Endocrinol Metab.
2013 Mar;28(1):65-69. 10.3803/EnM.2013.28.1.65.
Steroid Responsive Xanthomatous Hypophysitis Associated with Autoimmune Thyroiditis: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. drkuri10@gmail.com
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University of Medicine and Science, Incheon, Korea.
- KMID: 1805949
- DOI: http://doi.org/10.3803/EnM.2013.28.1.65
Abstract
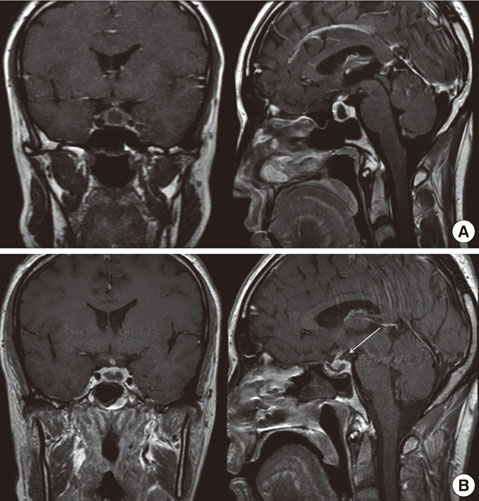
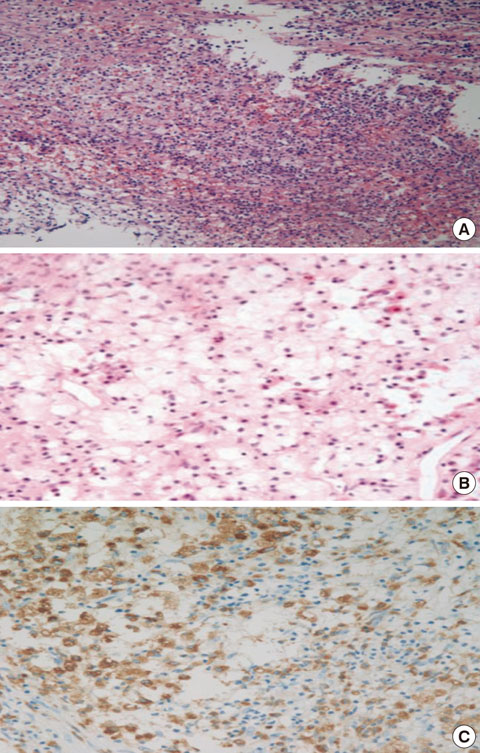
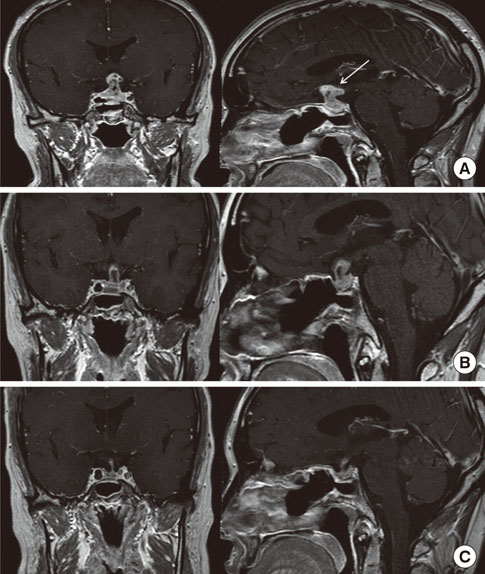
- We report the case of a 36-year-old woman who presented with headache, fever, and amenorrhea. Laboratory analysis revealed hypopituitarism and autoimmune thyroiditis, while a cerebrospinal fluid study suggested concurrent aseptic meningitis. A magnetic resonance image (MRI) scan revealed a 1.0x0.9 cm cystic mass enlarging the sella turcica. Surgical resection via an endoscopic transsphenoidal route was performed. The histological finding of the excised tissue revealed foamy histiocytes with vacuolated cytoplasm, supporting the diagnosis of xanthomatous hypophysitis. Although a residual soft lesion was observed on the MRI image postoperatively, the patient's headache and fever improved. Ten months after surgery, the patient complained of visual impairment and headache, and the residual mass had enlarged into the suprasellar area. High dose (500 mg intravenous) methylprednisolone was administered for 3 days. During the methylprednisolone pulse therapy, the patient's visual acuity and headache improved. A follow-up MRI taken after methylprednisolone therapy showed a marked mass reduction. Our case supports an autoimmune pathophysiology for xanthomatous hypophysitis and suggests that high dose glucocorticoid therapy as a treatment option.
