J Korean Soc Radiol.
2015 Jan;72(1):46-56. 10.3348/jksr.2015.72.1.46.
A Single-Center Experience of 2153 Tunneled-Cuffed Catheter Insertions Radiologically Placed via the Internal Jugular Vein: An Evaluation of Technical Success and Complication Rates Relative to Underlying Disease Conditions
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Gwangju, Korea. apleseed@chonnam.ac.kr
- KMID: 1823934
- DOI: http://doi.org/10.3348/jksr.2015.72.1.46
Abstract
- PURPOSE
To evaluate the technical success and complication rates of tunneled-cuffed catheter insertions radiologically placed via the internal jugular vein in patients with different types of underlying diseases.
MATERIALS AND METHODS
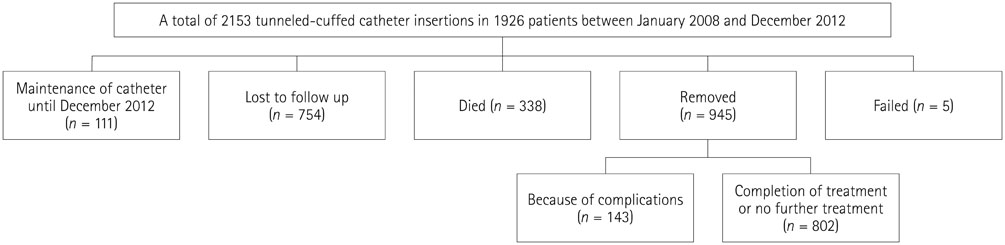
A total of 2153 tunneled-cuffed catheter insertions performed in 1926 patients between January 2008 and December 2012 were retrospectively reviewed. All procedures were conducted using sonography and fluoroscopy. The number of catheter maintenance days, technical success rates, and complication rates were analyzed based on radiologic and medical records.
RESULTS
A total of 204809 catheter maintenance days (mean, 95.35 days; range, 0-1710 days) were recorded. Technical success was achieved in 2148 insertions (99.77%). A total of 185 complications (8.61%, 0.903/1000 catheter days) were observed, including 22 procedure-related complications (1.02%). A total of 143 catheters (6.66%) were removed due to complications. Significant differences in complication rates were observed between patients with or without underlying hematologic diseases (11.65% vs. 7.02%, respectively; p = 0.000). Significant differences in catheter thrombosis were observed between patients in which right-sided or left-sided venous approaches were used (0.81% vs. 2.70%, respectively; p = 0.010).
CONCLUSION
The very high technical success rates and very low procedure-related complication rates indicate insertion of a tunneled-cuffed catheter radiologically placed via the internal jugular vein is safe and effective.
MeSH Terms
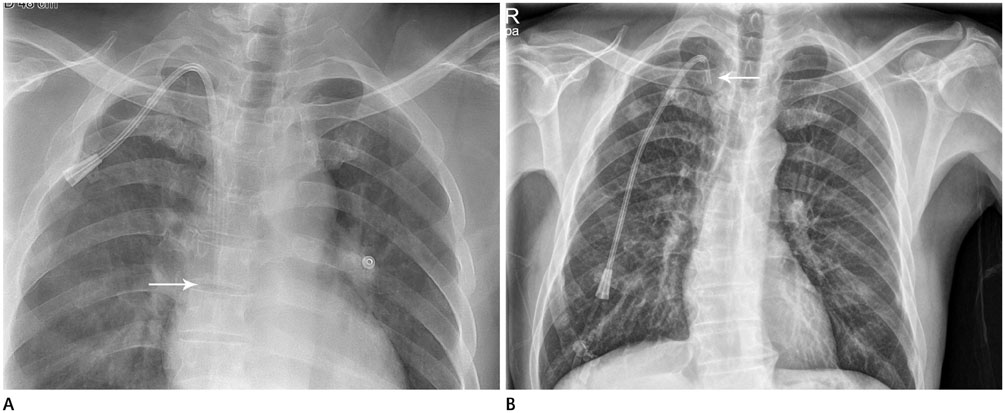
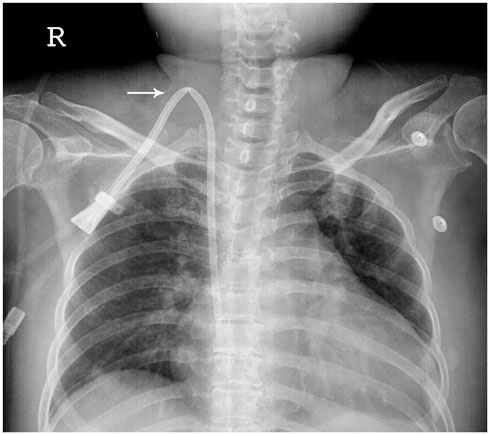
Figure
Reference
-
1. Silberzweig JE, Sacks D, Khorsandi AS, Bakal CW. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for central venous access. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S443–S452.2. Reeves AR, Seshadri R, Trerotola SO. Recent trends in central venous catheter placement: a comparison of interventional radiology with other specialties. J Vasc Interv Radiol. 2001; 12:1211–1214.3. Funaki B. Tunneled central venous catheter insertion. Semin Intervent Radiol. 2008; 25:432–436.4. Cavanna L, Civardi G, Vallisa D, Di Nunzio C, Cappucciati L, Bertè R, et al. Ultrasound-guided central venous catheterization in cancer patients improves the success rate of cannulation and reduces mechanical complications: a prospective observational study of 1,978 consecutive catheteri-zations. World J Surg Oncol. 2010; 8:91.5. Peynircioglu B, Ozkan F, Canyigit M, Pamuk GA, Geyik S, Cil BE, et al. Radiologically placed tunneled internal jugular catheters in the management of chronic hemodialysis and long-term infusion therapies in the pediatric population. J Vasc Interv Radiol. 2007; 18:875–881.6. Trerotola SO, Johnson MS, Harris VJ, Shah H, Ambrosius WT, McKusky MA, et al. Outcome of tunneled hemodialysis catheters placed via the right internal jugular vein by interventional radiologists. Radiology. 1997; 203:489–495.7. Caridi JG, Grundy LS, Ross EA, Prabhu PN, Tonkin JC, Hawkins IF Jr, et al. Interventional radiology placement of twin Tesio catheters for dialysis access: review of 75 patients. J Vasc Interv Radiol. 1999; 10:78–83.8. Koroglu M, Demir M, Koroglu BK, Sezer MT, Akhan O, Yildiz H, et al. Percutaneous placement of central venous catheters: comparing the anatomical landmark method with the radiologically guided technique for central venous catheterization through the internal jugular vein in emergent hemodialysis patients. Acta Radiol. 