Pediatr Gastroenterol Hepatol Nutr.
2014 Sep;17(3):170-177. 10.5223/pghn.2014.17.3.170.
Relationship between Anomalous Pancreaticobiliary Ductal Union and Pathologic Inflammation of Bile Duct in Choledochal Cyst
- Affiliations
-
- 1Division of Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. pedks@yuhs.ac
- 2Department of Pediatric Surgery, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1803117
- DOI: http://doi.org/10.5223/pghn.2014.17.3.170
Abstract
- PURPOSE
Choledochal cyst is a cystic dilatation of common bile duct. Although the etiology is presently uncertain, anomalous pancreaticobiliary ductal union (APBDU) is thought to be a major etiology of choledochal cyst. In this study, we analyzed the clinical and anatomical characteristics and pathologies of patients diagnosed with choledochal cyst in a single institute for 25 years.
METHODS
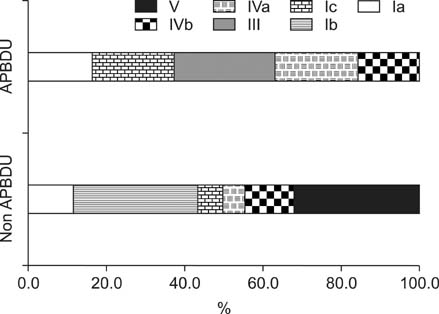
A total of 113 patients, diagnosed with choledochal cyst and who received an operation in Severance Children's Hospital from January 1988 to May 2013, were included. Medical records were reviewed, including clinical and demographic data, surgical procedures. Abdominal ultrasonography, magnetic resonance cholangiopancreatography, and intraoperative cholangiography were used as diagnostic tools for evaluation and classification of choledochal cyst and the presence of anomalous pancreaticobiliary ductal union. Todani's classification, and relationship between APBDU and surgical pathology.
RESULTS
Among 113 patients, 77 patients (68.1%) presented symptoms such as hepatitis, pancreatitis and/or cholecystitis. Eighty three patients (73.5%) had APBDU, and 94 patients (83.2%) showed inflammatory pathologic changes. APBDU, pathologic inflammation, and serological abnormalities such as hepatitis or pancreatitis showed a statistically significant correlation to one another.
CONCLUSION
APBDU is thought to be one of the etiologic factors of choledochal cyst. It is related to the inflammatory changes in bile duct that can lead to the cystic dilatation.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of long-term biliary complications between open and laparoscopic choledochal cyst excision in children
Changhoon Lee, Jeik Byun, Dayoung Ko, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Surg Treat Res. 2021;100(3):186-192. doi: 10.4174/astr.2021.100.3.186.
Reference
-
1. Vater A, Ezler CS. Dissertatio de Scirrhis viscerum occasione sectionis viri tympanite defunte. Wittenburgae. 1723; 881:22.2. Gigot JF, Nagorney DM, Farnell MB, Moir C, Ilstrup D. Bile duct cysts: a changing spectrum of presentation. J Hepatobiliary Pancreat Sci. 1996; 3:405–411.
Article3. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359.
Article4. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269.5. Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg. 1980; 140:653–657.6. Khandelwal C, Anand U, Kumar B, Priyadarshi RN. Diagnosis and management of choledochal cysts. Indian J Surg. 2012; 74:29–34.
Article7. Burnweit CA, Birken GA, Heiss K. The management of choledochal cysts in the newborn. Pediatr Surg Int. 1996; 11:130–133.
Article8. Casaccia G, Bilancioni E, Nahom A, Trucchi A, Aite L, Marcellini M, et al. Cystic anomalies of biliary tree in the fetus: is it possible to make a more specific prenatal diagnosis? J Pediatr Surg. 2002; 37:1191–1194.
Article9. Babbitt DP. Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb. Ann Radiol (Paris). 1969; 12:231–240.10. Tsuchiya R, Harada N, Ito T, Furukawa M, Yoshihiro I. Malignant tumors in choledochal cysts. Ann Surg. 1977; 186:22–28.
Article11. Bismuth H, Krissat J. Choledochal cystic malignancies. Ann Oncol. 1999; 10:Suppl 4. 94–98.