MeSH Terms
Figure
Cited by 2 articles
-
Brief Review of Articles in '
Endocrinology and Metabolism ' in 2013
Won-Young Lee
Endocrinol Metab. 2014;29(3):251-256. doi: 10.3803/EnM.2014.29.3.251.Xanthomatous Hypophysitis Secondary to a Ruptured Rathke’s Cleft Cyst: A Case Report
Emre Gezer, Burak Çabuk, Büşra Yaprak Bayrak, Zeynep Cantürk, Berrin Çetinarslan, Alev Selek, Mehmet Sözen, Damla Köksalan, Savaş Ceylan
Brain Tumor Res Treat. 2022;10(1):48-54. doi: 10.14791/btrt.2022.10.e24.
Reference
-
1. Gutenberg A, Hans V, Puchner MJ, Kreutzer J, Bruck W, Caturegli P, Buchfelder M. Primary hypophysitis: clinical-pathological correlations. Eur J Endocrinol. 2006. 155:101–107.2. Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR. Autoimmune hypophysitis. Endocr Rev. 2005. 26:599–614.3. Tashiro T, Sano T, Xu B, Wakatsuki S, Kagawa N, Nishioka H, Yamada S, Kovacs K. Spectrum of different types of hypophysitis: a clinicopathologic study of hypophysitis in 31 cases. Endocr Pathol. 2002. 13:183–195.4. Cheung CC, Ezzat S, Smyth HS, Asa SL. The spectrum and significance of primary hypophysitis. J Clin Endocrinol Metab. 2001. 86:1048–1053.5. Aste L, Bellinzona M, Meleddu V, Farci G, Manieli C, Godano U. Xanthomatous hypophysitis mimicking a pituitary adenoma: case report and review of the literature. J Oncol. 2010. 2010:195323.6. Burt MG, Morey AL, Turner JJ, Pell M, Sheehy JP, Ho KK. Xanthomatous pituitary lesions: a report of two cases and review of the literature. Pituitary. 2003. 6:161–168.7. Kristof RA, Van Roost D, Klingmuller D, Springer W, Schramm J. Lymphocytic hypophysitis: non-invasive diagnosis and treatment by high dose methylprednisolone pulse therapy? J Neurol Neurosurg Psychiatry. 1999. 67:398–402.8. Leung GK, Lopes MB, Thorner MO, Vance ML, Laws ER Jr. Primary hypophysitis: a single-center experience in 16 cases. J Neurosurg. 2004. 101:262–271.9. de Bruin WI, van 't Verlaat JW, Graamans K, de Bruin TW. Sellar granulomatous mass in a pregnant woman with active Crohn's disease. Neth J Med. 1991. 39:136–141.10. Niyazoglu M, Celik O, Bakkaloglu DV, Oz B, Tanriover N, Gazioglu N, Kadioglu P. Xanthomatous hypophysitis. J Clin Neurosci. 2012. 19:1742–1744.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Xanthomatous Hypophysitis: A Case Report and Literature Review
- Steroid-Responsive Recurrent Encephalopathy Associated with Subacute Thyroiditis
- Association Kikuchi disease with Hashimoto thyroiditis: a case report and literature review
- Lymphocytic Hypophysitis: A Cases Report
- A case of Kikuchi-Fujimoto disease with autoimmune thyroiditis