, Busacca M, Zupi E, Garcea N, Paparella P, Catalano GF. Laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy: a prospective, randomized, multicenter study. Am J Obstet Gynecol. 1999. 180:270–275.2. Vessey MP, Villard-Mackintosh L, McPherson K, Coulter A, Yeates D. The epidemiology of hysterectomy: findings in a large cohort study. Br J Obstet Gynaecol. 1992. 99:402–407.3. Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and metaanalysis of randomised controlled trials. BMJ. 2005. 330:1478.4. Raju KS, Auld BJ. A randomised prospective study of laparoscopic vaginal hysterectomy versus abdominal hysterectomy each with bilateral salpingo-oophorectomy. Br J Obstet Gynaecol. 1994. 101:1068–1071.5. Donnez O, Jadoul P, Squifflet J, Donnez J. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG. 2009. 116:492–500.6. Daraï , Soriano D, Kimata P, Laplace C, Lecuru F. Vaginal hysterectomy for enlarged uteri, with or without laparoscopic assistance: randomized study. Obstet Gynecol. 2001. 97:712–716.7. Holub Z, Jabor A, Kliment L, Fischlová D, Wágnerová M. Laparoscopic hysterectomy in obese women: a clinical prospective study. Eur J Obstet Gynecol Reprod Biol. 2001. 98:77–82.8. Elkington NM, Chou D. A review of total laparoscopic hysterectomy: role, techniques and complications. Curr Opin Obstet Gynecol. 2006. 18:380–384.9. Semm K. Endoscopic methods in gastroenterology and gynecology. Completion of diagnostic pelviscopy by endoscopic abdominal surgery. Fortschr Med. 1984. 102:534–537.10. Demco L, Garry R, Johns DA, Kovac SR, Lyons TL, Reich H. Hysterectomy. Panel discussion at the 22nd annual meeting of the American Association of Gynecologic Laparoscopists (AAGL), San Francisco, November 12, 1993. J Am Assoc Gynecol Laparosc. 1994. 1:287–295.11. Reich H. Total laparoscopic hysterectomy: indications, techniques and outcomes. Curr Opin Obstet Gynecol. 2007. 19:337–344.12. Garry R, Fountain J, Mason S, Hawe J, Napp V, Abbott J, et al. The eVALuate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004. 328:129.13. Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2006. (2):CD003677.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid laparoscopic myomectomy: A novel technique
- Total Laparoscopic Hysterectomy using Modified Bae's Uterine Elevator
- Clinical outcomes of hysterectomy for benign diseases in the female genital tract: 6 years’ experience in a single institute
- Total laparoscopic hysterectomy versus da Vinci robotic hysterectomy: is using the robot beneficial?
- Transumbilical single port total laparoscopic hysterectomy