Article12. She WH, Chung HY, Lan LC, Wong KK, Saing H, Tam PK. Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg. 2009; 44:2307–2311.
Article13. Liu CL, Fan ST, Lo CM, Lam CM, Poon RT, Wong J. Choledochal cysts in adults. Arch Surg. 2002; 137:465–468.
Article14. Kumar GCM, Rajagopalan BS. Choledochal cyst. Med J Armed Forces India. 2012; 68:296–298.
Article15. Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg. 2003; 138:333–339.
Article16. Lee HC, Yeung CY, Chang PY, Sheu JC, Wang NL. Dilatation of the biliary tree in children: sonographic diagnosis and its clinical significance. J Ultrasound Med. 2000; 19:177–182.
Article17. Govil S, Justus A, Korah I, Perakath A, Zachariah N, Sen S. Choledochal cysts: evaluation with MR cholangiography. Abdom Imaging. 1998; 23:616–619.
Article18. Chijiiwa K, Koga A. Surgical management and long-term follow-up of patients with choledochal cysts. Am J Surg. 1993; 165:238–242.
Article19. Pietrabissa A, Boggi U, Di Candio G, Giulianotti PC, Sartoni G, Mosca F. Unsuspected choledochal cyst during laparoscopic cholecystectomy. Surg Endosc. 1995; 9:1127–1129.
Article20. Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 2 of 3: diagnosis. Can J Surg. 2009; 52:506–511.21. Yamashiro Y, Sato M, Shimizu T, Oguchi S, Miyano T. How great is the incidence of truly congenital common bile duct dilatation? J Pediatr Surg. 1993; 28:622–625.
Article22. Kamisawa T, Ando H, Hamada Y, Fujii H, Koshinaga T, Urushihara N, et al. Japanese Study Group on Pancreaticobiliary Maljunction. Diagnostic criteria for pancreaticobiliary maljunction 2013. J Hepatobiliary Pancreat Sci. 2014; 21:159–161.
Article23. Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997; 32:1735–1738.
Article24. Babbitt DP, Starshak RJ, Clemett AR. Choledochal cyst: a concept of etiology. Am J Roentgenol Radium Ther Nucl Med. 1973; 119:57–62.
Article25. O'Neill JA Jr, Templeton JM Jr, Schnaufer L, Bishop HC, Ziegler MM, Ross AJ 3rd. Recent experience with choledochal cyst. Ann Surg. 1987; 205:533–540.26. Sela-Herman S, Scharschmidt BF. Choledochal cyst, a disease for all ages. Lancet. 1996; 347:779.
Article27. Alonso-Lej F, Rever WB Jr, Pessango DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg. 1959; 108:1–30.28. Büyükyavuz I, Ekinci S, Ciftçi AO, Karnak I, Senocak ME, Tanyel FC, et al. A retrospective study of choledochal cyst: clinical presentation, diagnosis and treatment. Turk J Pediatr. 2003; 45:321–325.29. Song HK, Kim MH, Myung SJ, Lee SK, Kim HJ, Yoo KS, et al. Choledochal cyst associated the with anomalous union of pancreaticobiliary duct (AUPBD) has a more grave clinical course than choledochal cyst alone. Korean J Intern Med. 1999; 14:1–8.
Article30. Oguchi Y, Okada A, Nakamura T, Okumura K, Miyata M, Nakao K, et al. Histopathologic studies of congenital dilatation of the bile duct as related to an anomalous junction of the pancreaticobiliary ductal system: clinical and experimental studies. Surgery. 1988; 103:168–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preemptive resection of choledochal cyst during redo resection of gallbladder cancer following laparoscopic cholecystectomy
- A Case of Choledochal Cyst with Anomalous Pancreaticobiliary Ductal Union
- Choledochal Cyst and Anomalous Union of Pancreaticobiliary Duct in the Adult
- A woman in her twenties with gallbladder cancer associated with an anomalous union of the pancreaticobiliary duct
- Gallbladder Cancer Associated with an Anomalous Union of the Pancreaticobiliary Duct and a Choledochal Cyst