2006; 47:43–47.9. Funaki B. Central venous access: a primer for the diagnostic radiologist. AJR Am J Roentgenol. 2002; 179:309–318.10. Moureau N, Poole S, Murdock MA, Gray SM, Semba CP. Central venous catheters in home infusion care: outcomes analysis in 50,470 patients. J Vasc Interv Radiol. 2002; 13:1009–1016.11. Dariushnia SR, Wallace MJ, Siddiqi NH, Towbin RB, Wojak JC, Kundu S, et al. Quality improvement guidelines for central venous access. J Vasc Interv Radiol. 2010; 21:976–981.12. Mauro MA, Jaques PF. Insertion of long-term hemodialysis catheters by interventional radiologists: the trend continues. Radiology. 1996; 198:316–317.13. Sulek CA, Blas ML, Lobato EB. A randomized study of left versus right internal jugular vein cannulation in adults. J Clin Anesth. 2000; 12:142–145.14. Rose SC, Kinney TB, Bundens WP, Valji K, Roberts AC. Importance of Doppler analysis of transmitted atrial waveforms prior to placement of central venous access catheters. J Vasc Interv Radiol. 1998; 9:927–934.15. Nightingale CE, Norman A, Cunningham D, Young J, Webb A, Filshie J. A prospective analysis of 949 long-term central venous access catheters for ambulatory chemotherapy in patients with gastrointestinal malignancy. Eur J Cancer. 1997; 33:398–403.16. Lee SH, Hahn ST. Comparison of complications between transjugular and axillosubclavian approach for placement of tunneled, central venous catheters in patients with hematological malignancy: a prospective study. Eur Radiol. 2005; 15:1100–1104.17. Galbusera M, Remuzzi G, Boccardo P. Treatment of bleeding in dialysis patients. Semin Dial. 2009; 22:279–286.18. Kerr A, Pathalapati R, Qiuhu S, Baumstein D. Purse-string suture to prevent bleeding after tunneled dialysis catheter insertion. J Vasc Interv Radiol. 2008; 19:1176–1179.19. Obialo CI, Conner AC, Lebon LF. Tunneled hemodialysis catheter survival: comparison of radiologic and surgical implantation. ASAIO J. 2000; 46:771–774.20. Male C, Chait P, Andrew M, Hanna K, Julian J, Mitchell L, et al. Central venous line-related thrombosis in children: association with central venous line location and insertion technique. Blood. 2003; 101:4273–4278.21. Magagnoli M, Masci G, Castagna L, Pedicini V, Poretti D, Morenghi E, et al. Prophylaxis of central venous catheter-related thrombosis with minidose warfarin in patients treated with high-dose chemotherapy and peripheral-blood stem-cell transplantation: retrospective analysis of 228 cancer patients. Am J Hematol. 2006; 81:1–4.22. van Rooden CJ, Rosendaal FR, Barge RM, van Oostayen JA, van der Meer FJ, Meinders AE, et al. Central venous catheter related thrombosis in haematology patients and prediction of risk by screening with Doppler-ultrasound. Br J Haematol. 2003; 123:507–512.23. Fijnheer R, Paijmans B, Verdonck LF, Nieuwenhuis HK, Roest M, Dekker AW. Factor V Leiden in central venous catheter-associated thrombosis. Br J Haematol. 2002; 118:267–270.24. Tesselaar ME, Ouwerkerk J, Nooy MA, Rosendaal FR, Osanto S. Risk factors for catheter-related thrombosis in cancer patients. Eur J Cancer. 2004; 40:2253–2259.25. Wong JK, Sadler DJ, McCarthy M, Saliken JC, So CB, Gray RR. Analysis of early failure of tunneled hemodialysis catheters. AJR Am J Roentgenol. 2002; 179:357–363.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placement of Tunneled Cuffed Hemodialysis Catheters Via Internal Jugular Vein by an Interventional Radiologist and a Vascular Surgeon Together
- Physician-Modified Fenestrated Endovascular Repair for Iatrogenic Innominate Vein Injury
- Cut-down method for perm catheter insertion in patients with completely occluded internal jugular vein
- Outcome of Tunneled Infusion Catheters Inserted via the Right Internal Jugular Vein
- Posterior triangle approach for lateral in-plane technique during hemodialysis catheter insertion via the internal jugular vein