J Korean Soc Radiol.
2014 Aug;71(2):65-68. 10.3348/jksr.2014.71.2.65.
Spontaneous Regression of Focal Nodular Hyperplasia of the Liver after Delivery: A Case Report
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. radmhlee@schmc.ac.kr
- 2Department of Pathology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- KMID: 1819781
- DOI: http://doi.org/10.3348/jksr.2014.71.2.65
Abstract
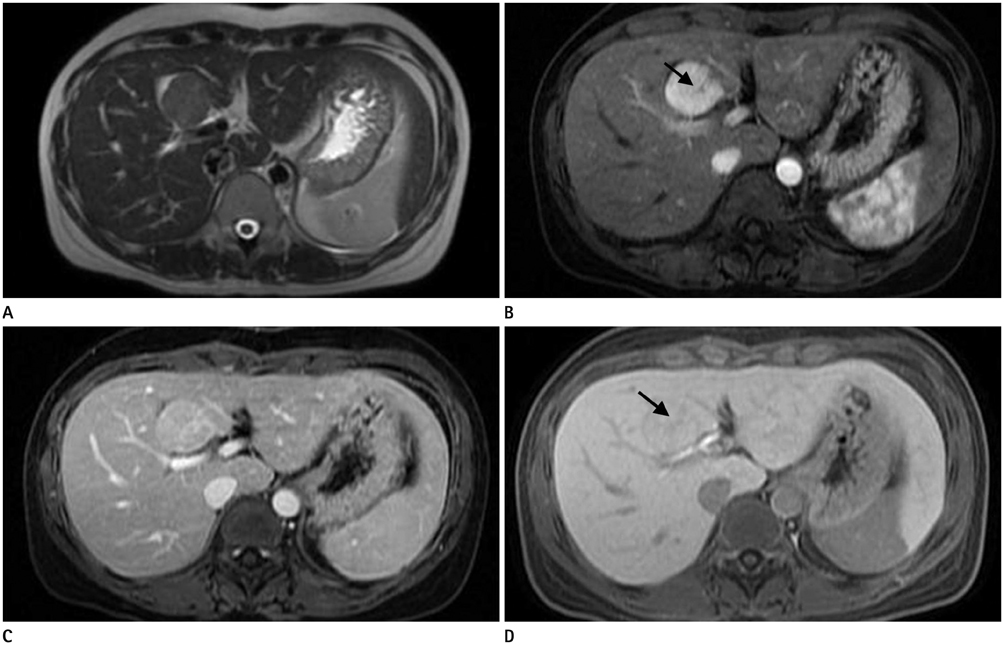
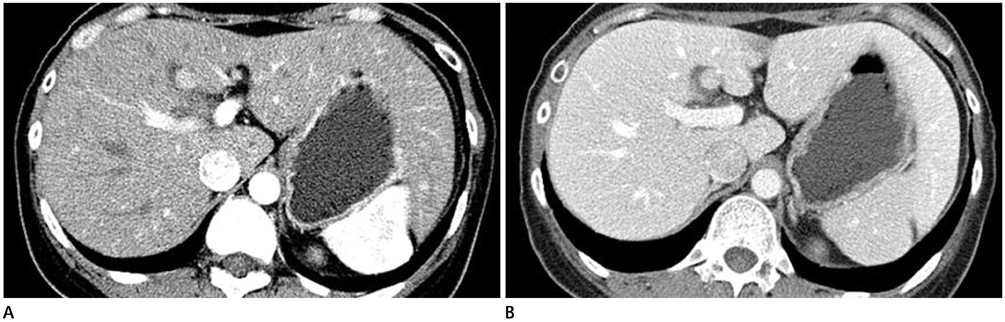
- A focal nodular hyperplasia (FNH) of the liver is the second most common benign hepatic tumor, but an interval growth or regression of FNH is uncommon. We report a case of spontaneous regression of FNH in a 34-year-old woman. This lesion was diagnosed during pregnancy and spontaneously regressed during a 5-year observation period after delivery.
Figure
Reference
-
1. Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985; 5:1194–1200.2. Buetow PC, Pantongrag-Brown L, Buck JL, Ros PR, Goodman ZD. Focal nodular hyperplasia of the liver: radiologic-pathologic correlation. Radiographics. 1996; 16:369–388.3. Côté C. Regression of focal nodular hyperplasia of the liver after oral contraceptive discontinuation. Clin Nucl Med. 1997; 22:587–590.4. Di Stasi M, Caturelli E, De Sio I, Salmi A, Buscarini E, Buscarini L. Natural history of focal nodular hyperplasia of the liver: an ultrasound study. J Clin Ultrasound. 1996; 24:345–350.5. Mathieu D, Kobeiter H, Maison P, Rahmouni A, Cherqui D, Zafrani ES, et al. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology. 2000; 118:560–564.6. Leconte I, Van Beers BE, Lacrosse M, Sempoux C, Jamart J, Materne R, et al. Focal nodular hyperplasia: natural course observed with CT and MRI. J Comput Assist Tomogr. 2000; 24:61–66.7. Giannitrapani L, Soresi M, La Spada E, Cervello M, D'Alessandro N, Montalto G. Sex hormones and risk of liver tumor. Ann N Y Acad Sci. 2006; 1089:228–236.8. Cobey FC, Salem RR. A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management. Am J Surg. 2004; 187:181–191.9. Rifai K, Mix H, Krusche S, Potthoff A, Manns MP, Gebel MJ. No evidence of substantial growth progression or complications of large focal nodular hyperplasia during pregnancy. Scand J Gastroenterol. 2013; 48:88–92.10. Halankar JA, Kim TK, Jang HJ, Khalili K, Masoom HA. Understanding the natural history of focal nodular hyperplasia in the liver with MRI. Indian J Radiol Imaging. 2012; 22:116–120.